Treatment of a Displaced Occipital Condyle Fracture - A Case to be discussed
Article Information
Vinz F1*, Ullrich BW1,2, Goehre F3, Hofmann GO1,2, Mendel T1,2
1BG Klinikum Bergmannstrost gGmbH, Department of Trauma and Reconstructive, Surgery, Merseburger Str. 165, 06112 Halle (Saale), Germany
2Friedrich Schiller University Jena, Department of Trauma, Hand and Reconstructive, Surgery, Erlanger Allee 101, 07747 Jena, Germany
3BG Klinikum Bergmannstrost gGmbH, Department of Neurosurgery, Merseburger, Str. 165, 06112 Halle (Saale), Germany
*Corresponding Author: Dr. Franziska Vinz, BG Klinikum Bergmannstrost gGmbH, Department of Trauma and Reconstructive Surgery, Merseburger Str. 165, 06112 Halle (Saale), Germany
Received: 01 July 2021; Accepted: 15 July 2021; Published: 03 September 2021
Citation:
Vinz F, Ullrich BW, Goehre F, Hofmann GO, Mendel T. Treatment of a Displaced Occipital Condyle Fracture - A Case to be discussed. Journal of Orthopaedics and Sports Medicine 3 (2021): 140-151.
Share at FacebookAbstract
Before the advent of computed tomography, occipital condyle injuries were solely a postmortem diagnosis. Nowadays, CT is well established in the diagnostic workflow of trauma management, allowing accurate planning and proper treatment. Anderson and Montesano as well Tuli developed radiologic classifications, each based on a small number of cases, in regards to the stability of the lesion and also provided treatment recommendations. In this case study we present a 24-year-old man suffering massive trauma to the head and thorax from a agricultural vehicle accident, leading to a displaced avulsion fracture of the right occipital condyle with high atlanto-occipital instability (Anderson Montesano type III). However, the patient did not develop any neurological deficit. Within the scope of the damage control polytrauma algorithm, the atlanto-occipital instability was initially stabilized in a HALO fixator. For devinitive treatment, we decided on an internal occipito-cervical fixation with a permanent fusion of the injured C0/C1-segment without reduction of the dislocated fragment at a time 14 days after the accident. The fixation construct spanned from the occiput to C3 in order to achieve a high primary stability. At 3-months follow-up, CT scans showed bony healing of the right condyle in an unchanged displaced position and a successful posterior fusion of C0/C1. After one year, a complete implant removal was done.
Keywords
Occipital condyle fracture; Operative vs. non-operative treatment; Operative cervicocranial fusion
Reconstructive articles Reconstructive Research articles Reconstructive review articles Reconstructive PubMed articles Reconstructive PubMed Central articles Reconstructive 2023 articles Reconstructive 2024 articles Reconstructive Scopus articles Reconstructive impact factor journals Reconstructive Scopus journals Reconstructive PubMed journals Reconstructive medical journals Reconstructive free journals Reconstructive best journals Reconstructive top journals Reconstructive free medical journals Reconstructive famous journals Reconstructive Google Scholar indexed journals Upper cervical spine articles Upper cervical spine Research articles Upper cervical spine review articles Upper cervical spine PubMed articles Upper cervical spine PubMed Central articles Upper cervical spine 2023 articles Upper cervical spine 2024 articles Upper cervical spine Scopus articles Upper cervical spine impact factor journals Upper cervical spine Scopus journals Upper cervical spine PubMed journals Upper cervical spine medical journals Upper cervical spine free journals Upper cervical spine best journals Upper cervical spine top journals Upper cervical spine free medical journals Upper cervical spine famous journals Upper cervical spine Google Scholar indexed journals Polytrauma articles Polytrauma Research articles Polytrauma review articles Polytrauma PubMed articles Polytrauma PubMed Central articles Polytrauma 2023 articles Polytrauma 2024 articles Polytrauma Scopus articles Polytrauma impact factor journals Polytrauma Scopus journals Polytrauma PubMed journals Polytrauma medical journals Polytrauma free journals Polytrauma best journals Polytrauma top journals Polytrauma free medical journals Polytrauma famous journals Polytrauma Google Scholar indexed journals Spinal cord articles Spinal cord Research articles Spinal cord review articles Spinal cord PubMed articles Spinal cord PubMed Central articles Spinal cord 2023 articles Spinal cord 2024 articles Spinal cord Scopus articles Spinal cord impact factor journals Spinal cord Scopus journals Spinal cord PubMed journals Spinal cord medical journals Spinal cord free journals Spinal cord best journals Spinal cord top journals Spinal cord free medical journals Spinal cord famous journals Spinal cord Google Scholar indexed journals Non-dislocated fracture articles Non-dislocated fracture Research articles Non-dislocated fracture review articles Non-dislocated fracture PubMed articles Non-dislocated fracture PubMed Central articles Non-dislocated fracture 2023 articles Non-dislocated fracture 2024 articles Non-dislocated fracture Scopus articles Non-dislocated fracture impact factor journals Non-dislocated fracture Scopus journals Non-dislocated fracture PubMed journals Non-dislocated fracture medical journals Non-dislocated fracture free journals Non-dislocated fracture best journals Non-dislocated fracture top journals Non-dislocated fracture free medical journals Non-dislocated fracture famous journals Non-dislocated fracture Google Scholar indexed journals Thoracic trauma articles Thoracic trauma Research articles Thoracic trauma review articles Thoracic trauma PubMed articles Thoracic trauma PubMed Central articles Thoracic trauma 2023 articles Thoracic trauma 2024 articles Thoracic trauma Scopus articles Thoracic trauma impact factor journals Thoracic trauma Scopus journals Thoracic trauma PubMed journals Thoracic trauma medical journals Thoracic trauma free journals Thoracic trauma best journals Thoracic trauma top journals Thoracic trauma free medical journals Thoracic trauma famous journals Thoracic trauma Google Scholar indexed journals Injury severity score articles Injury severity score Research articles Injury severity score review articles Injury severity score PubMed articles Injury severity score PubMed Central articles Injury severity score 2023 articles Injury severity score 2024 articles Injury severity score Scopus articles Injury severity score impact factor journals Injury severity score Scopus journals Injury severity score PubMed journals Injury severity score medical journals Injury severity score free journals Injury severity score best journals Injury severity score top journals Injury severity score free medical journals Injury severity score famous journals Injury severity score Google Scholar indexed journals CT-angiography articles CT-angiography Research articles CT-angiography review articles CT-angiography PubMed articles CT-angiography PubMed Central articles CT-angiography 2023 articles CT-angiography 2024 articles CT-angiography Scopus articles CT-angiography impact factor journals CT-angiography Scopus journals CT-angiography PubMed journals CT-angiography medical journals CT-angiography free journals CT-angiography best journals CT-angiography top journals CT-angiography free medical journals CT-angiography famous journals CT-angiography Google Scholar indexed journals Vertebral artery articles Vertebral artery Research articles Vertebral artery review articles Vertebral artery PubMed articles Vertebral artery PubMed Central articles Vertebral artery 2023 articles Vertebral artery 2024 articles Vertebral artery Scopus articles Vertebral artery impact factor journals Vertebral artery Scopus journals Vertebral artery PubMed journals Vertebral artery medical journals Vertebral artery free journals Vertebral artery best journals Vertebral artery top journals Vertebral artery free medical journals Vertebral artery famous journals Vertebral artery Google Scholar indexed journals Cervical spine articles Cervical spine Research articles Cervical spine review articles Cervical spine PubMed articles Cervical spine PubMed Central articles Cervical spine 2023 articles Cervical spine 2024 articles Cervical spine Scopus articles Cervical spine impact factor journals Cervical spine Scopus journals Cervical spine PubMed journals Cervical spine medical journals Cervical spine free journals Cervical spine best journals Cervical spine top journals Cervical spine free medical journals Cervical spine famous journals Cervical spine Google Scholar indexed journals Bone grafting articles Bone grafting Research articles Bone grafting review articles Bone grafting PubMed articles Bone grafting PubMed Central articles Bone grafting 2023 articles Bone grafting 2024 articles Bone grafting Scopus articles Bone grafting impact factor journals Bone grafting Scopus journals Bone grafting PubMed journals Bone grafting medical journals Bone grafting free journals Bone grafting best journals Bone grafting top journals Bone grafting free medical journals Bone grafting famous journals Bone grafting Google Scholar indexed journals Neurovascular articles Neurovascular Research articles Neurovascular review articles Neurovascular PubMed articles Neurovascular PubMed Central articles Neurovascular 2023 articles Neurovascular 2024 articles Neurovascular Scopus articles Neurovascular impact factor journals Neurovascular Scopus journals Neurovascular PubMed journals Neurovascular medical journals Neurovascular free journals Neurovascular best journals Neurovascular top journals Neurovascular free medical journals Neurovascular famous journals Neurovascular Google Scholar indexed journals Thorax articles Thorax Research articles Thorax review articles Thorax PubMed articles Thorax PubMed Central articles Thorax 2023 articles Thorax 2024 articles Thorax Scopus articles Thorax impact factor journals Thorax Scopus journals Thorax PubMed journals Thorax medical journals Thorax free journals Thorax best journals Thorax top journals Thorax free medical journals Thorax famous journals Thorax Google Scholar indexed journals Shoulder girdle articles Shoulder girdle Research articles Shoulder girdle review articles Shoulder girdle PubMed articles Shoulder girdle PubMed Central articles Shoulder girdle 2023 articles Shoulder girdle 2024 articles Shoulder girdle Scopus articles Shoulder girdle impact factor journals Shoulder girdle Scopus journals Shoulder girdle PubMed journals Shoulder girdle medical journals Shoulder girdle free journals Shoulder girdle best journals Shoulder girdle top journals Shoulder girdle free medical journals Shoulder girdle famous journals Shoulder girdle Google Scholar indexed journals Thoracic vertebrae articles Thoracic vertebrae Research articles Thoracic vertebrae review articles Thoracic vertebrae PubMed articles Thoracic vertebrae PubMed Central articles Thoracic vertebrae 2023 articles Thoracic vertebrae 2024 articles Thoracic vertebrae Scopus articles Thoracic vertebrae impact factor journals Thoracic vertebrae Scopus journals Thoracic vertebrae PubMed journals Thoracic vertebrae medical journals Thoracic vertebrae free journals Thoracic vertebrae best journals Thoracic vertebrae top journals Thoracic vertebrae free medical journals Thoracic vertebrae famous journals Thoracic vertebrae Google Scholar indexed journals
Article Details
1. Case Presentation
While cleaning a manure spreader a 24-year-old man suffered a massive compression trauma of the neck and upper chest when one of the vehicle’s sprayer arms shifted with a force of approximately one ton (Figure 1). He was freed from the vehicle with the help of colleagues and heavy machinery. His initial GCS was 15 points. He complained of pain in the upper cervical spine, chest and shoulder girdle. After first aid and immobilisation in a stiffnek and vacuum mattress the patient was transported via rescue helicopter into our Level-I trauma center. He arrived at the emergency room in a stable cardiopulmonary condition with retrograde amnesia to the accident, nausea and headache, but normal neurological status. Polytrauma CT scans detected a displaced fracture of the right occipital condyle close to the spinal cord (Figures 2 a, b, c), a type III injury according to Anderson and Montesano [1-5]. Additionally, he suffered from a peri-mesencephalic subarachnoid hemorrhage branching out to the ventricle system, a non-dislocated fracture of the right petros bone, a thoracic trauma with a serial rib fracture as well as a small pneumothorax, fractures of the transverse process of the 3rd and 4th thoracic vertebra as well as fractures to the right coracoid and the left scapula. His total Injury Severity Score (ISS) amounted to 25 points. To determine the dimensions of the occiput condyle injury, we subsequently performed CT-angiography. Imaging revealed direct contact of the medially-rotated and dislocated right occipital condyle to the V4-segment of the vertebral artery, but no compromising of the vessel (Figures 3 a, b).

Figure 1: Manure spreader with sprayer arms.
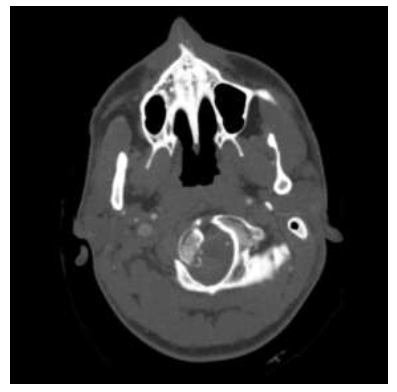
Figure 2a: Polytrauma CT scans showing the displaced fracture of the right occipital condyle (type III according to Anderson and Montesano).
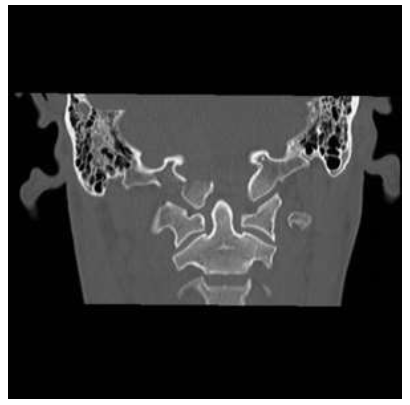
Figure 2b: Polytrauma CT scans showing the displaced fracture of the right occipital condyle (type III according to Anderson and Montesano
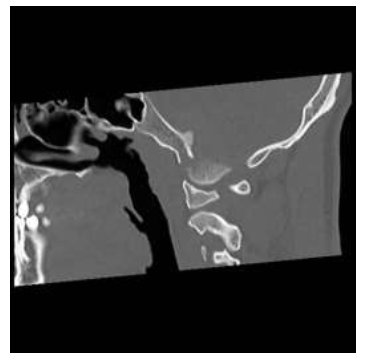
Figure 2c: Polytrauma CT scans showing the displaced fracture of the right occipital condyle (type III according to Anderson and Montesano).

Figure 3a: Postoperative X-rays of the cervical spine in (a) a.p. projection.

Figure 3b: Postoperative X-rays of the cervical spine in (b) lateral projection.
To further stabilize the highly unstable C0 injury a HALO fixator was applied at the same day. In the following hours the patient’s status deteriorated rapidly showing vomiting and increasing disorientation. A subsequent cranial CT scan showed an extension of the cerebral haemorrhage, particularly in the 4th ventricle and around the foramen magnum. The patient’s status improved after trepanation, installation of intracerebral pressure pressure tube and ventricle drainage.
Four days later the ventricle drainage could be removed. Five days after the accident the patient could be transferred from the ICU to our trauma ward.
2. Operative Procedure
We discussed the surgical treatment options in respect of expected functional outcome, potential peri-operative risk and patient’s volition. Therefore, three strategies came into consideration: A definitive fracture treatment with the HALO fixation for 8 to 10 weeks represented the option with the lowest iatrogenic risk. However, the wearing comfort is lousy. An occipito-cervical fusion (OCF) with additional bone grafting would be associated with a reasonable surgical invasion, but dismissing CO/C1 movement. Open reduction and internal screw fixation of the dislocated condyle fragment using the suboccipital approach with C1 hemilaminectomy and foraminatomy of the foramen magnum would promise a nearly complete functional restitution. However, this procedure is associated with a high risk of iatrogenic lesion of neurovascular structures.
The patient did not want the dislocated fracture to be reduced and decided for occipito-cervical fusion, despite of substancial functional loss of the occipito-axial and the atlanto-axial joints. Two weeks after the accident we performed surgery, using the dorsolateral, suboccipital transcondylar approach [6] and transfixing from the occiput to C3 vertebra (Mountaineer® OCT spinal system, Depuy-Synthes, Raynham, MA, USA) with apposition of bonegraft substitute (Actifuse®, Baxter Healthcare Corporation, Deerfield, IL, USA) C0/C2 fusion under 3D visualisation using the O-arm (Figures 4 a, b).
The injuries to the thorax, shoulder girdle and thoracic vertebrae where treated conservatively.

Figure 4a: Postoperative CT scans in (a) coronal reconstruction.

Figure 4b: Postoperative CT scans in (b) sagittal reconstruction.
3. Postoperative Course and Outcome
No intra- or postoperative complications occurred (Figures 5 a, b, c). Following surgery the cervical spine was immobilized in a soft collar for 6 weeks. Nine days after surgery the patient was released from the hospital in stable condition with a regular neurological status. We conducted a 12-week follow-up including clinical and radiographic examination. At this time CT scans showed an assimilation of the right occipital condyle in unchanged dislocation. In the following time he underwent intensive physiotherapy for muscle strengthening and motion improvement. One year after the accident we performed full implant removal, as planned to release the C2/3 segment. At last outpatient consultation the patient exhibited a limited range of motion, as expected, but did not complain of pain in the cervical spine or neurological deficits.
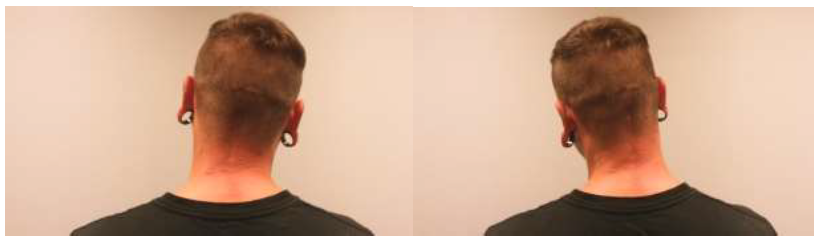
Figure 5a: Functional outcome of the cervical spine 14 months after trauma in side tilting.
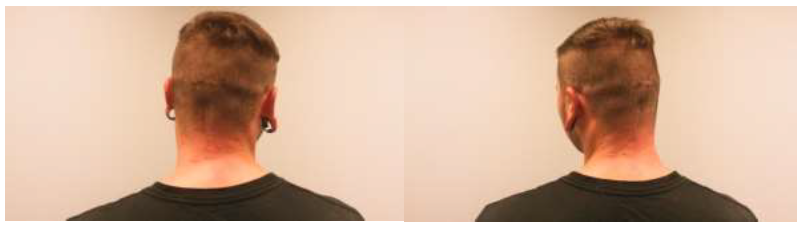
Figure 5b: Functional outcome of the cervical spine 14 months after trauma in (b) rotation.
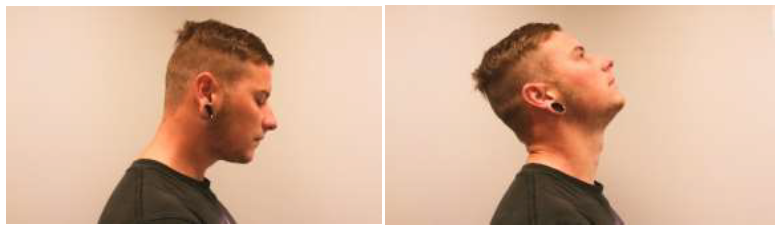
Figure 5c: Functional outcome of the cervical spine 14 months after trauma in (c) inclination/reclination.
4. Rational for Treatment and Review of the Literature
In the past, occipital condyle fractures were solely a postmortem diagnosis. Due to improved radiographic diagnosis techniques [2, 7], especially the modern widespread use of CT, outcomes have improved. Estimates of this injury’s incidence have a wide spread in the relevant literature. Aulino et. al identified an OCF in 0.65% of trauma admissions [2], Hanson et. al estimated the incidence at approximately 0.1% of patients [3], Maserati et al. calculated an incidence of 0,4% in their examined population [7] and the data of Mueller et al. indicates a 1% incidence [9].
In a large autopsy series of head trauma victims, OCF occured in 0.6% up to 4% of cases [10]. All authors agree that the mechanism leading to an OCF usually includes high impact cranial trauma [2, 3, 7, 11, 12] and occurs in association with muliple additional injuries. The paired occipital condyles and first two cervical vertebrae should be considered as a functional unit [3, 13]. The occipital condyles are prominences on the paired lateral exooccipital segments of the occipital bone on the anterior half of the foramen magnum [14, 15]. The condyles articulate with the lateral masses of C1 and are attached to C1/C2 by a number of ligaments [1, 14, 15]. The most important ligaments are the tectorial membrane and bilateral alar ligaments. They are the main limiting factor for axial rotation and, to a lesser degree, lateral flexion and anteroposterior rotation. The tectorial membrane is a continuation of the odontoid’s posterior face to the ventral surface of the foramen magnum. Its main function is to limit the extension of the atlantooccipital joints [2, 3, 15].
An injury to the occipitoatlantoaxial joint complex may lead to severe instability. Due to the complex anatomic relationship, an OCF in particular can cause lesions to the hypoglossal canal, jugular foramen, vascular structures and medulla oblongata [15, 16, 17]. The jugular canal sits just lateral to the hypoglossal canal and occipital condyles (approx. 1 cm). Through this canal pass the cranial nerves IX-XI, Jacobson's and Arnold's nerve, the inferior petrosal sinus, the internal jugular vein and the posterior meningeal artery.
The medulla oblongata, meninges, vertebral arteries, and the anterior and posterior spinal arteries and veins pass through the foramen magnum [12, 15].
An injury of the occipital condyles is difficult to detect clinically, as most patients are not accessable to full examination due to concomitant head injuries. Alert patients might present upper cervical spine tenderness or neurological deficits such as lower cranial nerve palsies. Nearly one third of the patients (up to 80% in some case series) with an OCF suffer neurological symptoms. Within this group, another third present delayed deficits which might occur days or even weeks after the accident [11-14, 18, 19].
Demisch et al. report a case about a 45-year-old woman with a fracture of the right occipital condyle who showed no initial neurological symptoms but later developed hypoglossal nerve palsy 9 weeks after the incident, most likely caused by compression of the hypoglossus canal due to callus formation or subseqent dislocation of a bony fragment [20]. Unilateral paralysis of the cranial nerves IX through XII is referred to as the "Collet-Sicard-Syndrome" [16, 17, 19].
A CT scan of the cervicooccipital junction is necessary for reliable diagnosis. Plain radiographs of this region typically appear normal, although sometimes prevertebral soft tissue swelling and asymmetry of the odontoid peg may provide indications of injury [9, 13]. An MRI may be useful for determining the extent of soft tissue involvement, although it is of secondary importance [2, 5, 21].
In our case the patient complained of intense pain in the upper cervical spine with no neurological limitations. Due to the trauma mechanism, we performed a CT scan from head to pelvis which revealed the displaced fracture of the right occipital condyle. Despite the dislocation into the foramen magnum, the lack of neurological symptoms might be explained by the anatomy of the craniocervical junction, which extends wider than the lower cervical spinal canal [15]. The occipital condyle fractures are commonly classified after Anderson and Montesano [22]. A Type-I fracture results from axial loading causing a comminuted condylar fracture with little or no displacement.
Type-II describes a condylar fracture with extension into the base of the skull, Type-III is classified by the avulsion of a condyle at the alar ligament, resulting in an unstable fracture. Tuli et al. introduced an alternative management-based categorization system: Type-I is a non-displaced (i.e. stable) OCF with the ligaments still intact; Type-IIa is a displaced OCF with intact ligaments (stable) and Type-IIb describes displaced OCFs with radiological signs of ligament injury that are therefore unstable [23].
In general the treatment of OCF is conservative [3, 8, 11, 23, 24], using a hard collar or HALO vest for 6 to 12 weeks. Only the few patients who presented neurological symptoms, displaced fractures or additional fractures of the upper cervical spine underwent an operative internal fixation procedure [8, 24].
However, there are also cases reported where conservative treatment was preferred despite neurological symptoms [16, 17, 19, 20]. We discussed further treatment options after HALO stabilization and were mindful of the inherent risks of surgery.
5. Conclusion
After consultation of experts in the field and in accordance with the patient’s wishes we decided on an operative internal stabilization with fusion of C0/C1 and no repositioning of the displaced condyle (Option 3).
Our reasons for this course of action where manifold:
- A Type III (Anderson and Montesano) injury of the right occipital condyle is an unstable fracture, therefore internal fixation is recom-mended.
- Intraoperative radiographic navigation provi-ded a significantly more secure method for screw positioning.
- Internal stabilization and fusion might prev-ent further dislocation and possible neuro-logical consequences.
- C3 was included in the construction to provide additional stability; this approach was also described by Schnake et al. in 2012 [25].
- As the right C0/C1 joint was completely destroyed in the accident, we decided on a definite fusion of this joint, accepting the malposition and avoiding possible intra-operative risks of repositioning.
- To regain better range of motion for the upper cervical spine, we performed an imp-lant removal after 12 months.
Conflict of Interest
None.
References
- Alcelik I, Manik KS, Sian PS, et al. Occipital Condylar fractures. J Bone Joint Surg 88-B (2006): 665-669.
- Aulino JM, Tutt LK, Kaye JJ, et al. Occpital condyle fractures: clinical presentation and imaging findings in 76 patients. Emerg Rad 11 (2005): 342-347.
- Hanson JA, Deliganis AV, Baxter AB, et al. Radiologic and clinical spectrum of occipital condyle fractures: Retrospective review of 107 consecutive fractures in 95 patients. AJR 178 (2002): 1261-1268.
- Heinz BC, Textor J, Hansis M. Diagnostische Probleme bei Frakturen der okzipitalen Kondylen. Unfallchirurg 100 (1997): 100-104.
- Kandziora F, Schnake K, Hoffmann R. Verletzungen der oberen Halswirbelsäule, Teil 2: Knöcherne Verletzungen. Unfallchirurg 113 (2010): 1023-1041.
- Bertalanffy H, Seeger W. The dorsolateral, suboccipital, transcondylar approach to the lower clivus and anterior portion of the craniocervical junction. Neurosurgery 29 (1991): 815 -821.
- Bloom AI, Neemann Z, Slasky S, et al. Fracture of occipital condyles and associated craniocervical ligament injury: incidence, CT Imaging and implications. Clinical Radiology 52 (1997): 198 -202.
- Maserati MB, Stephens B, Zohny Z, et al. Occipital condyle fractures: clinical decision rule and surgical management. J Neurosurg Spine 11 (2009): 338-395.
- Mueller FJ, Fuechtmeier B, Kinner B, et al. Occipital condyle fractures. Prospective follow-up of 31 cases within 5 years at a level 1 trauma centre. Eur Spine J 21 (2012): 289-294.
- Caroli I, Rocchi G, Orlando ER, et al. Occipital Condyle fractures: report of five cases and literature review. Eur Spine J 14 (2005): 487-492.
- Malham GM, Ackland HM, Jones R, et al. Occipital condyle fractures: incidence and clinical follow up at level 1 trauma centre. Emerg Radiol 16 (2009): 291-297.
- Payer M, Delavelle J. Bilateral occipital condylar fracture. Case report about successful treatment with SOMI brace. Journal of Clinical Neuroscience 11 (2004): 211-214.
- Kelly A, Parrish R. Fracture of the occipital condyle: the forgotten part of the neck. J Accid Emerg Med 17 (2000): 220-228.
- Karam YR, Traynelis VC. Occipital condyle fractures. Neurosurgy 66 (2010): A56-A59.
- Leone A, Cerase A, Colosimo C, et al. Occipital condyle fractures: A review. Radiology 216 (2000): 635-644.
- Erol FS, Topsakal C, Kaplan M, et al. Collet Siccard Syndrome associated with occipital condyle fracture and epidural haematoma. Yonsei Med J 48 (2007): 120-123.
- Hashimoto T, Watanabe O, Takase M, et al. Collet Siccard Syndrome after Minor Head Trauma.Neurosurgy 23 (1998): 367-370.
- Cirak B, Akpinar G, Palaoglu S. Traumatic occipital condyle fractures. Neurosurg Rev 23 (2000): 161-164.
- Schroedel HM, Kestlmeier R, Trappe AE. Bilateral occipital condyle fracture: Report of two cases. Skull Base 12 (2002).
- Demisch S, Lindner A, Beck R, et al. The forgotten condyle: Delayed hypoglossal nerve palsy caused by fracture of the occipital condyle. Clinical Neurology and Neurosurgery 100 (1998): 44 - 45.
- Wasserberg J, Bartlett RJV. Occipital condyle fractures diagnosed by high -definition CT and coronal reconstructions. Neuroradiology 37 (1995): 370-373.
- Anderson PA, Montesano PX. Morphology and treatment of occipital condyle fractures. Spine (Phila Pa 1976) 13 (1988): 721-736.
- Tuli S, Tator CH, Fehlings MG, et al. Occipital condyle fractures. Neurosurgery 41 (1997): 368-377.
- Young WF, Rosenwasser RH, Getch C, et al. Diagnosis and management of occipital condyle fractures. Neurosurgery 34 (1994): 257-261.
- Schnake KJ, Pingel A, Scholz M, et al. Temporary occipito-cervical stabilization of a unilateral occipital condyle fracture. Eur Spine J 21 (2012): 2198-2202.
