Uterine Artery Embolisation for Acquired Uterine Arteriovenous Malformation- A Case Report
Article Information
Tejdeep Singh1*, Richa2, Ankith N Swamy3, Sreehari C.S4, Subhash Kumar5
1Junior Resident, Radiodiagnosis, All India Institute of Medical Sciences, Patna, India
2Senior Resident, Radiodiagnosis, All India Institute of Medical Sciences, Patna, India
3Junior Resident, Radiodiagnosis, All India Institute of Medical Sciences, Patna, India
4Junior Resident, Radiodiagnosis, All India Institute of Medical Sciences, Patna, India
5Additional Professor, Radiodiagnosis, All India Institute of Medical Sciences, Patna, India
*Corresponding Author: Tejdeep Singh, Junior Resident, Radiodiagnosis, All India Institute of Medical Sciences, Patna, India
Received: 19 October 2020; Accepted: 30 November 2020; Published: 22 December 2020
Citation: Tejdeep Singh, Richa, Ankith N Swamy, Sreehari C.S, Subhash Kumar. Uterine Artery Embolisation for Acquired Uterine Arteriovenous Malformation- A Case Report. Journal of Radiology and Clinical Imaging 3 (2020): 110-115.
Share at FacebookAbstract
Uterine arteriovenous malformations (AVMs) are the rare but potentially life-threatening cause of uterine artery bleeding. We report a case of acquired uterine AVM following dilatation and curettage (D&C) that was successfully treated with bilateral uterine artery embolization using 20% lipiodol- nBCA (N-butyl cyanoacrylate) mixture as an embolizing agent.
Keywords
Uterine arteriovenous malformations; Uterine artery bleeding; Congenital; Uterine malformations
Uterine arteriovenous malformations articles; Uterine artery bleeding articles; Congenital articles; Uterine malformations articles
Uterine arteriovenous malformations articles Uterine arteriovenous malformations Research articles Uterine arteriovenous malformations review articles Uterine arteriovenous malformations PubMed articles Uterine arteriovenous malformations PubMed Central articles Uterine arteriovenous malformations 2023 articles Uterine arteriovenous malformations 2024 articles Uterine arteriovenous malformations Scopus articles Uterine arteriovenous malformations impact factor journals Uterine arteriovenous malformations Scopus journals Uterine arteriovenous malformations PubMed journals Uterine arteriovenous malformations medical journals Uterine arteriovenous malformations free journals Uterine arteriovenous malformations best journals Uterine arteriovenous malformations top journals Uterine arteriovenous malformations free medical journals Uterine arteriovenous malformations famous journals Uterine arteriovenous malformations Google Scholar indexed journals Uterine artery bleeding articles Uterine artery bleeding Research articles Uterine artery bleeding review articles Uterine artery bleeding PubMed articles Uterine artery bleeding PubMed Central articles Uterine artery bleeding 2023 articles Uterine artery bleeding 2024 articles Uterine artery bleeding Scopus articles Uterine artery bleeding impact factor journals Uterine artery bleeding Scopus journals Uterine artery bleeding PubMed journals Uterine artery bleeding medical journals Uterine artery bleeding free journals Uterine artery bleeding best journals Uterine artery bleeding top journals Uterine artery bleeding free medical journals Uterine artery bleeding famous journals Uterine artery bleeding Google Scholar indexed journals Congenital articles Congenital Research articles Congenital review articles Congenital PubMed articles Congenital PubMed Central articles Congenital 2023 articles Congenital 2024 articles Congenital Scopus articles Congenital impact factor journals Congenital Scopus journals Congenital PubMed journals Congenital medical journals Congenital free journals Congenital best journals Congenital top journals Congenital free medical journals Congenital famous journals Congenital Google Scholar indexed journals Uterine malformations articles Uterine malformations Research articles Uterine malformations review articles Uterine malformations PubMed articles Uterine malformations PubMed Central articles Uterine malformations 2023 articles Uterine malformations 2024 articles Uterine malformations Scopus articles Uterine malformations impact factor journals Uterine malformations Scopus journals Uterine malformations PubMed journals Uterine malformations medical journals Uterine malformations free journals Uterine malformations best journals Uterine malformations top journals Uterine malformations free medical journals Uterine malformations famous journals Uterine malformations Google Scholar indexed journals dilatation and curettage articles dilatation and curettage Research articles dilatation and curettage review articles dilatation and curettage PubMed articles dilatation and curettage PubMed Central articles dilatation and curettage 2023 articles dilatation and curettage 2024 articles dilatation and curettage Scopus articles dilatation and curettage impact factor journals dilatation and curettage Scopus journals dilatation and curettage PubMed journals dilatation and curettage medical journals dilatation and curettage free journals dilatation and curettage best journals dilatation and curettage top journals dilatation and curettage free medical journals dilatation and curettage famous journals dilatation and curettage Google Scholar indexed journals N-butyl cyanoacrylate articles N-butyl cyanoacrylate Research articles N-butyl cyanoacrylate review articles N-butyl cyanoacrylate PubMed articles N-butyl cyanoacrylate PubMed Central articles N-butyl cyanoacrylate 2023 articles N-butyl cyanoacrylate 2024 articles N-butyl cyanoacrylate Scopus articles N-butyl cyanoacrylate impact factor journals N-butyl cyanoacrylate Scopus journals N-butyl cyanoacrylate PubMed journals N-butyl cyanoacrylate medical journals N-butyl cyanoacrylate free journals N-butyl cyanoacrylate best journals N-butyl cyanoacrylate top journals N-butyl cyanoacrylate free medical journals N-butyl cyanoacrylate famous journals N-butyl cyanoacrylate Google Scholar indexed journals uterine artery embolization articles uterine artery embolization Research articles uterine artery embolization review articles uterine artery embolization PubMed articles uterine artery embolization PubMed Central articles uterine artery embolization 2023 articles uterine artery embolization 2024 articles uterine artery embolization Scopus articles uterine artery embolization impact factor journals uterine artery embolization Scopus journals uterine artery embolization PubMed journals uterine artery embolization medical journals uterine artery embolization free journals uterine artery embolization best journals uterine artery embolization top journals uterine artery embolization free medical journals uterine artery embolization famous journals uterine artery embolization Google Scholar indexed journals hysterectomy articles hysterectomy Research articles hysterectomy review articles hysterectomy PubMed articles hysterectomy PubMed Central articles hysterectomy 2023 articles hysterectomy 2024 articles hysterectomy Scopus articles hysterectomy impact factor journals hysterectomy Scopus journals hysterectomy PubMed journals hysterectomy medical journals hysterectomy free journals hysterectomy best journals hysterectomy top journals hysterectomy free medical journals hysterectomy famous journals hysterectomy Google Scholar indexed journals Ultrasonography articles Ultrasonography Research articles Ultrasonography review articles Ultrasonography PubMed articles Ultrasonography PubMed Central articles Ultrasonography 2023 articles Ultrasonography 2024 articles Ultrasonography Scopus articles Ultrasonography impact factor journals Ultrasonography Scopus journals Ultrasonography PubMed journals Ultrasonography medical journals Ultrasonography free journals Ultrasonography best journals Ultrasonography top journals Ultrasonography free medical journals Ultrasonography famous journals Ultrasonography Google Scholar indexed journals Peak systolic velocity articles Peak systolic velocity Research articles Peak systolic velocity review articles Peak systolic velocity PubMed articles Peak systolic velocity PubMed Central articles Peak systolic velocity 2023 articles Peak systolic velocity 2024 articles Peak systolic velocity Scopus articles Peak systolic velocity impact factor journals Peak systolic velocity Scopus journals Peak systolic velocity PubMed journals Peak systolic velocity medical journals Peak systolic velocity free journals Peak systolic velocity best journals Peak systolic velocity top journals Peak systolic velocity free medical journals Peak systolic velocity famous journals Peak systolic velocity Google Scholar indexed journals
Article Details
1. Introduction
Uterine arteriovenous malformations (AVMs) are an unusual cause of uterine artery bleeding that can be either congenital or acquired following uterine instrumentation, trauma, infection, or Gestational trophoblastic disease [1]. Uterine artery malformations are mostly acquired malformations that is abide by a pregnancy event and investigated when uterine artery bleeding remains unmanageable despite medical measures. The bleeding caused by uterine malformations is episodic and can be severe, warranting hospitalization and blood transfusions. Traditional therapies of AVMs include medical management of symptomatic bleeding, blood transfusions, uterine artery embolization (UAE), or hysterectomy [2]. Treatment usually depends on the symptoms, age, desire for future fertility, localization, and lesion size. Uterine artery embolization is a preferred method of treating AVM, particularly in the patients of reproductive age group [3].
2. Case Report
A 27 years old female, P1 L1 A3, presented to our hospital on July 04, 2020 with chief complaints of intermittent per vaginal bleed in the form of spotting for the last 2.5 months and pain in the lower abdomen for the same duration. Her last menstrual period (LMP) date was June 28, 2020.
The patient had overdue of menses, for which she did a urine human chorionic gonadotropin level test, which came out to be positive. Ultrasonography was done in a private hospital confirming the intrauterine pregnancy. Serum beta HCG was raised (1.5 lakh mIU/ml). The patient had two bleeding episodes during this pregnancy, each lasting for ten days. According to the previous treatment history, she underwent a medical abortion on April 14, 2020 and Dilatation and curettage (D&C) on April 16, 2020. Since then, the patient was having on and off per vaginal bleeding along with pain abdomen. There was no history of the passage of clot per vaginally.
The patient had a history of two more D&Cs in the past. Apart from that, she had a history of Laparoscopic cholecystectomy done for the treatment of cholelithiasis. Her liver function tests and kidney function tests were within normal limits. Again, Ultrasonography (June 29, 2020) was done in a private hospital for persistent per vaginal bleed, which showed a Bulky uterus measuring 12.4 x 7.2 x 5.2 cm with a heterogeneous mass-like area involving endometrium, myometrium of the lower uterine segment, and cervix showing arterial and venous flow on doppler study. Spectral analysis of the arterial vessels using doppler showed a low resistance and high-velocity flow. Peak systolic velocity (PSV) and resistance index (RI) were 47 cm/s and 0.32, respectively. These findings were suggestive of AVM. Also, CT Angiography (July 01, 2020) was done, which revealed a bulky uterus with a large well-defined lesion in the lower uterine segment involving the myometrium and endometrium with internal necrosis. It also showed multiple dilated and tortuous arteries and veins within the lesion supplied by the bilateral uterine artery and drained by bilateral uterine vein suggestive of AVM. The patient was planned for Digital subtraction angiography with uterine artery embolization on July 06, 2020 in the interdepartmental meeting.
After informed consent was obtained, both femoral arteries were punctured with an 18G puncture needle under Local Anaesthesia, and a 6Fr sheath was placed. 2500 U of heparin was given. 5Fr C1 catheter was navigated through the sheath, and Aortic run-off was taken. Selective external and internal iliac artery catheterization was done, and angiography was taken. It showed hypertrophied and tortuous bilateral uterine arteries (R>L). A tangle of vascular structures was seen, supplied by both rights and left uterine artery (Figure 1). Using 2.7 Fr Terumo Progreat microcatheter, super-selective catheterization of both arteries was done sequentially and embolised. Immediate flushing with 5% Dextrose was done, followed by removal of the Microcatheter. Embolising agent used was 20% lipiodol- nBCA (N-butyl cyanoacrylate) mixture. Postprocedural control angiogram showed complete devascularisation with patent other iliac artery branches (Figure 2 and 3). The Proximal left uterine artery was patent. Then, femoral sheath was removed, and manual compression was done to achieve hemostasis. A Pressure bandage was applied after that. No major post-procedure complication was noted except for diffuse pain in the lower abdomen, which was managed with oral and intravenous analgesics. The patient was planned for review USG Pelvis (B mode + doppler) two days after the procedure.
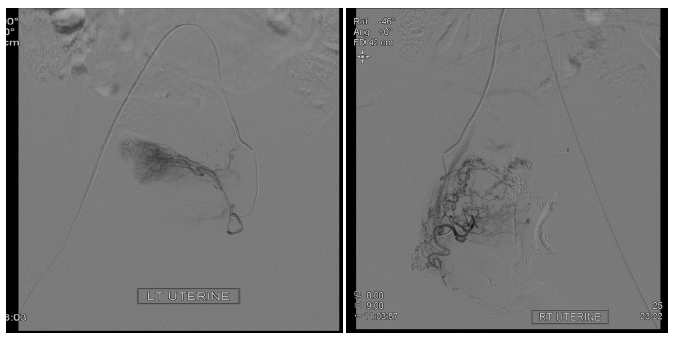
Figure 1: Shows the tangled vascular network supplied by bilateral uterine arteries seen during super selective angiogram of the vessels.
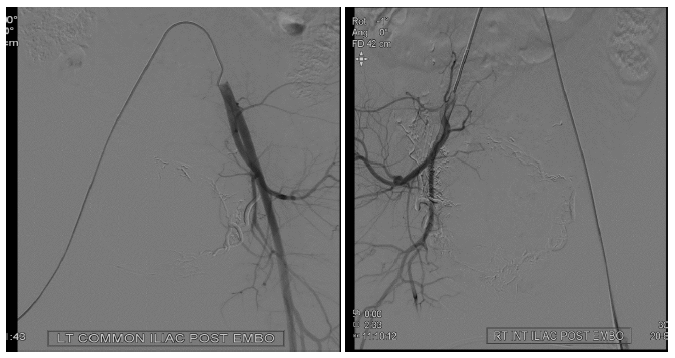
Figure 2: Shows post embolization angiogram of both iliac arteries showing no residual vascular network.
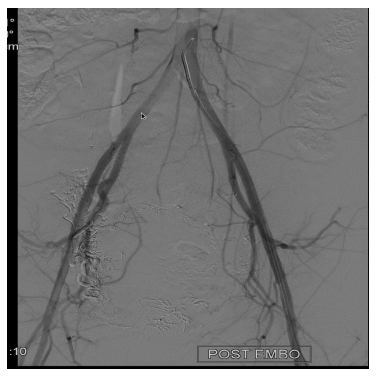
Figure 3: Shows post embolization angiogram at aortic bifurcation. No residual lesion is noted.
Ultrasonography (July 08, 2020) showed a heterogeneous soft tissue lesion with anechoic areas within the lower uterine segment measuring 7.2 x 6.9 cm in size involving anterior and posterior myometrium. The upper part of the uterus and thin posterior myometrial tissue are uninvolved. On the Doppler study, no flow was noted within the anechoic areas. Few echogenic foci were seen within the lesion.
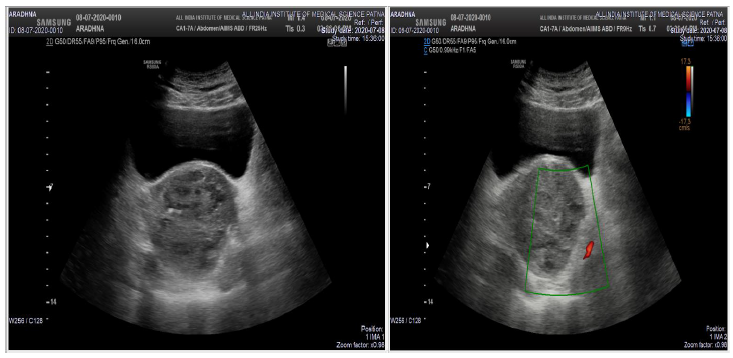
Figure 4: Shows the post-procedure USG (B mode+ colour doppler)- Heterogenous soft tissue lesion with anechoic areas within is noted in the lower uterine segment. No flow was noted within the anechoic areas on colour doppler.
There was no recurrent episode of abnormal uterine bleeding at the two-week follow-up visit. Also, the menstrual cycle of the patient returned to normal one month after the follow-up.
3. Discussion
Uterine Arteriovenous malformation is an uncommon condition which can result in serious life-threatening complications. They can lead to acute severe bleeding, infertility, or abnormal placentation. Uterine AVM can be congenital or acquired. Common acquired causes include uterine instrumentation, trauma, infection, gestational trophoblastic disease, and gynaecologic malignancies [4]. With the increased number of gynecological surgical procedures being done, the acquired uterine AVM prevalence will increase. Thus, uterine AVM is a differential that should be considered in any patient who presents with abnormal uterine bleeding.
Earlier AVM was diagnosed by laparotomy or during an examination of the uterine specimen after a hysterectomy [5]. However, with the availability of colour Doppler US, a non-invasive method, early diagnosis is possible. Grayscale ultrasound can detect multiple serpentine tubular or sponge-like anechoic or hypoechoic regions within the myometrium with normal endometrium, which on color doppler shows both arterial as well as venous flow. The spectral analysis will show high velocity (mean PSV: 136 cm/s), low resistance (mean RI: 0.3) flow, low pulsatility of the arterial waveform, and pulsatile high-velocity venous waveform. Differential diagnosis includes haemangioma, gestational trophoblastic disease, complex ovarian cyst, and retained products of conception. Thus, Digital subtraction angiography (DSA) remains the gold standard for diagnosis [5].
MRI is an excellent imaging modality providing an accurate definition of uterine AVMs and delineating the invasion of adjacent organs. The characteristic features include a sizeable bulky uterus with a focal mass, multiple serpentine flow-related signal voids within the lesion, disruption of the junctional zones, and prominent parametrial vessels [6]. Gadolinium-enhanced MRI demonstrates a hypervascular arterial-dominant flow. Like MRI, computed tomography (CT) may be used to determine the vascularity, extent, size, and involvement of the adjacent organs [7].
Peitsidis and colleagues [2] reported an extensive review of all reported cases of acquired AVM after D&C, in which 91 studies totaling 103 patients (1954–2011) were included. Among these, 95 women reported having a history of a curettage procedure before the onset of their symptoms. The mean age of diagnosis was 30 years, with 96% being premenopausal. UAE was the foremost standard treatment (59%), followed by hysterectomy (29%). The recurrence rate following UAE was 17%.
Traditionally, hysterectomy was the preferred modality in treating uterine AVMs; however, UAE, because of its effectiveness, minimally invasive nature, and the possibility of preserving uterine function to allow future childbearing, is increasingly becoming one of the preferred treatment methods [8]. Studies have shown bilateral UAE to be effective in 90% of the cases, with technical failures related to procedure complications, incomplete embolization, and rupture of the uterine artery in rest. Different embolization materials, including isobutyl-2-cyanoacrylate, detachable balloons, gelatin sponge, coils, thrombin, and polyvinyl alcohol, have been used in these procedures. However, there have been no study comparing the efficacy of different methods. In our case, we used a 20% lipiodol-nBCA (N-butyl cyanoacrylate) mixture as the embolizing agent [9].
4. Conclusion
Bilateral UAE using nBCA is a safe, effective, and minimally invasive method to treat uterine AVMs, which has long-term efficacy and can preserve fertility.
References
- Beller U, Rosen RJ, Beckman EM, et al. Congenital arteriovenous malformation of the female pelvis: A gynecologic perspective. Am J Obstet Gynecol 159 (1988): 1153-1160.
- Peitsidis P, Manolakos E, Tsekoura V, et al. Uterine arteriovenous malformations induced after diagnostic curettage: a systematic review. Arch Gynecol Obstet 284 (2011): 1137.
- Khan S, Saud S, Khan I, et al. Acquired Uterine Arteriovenous Malformation Following Dilatation and Curettage Treated with Bilateral Uterine Artery Embolization: A Case Report. Cureus 11 (2020): PMC6516630.
- Hashim H, Nawawi O. Uterine Arteriovenous Malformation. Malays J Med Sci MJMS 20 (2013): 76-80.
- Grivell RM, Reid KM, Mellor A. Uterine arteriovenous malformations: a review of the current literature. Obstet Gynecol Surv 60 (2005): 761-767.
- Huang MW, Muradali D, Thurston WA, et al. Uterine arteriovenous malformations: gray-scale and Doppler US features with MR imaging correlation. Radiology 206 (1998): 115-123.
- Müngen E. Vascular abnormalities of the uterus: have we recently over-diagnosed them? Ultrasound Obstet Gynecol 21 (2003): 529-531.
- Vilos AG, Vilos GA, Hollett-Caines J, et al. Uterine artery embolization for uterine arteriovenous malformation in five women desiring fertility: pregnancy outcomes. Hum Reprod 30 (2015): 1599-1605.
- Uterine artery embolization: An underused method of controlling pelvic hemorrhage - American Journal of Obstetrics & Gynecology (2020): 70624-0.
