Tuberculosis of the Male Breast Mimicking Breast Cancer. A Case Report from Low-Resource Country
Article Information
Kenfack B1*, Atemkeng Tsatedem F1, Fouogue Tsuala J1, Dobgima Pisoh W2, Kenfack BC3 and Sando Z4
1Faculty of Medicine and Pharmaceutical Sciences, University of Dschang, Cameroon
2Faculty of Heath Sciences, University of Bamenda, Cameroon
3Catholic University of Cameroon
4Faculty of Medicine and Biomedical Sciences, University of Yaoundé 1, Cameroon
*Corresponding Author: Kenfack Bruno, Faculty of Medicine and Pharmaceutical Sciences, University of Dschang, Cameroon
Received: 04 April 2023; Accepted: 17 April 2023; Published: 28 April 2023
Citation: Kenfack B, Atemkeng Tsatedem F, Fouogue Tsuala J, Dobgima Pisoh W, Kenfack BC and Sando Z. Tuberculosis of the Male Breast Mimicking Breast Cancer. A Case Report from Low-Resource Country. Archives of Clinical and Medical Case Reports. 7 (2023): 178-180.
Share at FacebookAbstract
Introduction: Tuberculosis (TB) mainly affects lungs but may also have extra-pulmonary localizations, among which the breast. The incidence of breast TB is estimated at 0.1% of all breast lesions in Western countries and 3-4% in tuberculosis endemic regions. Primary breast tuberculosis (PBT) is defined as tuberculosis localized only in the breast, in a patient with no history of pulmonary TB. PBT is very rare and represents 0.06%- 0.1% of all tuberculosis localizations.
Case Report: We report here a case of a 22 years old male student presenting with a mildly painful right breast lump evolving for three months. Physical examination revealed a sub-areolar lump, 3 cm in diameter, ill-defined, fixed to the surrounding tissues and not warm to touch. Two axillary lymph nodes of less than 1 cm were palpable. The diagnosis of male breast cancer was suspected, with chronic abscess as differential diagnosis. Breast ultrasound revealed a mass of 32 mm in diameter with central necrosis. Needle biopsy of the breast lump confirmed the diagnosis of tuberculosis. The patient received oral anti-tuberculosis drugs for six months and the mass regressed completely without any complication.
Conclusion: Breast tuberculosis is a rare entity especially in male breast, mimicking carcinoma. Clinical awareness is necessary during diagnostic workup to establish the correct diagnosis and treatment.
Keywords
Breast tuberculosis; Male; Medical treatment
Article Details
1. Introduction
Although being a preventable and curable disease, tuberculosis (TB) is still a global health problem, responsible for 1.4 million deaths in 2019 [1]. All the organs can be affected by TB, with some disparity in the incidence in favour of the lung. The two most frequent risk factors are HIV infection and malnutrition [1]. The diagnosis of the extra pulmonary locations, especially in their primary form, can be challenging. Breast TB is an uncommon location first described in 1829 [2]. The reported incidence of breast TB is less than 1% of all breast diseases [2]. Primary breast tuberculosis is defined as TB localized only in the breast, in a patient with no history of pulmonary TB. It is an extremely rare condition and therefore may be misdiagnosed as a cancer, especially in men. Kakkar et al. [2] found 6 cases of male TB out of 160 cases (3.9%) in India.
2. Case Report
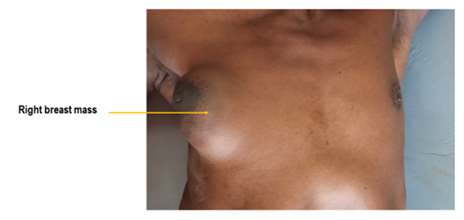
We report here a case of a 22 years old male student of Chadian origin presenting with a mildly painful right breast lump evolving for three months (Figure 1).
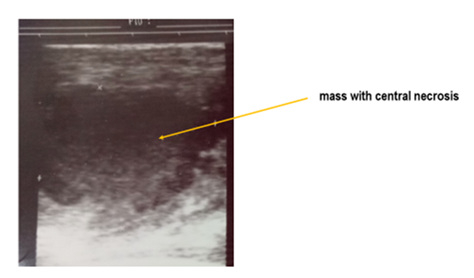
His past medical history revealed no chronic lung infection. Physical examination revealed a blood pressure of 120/88 mmHg, temperature of 37.4°C, weight of 57 Kg, and height of 172 cm. The breast lump was sub-areola, 3 cm in diameter, ill-defined, slightly tender on palpation, fixed to surrounding tissues and not warm to touch. Two ipsilateral axillary lymph nodes of less than 1 cm were palpable. The diagnosis of male breast cancer was suspected, with chronic abscess as differential. Breast ultrasound showed a mass of 32 mm in diameter with central necrosis (Figure 2).
Needle biopsy of the lump confirmed the diagnosis of tuberculosis, presenting as an inflammatory granuloma with tuberculous-like caseum. The patient was transferred to the Anti-tuberculosis Unit of the Dschang (Cameroon) District Hospital where he received oral ambulatory anti-tuberculosis made of Rifampicin 600 mg, Isoniazid 300 mg, Ethambutol 1800 mg for 2 months followed by Rifampicin 600 mg, Isoniazid 300 mg drugs for 4 months. The mass regressed completely without any complication at the end of the 6-months therapy (Figure 3).
3. Discussion
Tuberculosis is mostly found in low and middle-income countries. Among the most frequently reported risk factors are HIV infection and malnutrition [1]. Our patient had some of these environmental and clinical risk factors as he was a migrated Chadian student with poor living conditions, but HIV-negative. Moreover, he had never received the anti-tuberculous vaccine. The history of the presenting symptoms in breast TB is usually less than a year [3]. In our case, the symptoms lasted for 3 months prior to consultation. This relatively short period may be explained by the fact that he was a male and therefore, the lump was easily identifiable. Clinically, breast tuberculosis can mimic carcinoma, and it can be mistaken for a pyogenic breast abscess. The lump is generally painful and often located in the central or upper outer quadrant of the breast. It may be associated with a discharge as well as ipsilateral axillary lymph nodes [4,5]. In our case, the lump was sub-areola, tender, ill-defined, associated with axillary lymph nodes and had been evolving for more than 3 months, all these making it suspicious of a malignant mass.
The standard algorithm for the investigation of a breast tumour starts with clinical exam, followed by medical imaging and lastly pathologic analysis. The simple and widely used imaging technique, the ultrasound, was done and showed a picture suggestive of a necrotising tumour. For many authors [6,7], ultrasound played a key role in their diagnostic procedure of breast TB.
Even though ultrasound provides strong arguments for TB, pathology exam is mandatory to confirm the diagnosis. Needle aspiration biopsy is preferred to open biopsy. Fine needle aspiration cytology (FNAC) from the breast lesion remains an important diagnostic tool for breast tuberculosis. In the study of Kakkar et al. in India [2], 73% of cases of breast tuberculosis were diagnosed on FNAC when both epitheloid cell granulomas and necrosis were present as in our case. Opening the abscess for pus drainage would have led to a hard-to-heal wound.
No specific guidelines are available for chemotherapy of breast tuberculosis, and therapy generally follows the guidelines commonly used for pulmorary TB. The patient was treated with 6 months’ therapy including: 2 months of Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol followed by 4 months of Isoniazid and Rifampicin. The mass regressed completely by the end of the treatment. In the series of 100 cases of breast TB treated by chemotherapy, only 90% were free of disease after 6 months [8]. The challenge the clinician faces with breast TB is therefore that of diagnosis rather than that of treatment.
4. Conclusion
Primary breast tuberculosis is a rare entity especially in male breast, mimicking carcinoma. It should always be suspected in patients from endemic areas. Clinical awareness is necessary during diagnostic workup to establish the correct diagnosis and treatment. The mainstay of treatment is anti-tuberculosis therapy if imaging and histopathology confirm the diagnosis.
Conflict of Interest
The authors have no conflict of interest to declare
References
- Global tuberculosis report 2020. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO (2020).
- Kakkar S, Kapila K, Singh MK, et al. Tuberculosis of the breast. A cytomorphologic study. Ada Cytol 44 (2000): 292-296.
- Tewari M, Shukla HS. Breast tuberculosis: diagnosis, clinical features and management. Indian Journal of Medical Research 122 (2005): 103-110.
- Asjad B, Ali M, Naeem B Kiran, et al. Breast Abcess and Tuberculosis and its Diagnostic Challenges: A Two-Year Prospective Study in Karachi, Pakistan. Cureus 11 (2019): e5909.
- Rizzo G, Colli F, De Marco P, et al. An unusual presentation of breast tuberculosis: A case report. Clin Case Rep 9 (2021): 210-212.
- Fatima K, Naz F. Tuberculosis of Male Breast: A Rare Benign Entity. Cureus 11 (2019): e4709.
- Ghalleb M, Seghaier S, Adouni O, et al. Breast tuberculosis: a case series. J Med Case Reports 15 (2021): 73.
- Shinde SR, Chandawarkar RY, Deshmukh SP. Tuberculosis of the breast masquerading as carcinoma: a study of 100 patients. World J Surg 19 (1995): 379-381.