“What you are asking is not what we are told to prepare’’: A communitybased study of Birth preparedness and complication readiness among postpartum women in a rural district, northern Tanzania
Article Information
Minael G. Mjemmas1†*, Edwin J. Shewiyo1†, Ester J. Diarz2,3, Patricia Swai4, Beatrice J. Leyaro2, Sia E. Msuya1,2,5
Affiliation:
1Institute of Public Health, Department of Community Health, Kilimanjaro Christian Medical University College, Moshi, Tanzania
2Institute of Public Health, Department of Epidemiology & Biostatistics, Kilimanjaro Christian Medical University College, Moshi, Tanzania
3National Institute for Medical Research (NIMR), Muhimbili Medical Research Centre (MMRC), Dar es salaam, Tanzania
4Department of Obstetrics and Gynecology, Kilimanjaro Christian Medical Centre (KCMC), Moshi, Tanzania
5Department of Community Medicine, Kilimanjaro Christian Medical Centre (KCMC), Moshi, Tanzania
†Equal authorship
*Corresponding author:Minael G. Mjemmas, KCMUCo, Po Box 2240, Moshi Tanzania.
Received: March 04, 2023; Accepted: March 20, 2023; Published: April 11, 2023
Citation: Minael G. Mjemmas, Edwin J. Shewiyo, Ester J. Diarz, Patricia Swai, Beatrice J. Leyaro, Sia E. Msuya. “What you are asking is not what we are told to prepare’’: a community-based study of Birth preparedness and complication readiness among postpartum women in a rural district, northern Tanzania. Obstetrics and Gynecology Research. 6 (2023): 115-121
Share at FacebookAbstract
Background:
This study aimed to assess knowledge and practice of birth preparedness and complication readiness among women in a rural district, northern Tanzania.
Methods:
A community-based, cross-sectional study was conducted in July 2019, among women who delivered in the 24 months prior to the study. A validated maternal neonatal program JHPIEGO tool was translated, modified and used for data collection through face-to-face interviews. Results:
A total of 372 women participated; the mean age was 28.5 (S.D 7.1) years. Among these, 93.3% reported they were counseled on BPCR plan. A majority (96%) were counseled to prepare birth materials, 26.9% to prepare money, 13.2% counseled to prepare transport and 1.1% informed on choosing birth attendant. (95.7%) prepared birth materials (clothes, gloves), 30.1% prepared money, 8.1% prepared transport and 2.7% prepared blood donors. Only 13.7% of the women prepared ≥3 components of BPCR plan. Counseling for danger signs during pregnancy was associated with having a BPCR plan (p= 0.003). Preparing ≥3 components was significantly associated with postnatal care use (p=0.005), but not with 4+ ANC visits (p = 0.875) or SBA use (p=0.057).
Conclusion:
Women are counseled on birth preparedness but not on components that can save lives in case of complications. The need to change counseling on birth preparedness plan is required.
Keywords
Prevalence, birth preparedness and complication readiness, BPCR, counseling, childbirth, danger signs, Tanzania
Prevalence articles Prevalence Research articles Prevalence review articles Prevalence PubMed articles Prevalence PubMed Central articles Prevalence 2023 articles Prevalence 2024 articles Prevalence Scopus articles Prevalence impact factor journals Prevalence Scopus journals Prevalence PubMed journals Prevalence medical journals Prevalence free journals Prevalence best journals Prevalence top journals Prevalence free medical journals Prevalence famous journals Prevalence Google Scholar indexed journals birth preparedness and complication readiness articles birth preparedness and complication readiness Research articles birth preparedness and complication readiness review articles birth preparedness and complication readiness PubMed articles birth preparedness and complication readiness PubMed Central articles birth preparedness and complication readiness 2023 articles birth preparedness and complication readiness 2024 articles birth preparedness and complication readiness Scopus articles birth preparedness and complication readiness impact factor journals birth preparedness and complication readiness Scopus journals birth preparedness and complication readiness PubMed journals birth preparedness and complication readiness medical journals birth preparedness and complication readiness free journals birth preparedness and complication readiness best journals birth preparedness and complication readiness top journals birth preparedness and complication readiness free medical journals birth preparedness and complication readiness famous journals birth preparedness and complication readiness Google Scholar indexed journals counseling articles counseling Research articles counseling review articles counseling PubMed articles counseling PubMed Central articles counseling 2023 articles counseling 2024 articles counseling Scopus articles counseling impact factor journals counseling Scopus journals counseling PubMed journals counseling medical journals counseling free journals counseling best journals counseling top journals counseling free medical journals counseling famous journals counseling Google Scholar indexed journals danger signs articles danger signs Research articles danger signs review articles danger signs PubMed articles danger signs PubMed Central articles danger signs 2023 articles danger signs 2024 articles danger signs Scopus articles danger signs impact factor journals danger signs Scopus journals danger signs PubMed journals danger signs medical journals danger signs free journals danger signs best journals danger signs top journals danger signs free medical journals danger signs famous journals danger signs Google Scholar indexed journals Tanzania articles Tanzania Research articles Tanzania review articles Tanzania PubMed articles Tanzania PubMed Central articles Tanzania 2023 articles Tanzania 2024 articles Tanzania Scopus articles Tanzania impact factor journals Tanzania Scopus journals Tanzania PubMed journals Tanzania medical journals Tanzania free journals Tanzania best journals Tanzania top journals Tanzania free medical journals Tanzania famous journals Tanzania Google Scholar indexed journals maternal deaths articles maternal deaths Research articles maternal deaths review articles maternal deaths PubMed articles maternal deaths PubMed Central articles maternal deaths 2023 articles maternal deaths 2024 articles maternal deaths Scopus articles maternal deaths impact factor journals maternal deaths Scopus journals maternal deaths PubMed journals maternal deaths medical journals maternal deaths free journals maternal deaths best journals maternal deaths top journals maternal deaths free medical journals maternal deaths famous journals maternal deaths Google Scholar indexed journals maternal mortality articles maternal mortality Research articles maternal mortality review articles maternal mortality PubMed articles maternal mortality PubMed Central articles maternal mortality 2023 articles maternal mortality 2024 articles maternal mortality Scopus articles maternal mortality impact factor journals maternal mortality Scopus journals maternal mortality PubMed journals maternal mortality medical journals maternal mortality free journals maternal mortality best journals maternal mortality top journals maternal mortality free medical journals maternal mortality famous journals maternal mortality Google Scholar indexed journals Live births articles Live births Research articles Live births review articles Live births PubMed articles Live births PubMed Central articles Live births 2023 articles Live births 2024 articles Live births Scopus articles Live births impact factor journals Live births Scopus journals Live births PubMed journals Live births medical journals Live births free journals Live births best journals Live births top journals Live births free medical journals Live births famous journals Live births Google Scholar indexed journals pregnant women articles pregnant women Research articles pregnant women review articles pregnant women PubMed articles pregnant women PubMed Central articles pregnant women 2023 articles pregnant women 2024 articles pregnant women Scopus articles pregnant women impact factor journals pregnant women Scopus journals pregnant women PubMed journals pregnant women medical journals pregnant women free journals pregnant women best journals pregnant women top journals pregnant women free medical journals pregnant women famous journals pregnant women Google Scholar indexed journals birth materials articles birth materials Research articles birth materials review articles birth materials PubMed articles birth materials PubMed Central articles birth materials 2023 articles birth materials 2024 articles birth materials Scopus articles birth materials impact factor journals birth materials Scopus journals birth materials PubMed journals birth materials medical journals birth materials free journals birth materials best journals birth materials top journals birth materials free medical journals birth materials famous journals birth materials Google Scholar indexed journals
Article Details
Introduction
Globally 814 women die every day from preventable causes of death following pregnancy and childbirth. Sub Saharan Africa contributes 86% of the global maternal deaths. Obstetric complications account for 75% of the maternal deaths. Majority of these deaths occur in low- and middle-income countries of which 94% are preventable (Say et al., 2014; World Health Organization, 2022). In Tanzania maternal mortality remains high at 524 per 100,000 live births as of 2021 (Ministry of Health et al., 2016; Limenih, Belay and Tassew, 2019; World Bank, 2022). The use of skilled birth attendants during delivery and delivering at health facilities is among the indicators towards reducing maternal deaths by 2030 according to SDG 3.1, SBA coverage in Tanzania is increasing but remains lower than the global target at
65% as of 2016 (United Nations, 2015; L et al., 2016; World Health Organization, 2016; Orwa et al., 2020).
Birth Preparedness and Complications Readiness (BPCR) is among the interventions recommended by WHO to promote the increase of use of skilled birth attendants and health facilities during delivery(World Health Organization, 2015; Solnes Miltenburg et al., 2017; Obionu, Ajuba and Aguwa, 2022). BPCR plan involves several items that mothers have to prepare including the desired place of birth, the preferred birth attendant, the location of the closest facility for birth , funds for any expenses related to birth; supplies and materials necessary to bring to the facility, an identified labor and birth companion, an identified support to look after at home and other children (if present) while the woman is away, transport to a facility for birth and identification of compatible blood donors in case of complications (Solnes Miltenburg et al., 2017; Smeele et al., 2018; Shimpuku et al., 2021).
There is limited information on BPCR knowledge and practice among women in Tanzania. The demographic health survey shows that despite 84.8% of women are being informed about BPCR during ANC visits during pregnancy, only 58.2% were prepared for birth and its complications. This low practice is similar to studies done in countries such as Kenya , Rwanda , Nigeria and Ethiopia (Smeele et al., 2018; Limenih, Belay and Tassew, 2019; Orwa et al., 2020; Obionu, Ajuba and Aguwa, 2022). Furthermore, pregnant women in urban areas perform the recommended ANC visits compared to rural settings hence even maternal mortality is higher in rural than in urban areas. (Ministry of Health et al., 2016; Obionu, Ajuba and Aguwa, 2022). Based on these findings we hypothesize that women in rural Manyara are not fully informed about BPCR during pregnancy and do not have a BPCR plan during pregnancy. We aim to assess the training and practice of BPCR among women in a rural, Manyara, Northern Tanzania and furthermore to analyze the association of BPCR planning and the use of services among women.
Subjects and Methods
Study Design and study site
This was a community based cross-sectional study conducted in 2019 at a rural district, in Manyara region, Northern Tanzania.
Study population and Sampling
The study population was 422 women who gave birth in the past 24 months prior to the study. Random sampling was used from district level to household level of which 2 wards out of 25 wards in the district and 70 households were selected.
Data collection tool and methods:
A standard validated Maternal and Neonatal health
JHPIEGO questionnaire tool was used to collect data from participants (JHPIEGO, 2004). The questionnaire was translated to Swahili and pilot tested before data collection. The questionnaire was semi-structured contained open and closed ended questions and had four sections which included the socio- demographic characteristics of the participants, reproductive and maternal health characteristics of the participants, counselling on birth preparedness and the history of the birth preparedness plan of the participants during the last pregnancy. Face to face interviews were used to collect data from participants with pre-trained interviewee team. The interviews lasted about 15-30 minutes on average.
Study Variables
Dependent variables is Birth preparedness and complication readiness. Independent variables are birth materials, money for delivery, person to stay with children, transport, and place of delivery, blood donor and choosing skilled birth attendant.
Operational Definition of Variables
Women were categorized as well prepared if they prepared three or more components and not well prepared if they prepared less than three components. The term “birth materials” referred to the following items birth clothing (khangas or kitenge a cloth used to wrap the baby), wash basin (beseni), baby clothes, hat, sanitary towels (pads), makintosh (bed cover), gloves, sharps (wembe) and sometimes sutures.
Data analysis
Difference between groups and outcome variables (categorical) was first assessed using Chi-square test. In bivariate analysis, Odds Ratio with their 95% confidence interval were calculated to assess the strength of association between having a BPCR plan with socio-demographic, reproductive and maternal health characteristics.
Ethical considerations
The Research Ethical Committee at the Kilimanjaro Medical University approved the study. Permission to conduct the study at the rural communities of Manyara was granted by the District Medical Officer. The informed consent from the participant included a description of the purpose of the study, benefits, risks, right to refusal, also confidentiality and privacy was insured. We obtained a signed consent and a right thumb print for an illiterate participant.
Results
Response rate
A total of 422 women were approached but only 372 women agreed to be enrolled in the study, hence 88.1% was the participation proportion. The reasons for refusal to provide participation to the study regardless after the explanation of the benefit of the study to the participants was lack of interest to provide their personal information, busy with household activities and taking care of babies, being in a rush to go to their daily activities.
Socio-demographic characteristics of the participants
The mean age of the 372 participants was 28.5 (S.D 7.1) years. The majority of the 372 participants were in union (86.6%), had no and/or primary education (80.1%), and were unemployed (69.1%), with 82.3% not able to estimate their income per month, Table 1. Nearly half (49%) of the women walked for < 30 minutes to reach the nearest health facility with reproductive and child health (RCH) services, and (67%) use motorcycle and/ or tricycle as common mode of transport during labor.
Reproductive and maternal health characteristics of the participants
The median parity of the 372 women was 3 (IQR 2-4). All the women attended for ANC visit at least once during last pregnancy, but 68.3% had first ANC visit at >12 weeks of gestation and 65.3%attended for four or more visits. The majority of the 372 women (70%) reported to have been counseled on danger signs of obstetric emergency during pregnancy and 85% delivered their last baby at the health facility (Table 2).
Counseling on birth preparedness
Of the 372 women, 93.3% reported to have been counseled on birth preparedness and complication readiness plan. Figure 1, shows proportion of each component that the women reported they were counseled to prepare. Majority of the women (96%) reported that they were informed to prepare several things like; child clothes, khanga or kitenge to wrap the baby when born, hat, basin to wash the baby, gloves, mackintosh to put on the bed during delivery and pads. Nearly a third (26.9%) of the women were informed to prepare money, 13% to prepare for transport and 1.1% were informed to prepare the skilled birth attendant (SBA) of their choice, (Figure 1).
Proportion of women who had BPCR plan
Most of the women prepared birth materials (like khanga, child clothes, hat, wash basin for the child and gloves) before delivery (95.7%); 30.1% prepared money, 15.1% prepared a person to take care of children when the woman is at the facility during delivery and 8.1% prepared for transport (Figure 2). No woman among the participants chose a birth attendant during delivery. Many women commented that “what you asking us on birth preparedness is not what we are told to prepare. During ANC most of the time the health providers insist to prepare baby things like gloves, clothes, what to wrap the baby once he/she is born, hat, wash basin and pads”.
Of the 112 who prepared money; the median amount of money prepared was 50,000 Tanzanian shillings (IQR 30,000
– 100,000).
Of the 372 women, only 51 (13.7%) had prepared three or more components of BPCR plan, and were therefore classified as being well prepared for birth and for complications that may arise during pregnancy and/or at delivery. Figure 2;
Factors associated with being well prepared for birth and complications and its effect on maternal health service use
Bi-variate analysis was done to assess factors associated with being well prepared for birth and complications. Women aged 25-34 years had 2 times higher odds of having a well
Table 1: Background characteristics of the 372 women in a rural district, Manyara, Northern Tanzania
|
Variables |
Frequency |
% |
|
Age (years) |
||
|
< 20 |
20 |
5.4 |
|
20 – 29 |
210 |
56.5 |
|
30 – 39 |
105 |
28.2 |
|
40 –49 |
37 |
9.9 |
|
Marital status |
||
|
In union (married/cohabiting) |
322 |
86.6 |
|
Not union (single/ divorced) |
50 |
13.4 |
|
Education level |
||
|
None/ primary |
298 |
80.1 |
|
Secondary and above |
74 |
19.9 |
|
Employment status |
||
|
Formal employed |
9 |
2.4 |
|
Self employed |
106 |
28.5 |
|
Unemployed |
257 |
69.1 |
|
Income of women per month (TZS)* |
||
|
<70,000 |
50 |
13.4 |
|
>70,000 |
16 |
4.3 |
|
Don’t know |
306 |
82.3 |
|
Level of nearest health facility with RCH services |
||
|
Dispensary |
67 |
18 |
|
Health centre |
199 |
53.5 |
|
Hospital |
106 |
28.5 |
|
Time to nearest health facility with RCH (walking) |
||
|
Up to 30 minutes |
181 |
48.7 |
|
31 – 60 minutes |
107 |
28.8 |
|
61 – 180 minutes |
84 |
22.5 |
|
Mode of transport used by women during delivery (reported) |
||
|
Walking |
54 |
14.5 |
|
Motorcycle/ Tricycle |
249 |
66.9 |
|
Car/Tax |
103 |
18.6 |
* 1 USD = 2,280 TZS during data collection
Table 2: Reproductive and maternal health characteristics of the 372 women in a rural district, Manyara, Northern Tanzania
|
Variable |
Frequency |
% |
|
Parity |
||
|
1 |
89 |
23.9 |
|
2-3 |
155 |
41.7 |
|
4+ |
128 |
34.4 |
|
Number of living children |
||
|
0-3 |
256 |
68.8 |
|
4+ |
116 |
31.2 |
|
GA when started ANC at last pregnancy |
||
|
≤ 12 weeks |
118 |
31.7 |
|
13 – 27 weeks |
215 |
57.8 |
|
28+ weeks |
39 |
10.5 |
|
Frequency of ANC visit at last pregnancy |
||
|
1-3 |
129 |
34.7 |
|
4 |
126 |
33.9 |
|
5-9 |
117 |
31.5 |
|
Place of delivery of last child |
||
|
Healthy facility |
316 |
84.9 |
|
Home/ on the way (BBA) |
56 |
15.1 |
|
Birth Assistant at last delivery |
||
|
Health care provider |
317 |
85.2 |
|
TBA/relative/ mother-in-law |
50 |
13.4 |
|
Self-delivery |
5 |
1.3 |
|
Attended ANC with a partner |
||
|
No |
139 |
37.4 |
|
Yes |
233 |
62.6 |
|
Counseled on danger signs during pregnancy |
||
|
No |
100 |
26.9 |
|
Yes |
272 |
73.1 |
|
Counseled on danger signs before discharge (N = 316) |
||
|
No |
148 |
46.8 |
|
Yes |
168 |
53.2 |
|
Well prepared (prepared 3+ components of BPCR plan) |
||
|
No |
321 |
86.3 |
|
Yes |
51 |
13.7 |
BPCR plan than those aged 15-24 years (OR 2.33 [95% CI: 1.14-4.79]). All the socio-demographic factors (education, marital status, income, partner attendance at ANC) were not associated with having three or more components of the BPCR plan, Table 3. Of the facility, reproductive and maternal health factors, the level of facility where women received ANC care (p < 0.001) and report of being counseled for danger sign during antenatal care (p=0.003) were significantly associated with being well prepared with BPCR plan (Table
3). A higher proportion of women who were counseled for danger signs of obstetric emergency had BPCR plan (16.9%) compared to those who were not counseled (5.0%), [OR 3.87; (95% CI: 1.49 – 10.04)]. The 95% confidence interval for both (level of facility and counseled for DS) were wide. In logistic regression analysis level of facility where the woman received ANC and counseling on danger signs during ANC remained associated with having a BPCR plan being well prepared for birth was not significantly associated with four or more ANC visits [OR 1.07; (95% CI: 0.57 – 2.01)] or with skilled birth attendance use during delivery [OR 3.09; (95% CI: 0.93 – 10.31)]. It was however associated with postnatal care utilization within 42 days after delivery [2.39; (95% CI: 1.31 – 4.36)]. Table 3.
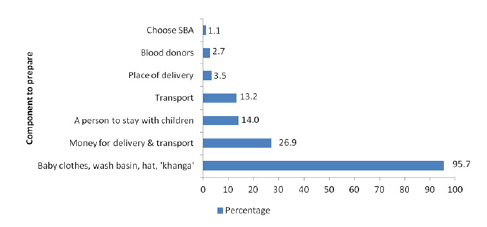
Figure 1: Proportion of women who were counseled on each component of birth preparedness and complication readiness plan at a rural district, Manyara, northern Tanzania (N = 372)
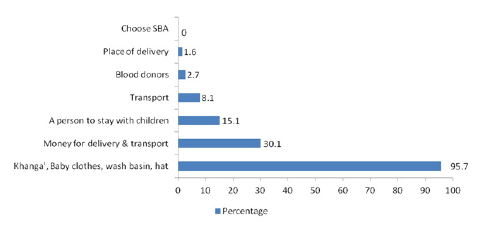
Figure 2: Proportion of women who had Birth Preparedness and Complication Readiness Plan in a rural district, Manyara, Northern Tanzania (N=372)
Discussion
In this study (93.3%) of women were counseled on birth preparedness whereby (96%)were informed on preparing birth materials before delivery and less than 3% of women were informed on choosing facility for delivery, birth attendant and blood donors. This resulted in a majority (95.7%) of women prepared materials for birth before delivery and those who prepared facility for delivery, birth attendant and blood donors were less than (5%). This is similar to study done in Southeast Nigeria where 94.1% of the women prepared birth materials as instructed (Onoh et al., 2020). This implies that women prepare accordingly to what they are informed with emphasis from the counseling by health providers. Thus,
Table 3: Factors associated with having a birth preparedness and complication readiness plan in a rural district, Manyara, Northern Tanzania
|
Variable |
Had a BPCR plan |
Association with BPCR plan |
||
|
N |
n (%) |
COR (95%CI) |
AOR (95%CI) |
|
|
Predictors |
||||
|
Age of woman (years) |
||||
|
15-24 |
139 |
12 (8.6) |
1 |
1 |
|
25-34 |
155 |
28 (18.1) |
2.33 (1.14 – 4.79) * |
1.70 (0.77 – 3.77) |
|
35-49 |
78 |
11 (14.1) |
1.74 (0.73 – 4.15) |
1.15 (0.43 – 3.02) |
|
Education level |
||||
|
None/primary |
298 |
41 (13.8) |
1 |
|
|
Secondary and above 74 |
10 (13.5) |
0.98 (0.47 – 2.06) |
||
|
Marital status |
||||
|
Not in union |
50 |
4 (8.0) |
1 |
|
|
In union |
322 |
47 (14.6) |
1.97 (0.68 – 5.72) |
|
|
Income per month (TZS) |
||||
|
< 70,000 |
50 |
5 (10.0) |
1 |
|
|
>70,000 |
16 |
4 (25.0) |
3.00 (0.70 – 12.90) |
|
|
Don’t know |
306 |
42 (13.7) |
1.43 (0.54 – 3.81) |
|
|
Time to nearest facility (walking) |
||||
|
Up to 60 minutes |
288 |
35 (12.2) |
1 |
|
|
61 – 180 minutes |
84 |
16 (19.0) |
1.71 (0.89 – 3.26) |
|
|
Level of facility received ANC |
||||
|
Hospital |
121 |
4 (3.3) |
1 |
1 |
|
Health Centre |
197 |
38 (19.3) |
6.99 (2.43 – 20.10) *** |
6.83 (2.20 – 18.56) *** |
|
Dispensary |
54 |
9 (16.7) |
5.85 (1.72 – 20.00) ** |
5.52 (1.59 – 19.16) ** |
|
Partner attended ANC |
||||
|
No |
139 |
17 (12.2) |
1 |
|
|
Yes |
233 |
34 (14.6) |
1.23 (0.66 – 2.29) |
|
|
Parity |
||||
|
1 |
89 |
7 (7.9) |
1 |
1 |
|
2+ |
283 |
44 (15.5) |
2.16 (0.94 – 4.98) |
1.74 (0.67 – 4.49) |
|
GA when started ANC at last pregnancy |
||||
|
≤ 12 weeks |
118 |
21 (17.8) |
1 |
|
|
13+ weeks |
254 |
30 (11.8) |
0.62 (0.34 – 1.13) |
|
|
Informed on danger signs during ANC |
||||
|
No |
100 |
5 (5.0) |
1 |
1 |
|
Yes |
272 |
46 (16.9) |
3.87 (1.49 – 10.04) * |
3.47 (1.32 – 9.17) * |
*p-value <0.05; ** p-value<0.01; *** p-value<0.001COR: Crude Odds Ratio; AOR: Adjusted Odds Ratio women are not well informed about all components of BPCR and more emphasis is put on certain components of BPCR such as birth materials, resulting in a lower proportion of women who are well prepared for birth and its complications. Hence, interventions are required to improve counseling on BPCR.
Overall 13.7% of women were well prepared for birth and its complications, this proportion is lower than in studies done in rural Rwanda 22.3% , Nigeria 25.7% and Ethiopia 34% (Smeele et al., 2018; Limenih, Belay and Tassew, 2019; Obionu, Ajuba and Aguwa, 2022). This might be due to the differences in study settings and level of literacy among women in the areas. The low proportion of women who were well prepared implies that there is still work to be done to increase Birth preparedness in some of the regions in Tanzania, a study done in central Tanzania showed majority (86.2%) of women were well prepared for birth and its complications (11) but this is not the case in other parts of Tanzania such as Manyara. More interventions are required to improve BPCR coverage throughout the country.
In our study having middle age of 25-34 among women was found to be an important factor associated with being well prepared for birth than those aged <25 years and >35 years of age. This is similar to study done in Nigeria which also found participants aged 25-29 are associated with being well prepared for birth. Although this is different to study done in in Southern Ethiopia a community based study that showed having a young age of 15-24 was more likely to be prepared for birth than others. This difference may be due to age between 25-34 years tends to have experienced previous pregnancies hence more aware of complications that can arise and be encountered during pregnancy, delivery and even after delivery. Also women aged above 35 years of aged tend to believe can deliver safely without assistance of health professional since they belong to traditional era when most women delivered without skilled birth assistants because of lack of health facilities. This finding stresses the importance of improved training for health providers on how to better communicate BPCR related messages with antenatal care attendants (Azeze, Mokonnon and Kercho, 2019; Onoh et al., 2020).
Moreover, being counseled for danger sign was associated with being well prepared with BPCR plan. Women who were counseled for danger signs of obstetric emergency had 3.87 times higher odds to have a BPCR plan compared to the women who were not counseled, This was similar to other studies done in Rwanda Ethiopia, and Kenya (Smeele et al., 2018; Limenih, Belay and Tassew, 2019; Orwa et al., 2020). This further stresses the importance of proper counseling of women during Antenatal Clinic to help them prepare for birth and its complications. There is a need to improve the quality of counseling in Antenatal Clinic to ensure that women are given the right information and furthermore supporting strategies such as house to house teachings and focus group discussions serving as a reminder to pregnant women to maintain flow of information.
In this study the level of education, marital status and parity was found to have no association with women being well prepared for birth. This is different from other studies done in Kenya ,Tanzania , Rwanda , Nigeria and Ethiopia (Smeele et al., 2018; Limenih, Belay and Tassew, 2019; Onoh et al., 2020; Orwa et al., 2020). The difference may be due to study settings, type of study conducted and number of participants involved in the study.
Consent to publish:
Not applicable, the manuscript does not contain any individual personal data.
Competing interests:
The authors declare that they have no competing interests.
Funding
The funding in this study was partially sponsored by Higher Education Students Loans Board and by the DELTAS Africa Initiative grant. The funders did not have any role or influence the design of the study, data collection, analysis or interpretation of the results and in development of the manuscript.
Authors’ contributions
MGM, EJS, BJL and SEM contributed to the design of the study. EJS, MGM collected the data. MGM, EJS, EJD and SEM analyzed the data. MGM, EJS, EJD, BJL, PS and SEM interpreted the results. MGM, EJS and EJD prepared the manuscript and all the other authors reviewed the manuscript critical input before submission. All authors read and approved the final manuscript.
Acknowledgements
We extend our gratitude to the women who enrolled in the study, the district medical officer, and the community health workers who facilitated the study.
References
- Azeze, G.A., Mokonnon, T.M. and Kercho, M.W. (2019) ‘Birth preparedness and complication readiness practice and influencing factors among women in Sodo town, Wolaita zone, Southern Ethiopia, 2018; community based cross-sectional study’, Reproductive Health, 16(1), 39.
- JHPIEGO (2004) ‘Monitoring Birth Preparedness and Complication Readiness tools and indicators for maternal and newborn health.’, FAMILY CARE [Preprint].
- L, A. et al. (2016) ‘Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter- Agency Group’, Lancet (London, England), 387(10017).
- Limenih, M.A., Belay, H.G. and Tassew, H.A. (2019) ‘Birth preparedness, readiness planning and associated factors among mothers in Farta district, Ethiopia: a cross- sectional study’, BMC pregnancy and childbirth, 19(1), 171.
- Ministry of Health, D. et al. (2016) ‘Tanzania Demographic and Health Survey and Malaria Indicator Survey 2015-2016’.
- Obionu, M., Ajuba, M. and Aguwa, E.N. (2022) ‘Preparation for birth and complication readiness: rural- urban disparities among pregnant women in communities in Enugu State, Nigeria’, The Pan African Medical Journal, 42, p. 310.
- Onoh, C. et al. (2020) ‘Birth preparedness and complication readiness among women of reproductive age group in Abakaliki, Southeast Nigeria’, Nigerian Journal of Clinical Practice, 23(3), pp. 362–370.
- Orwa, et al. (2020) ‘Birth preparedness and complication readiness among women of reproductive age in Kenya and Tanzania: a community-based cross-sectional survey’, BMC pregnancy and childbirth, 20(1), p. 636.
- Say, L. et al. (2014) ‘Global causes of maternal death: a WHO systematic analysis’, The Lancet. Global Health, 2(6), pp. e323-333.
- Shimpuku, et al. (2021) ‘Birth preparedness and related factors: a cross-sectional study in Tanzania City area’, BMC Health Services Research, 21, p. 818.
- Smeele, et al. (2018) ‘Birth preparedness and complication readiness among pregnant women admitted in a rural hospital in Rwanda’, BMC Pregnancy and Childbirth, 18, p. 190.
- Solnes Miltenburg, A. et al. (2017) ‘Factors influencing implementation of interventions to promote birth preparedness and complication readiness’, BMC pregnancy and childbirth, 17(1), p. 270.
- United Nations (2015) Sustainable Development Goals. Goal 3. Indicator and Targets | Department of Economic and Social
- World Bank (2022) Maternal mortality ratio (modeled estimate, per 100,000 live births) - Tanzania |
- World Health Organization (2015) WHO recommendations on health promotion interventions for maternal and newborn health World Health Organization.
- World Health Organization (2016) Births attended by skilled health personnel.
- World Health Organization (2022) Maternal
