The Role of Radiation Therapy in Recurrent Ovarian Cancer
Article Information
Yuichiro Hotta, Tamina Kino*, Hiroyuki Shigeta
Department of Obstetrics and Gynecology, Yokohama Municipal Citizen’s Hospital, 1-1 Mitsuzawanishi-cho, Kanagawa-ku, Yokohama 221-0855, Japan
*Corresponding Author: Tamina Kino, Department of Obstetrics and Gynecology, Yokohama Municipal Citizen’s Hospital, 1-1 Mitsuzawanishi-cho, Kanagawa-ku, Yokohama 221-0855, Japan
Received: 21 November 2021; Accepted: 12 December 2021; Published: 04 January 2022
Citation: Yuichiro Hotta, Tamina Kino, Hiroyuki Shigeta. The Role of Radiation Therapy in Recurrent Ovarian Cancer. Journal of Cancer Science and Clinical Therapeutics 6 (2022): 25-30.
Share at FacebookAbstract
Recent remarkable technological advances in radiation therapy made the way for stereotactic body RT (SBRT), which can be used for oligometastatic tumors anywhere in the body. Oligometastases from gynecological malignancies have been considered as one of the most promising candidate for SBRT. It is suggested that SBRT was associated with high rates of local control, impressive survival, and minimal toxicity in ovarian cancer. It is also suggested that SBRT serves to destroy chemoresistant tumor clones, and help stimulate innate immune response or expose tumor neoantigens, and can be used in women who have had prior radiotherapy.
Among the ovarian cancers, clear cell cancer might be a good candidate for radiation therapy because it is less sensitive to standard platinum-based chemotherapy. A patient was reported who had recurrent ovarian clear cell cancer and had been free from disease more than ten years after the discontinuation of proton beam therapy. Proton beam therapy provides superior dose distributions and a dosimetric advantages over photon beam therapy.
Therefore, radiation therapy is considered to be an effective and safe option for oligometastatic ovarian cancer patients. Proton beam therapy is a good potential option for chemotherapy-resistant, localized, recurrent ovarian cancer including clear cell cancer.
Keywords
Recurrent ovarian cancer; Clear cell cancer; Radiation therapy; Proton beam therapy
Recurrent ovarian cancer articles; Clear cell cancer articles; Radiation therapy articles; Proton beam therapy articles
Recurrent ovarian cancer articles Recurrent ovarian cancer Research articles Recurrent ovarian cancer review articles Recurrent ovarian cancer PubMed articles Recurrent ovarian cancer PubMed Central articles Recurrent ovarian cancer 2023 articles Recurrent ovarian cancer 2024 articles Recurrent ovarian cancer Scopus articles Recurrent ovarian cancer impact factor journals Recurrent ovarian cancer Scopus journals Recurrent ovarian cancer PubMed journals Recurrent ovarian cancer medical journals Recurrent ovarian cancer free journals Recurrent ovarian cancer best journals Recurrent ovarian cancer top journals Recurrent ovarian cancer free medical journals Recurrent ovarian cancer famous journals Recurrent ovarian cancer Google Scholar indexed journals Clear cell cancer articles Clear cell cancer Research articles Clear cell cancer review articles Clear cell cancer PubMed articles Clear cell cancer PubMed Central articles Clear cell cancer 2023 articles Clear cell cancer 2024 articles Clear cell cancer Scopus articles Clear cell cancer impact factor journals Clear cell cancer Scopus journals Clear cell cancer PubMed journals Clear cell cancer medical journals Clear cell cancer free journals Clear cell cancer best journals Clear cell cancer top journals Clear cell cancer free medical journals Clear cell cancer famous journals Clear cell cancer Google Scholar indexed journals Radiation therapy articles Radiation therapy Research articles Radiation therapy review articles Radiation therapy PubMed articles Radiation therapy PubMed Central articles Radiation therapy 2023 articles Radiation therapy 2024 articles Radiation therapy Scopus articles Radiation therapy impact factor journals Radiation therapy Scopus journals Radiation therapy PubMed journals Radiation therapy medical journals Radiation therapy free journals Radiation therapy best journals Radiation therapy top journals Radiation therapy free medical journals Radiation therapy famous journals Radiation therapy Google Scholar indexed journals Proton beam therapy articles Proton beam therapy Research articles Proton beam therapy review articles Proton beam therapy PubMed articles Proton beam therapy PubMed Central articles Proton beam therapy 2023 articles Proton beam therapy 2024 articles Proton beam therapy Scopus articles Proton beam therapy impact factor journals Proton beam therapy Scopus journals Proton beam therapy PubMed journals Proton beam therapy medical journals Proton beam therapy free journals Proton beam therapy best journals Proton beam therapy top journals Proton beam therapy free medical journals Proton beam therapy famous journals Proton beam therapy Google Scholar indexed journals laparotomy articles laparotomy Research articles laparotomy review articles laparotomy PubMed articles laparotomy PubMed Central articles laparotomy 2023 articles laparotomy 2024 articles laparotomy Scopus articles laparotomy impact factor journals laparotomy Scopus journals laparotomy PubMed journals laparotomy medical journals laparotomy free journals laparotomy best journals laparotomy top journals laparotomy free medical journals laparotomy famous journals laparotomy Google Scholar indexed journals tumor neoantigens articles tumor neoantigens Research articles tumor neoantigens review articles tumor neoantigens PubMed articles tumor neoantigens PubMed Central articles tumor neoantigens 2023 articles tumor neoantigens 2024 articles tumor neoantigens Scopus articles tumor neoantigens impact factor journals tumor neoantigens Scopus journals tumor neoantigens PubMed journals tumor neoantigens medical journals tumor neoantigens free journals tumor neoantigens best journals tumor neoantigens top journals tumor neoantigens free medical journals tumor neoantigens famous journals tumor neoantigens Google Scholar indexed journals Oligometastases articles Oligometastases Research articles Oligometastases review articles Oligometastases PubMed articles Oligometastases PubMed Central articles Oligometastases 2023 articles Oligometastases 2024 articles Oligometastases Scopus articles Oligometastases impact factor journals Oligometastases Scopus journals Oligometastases PubMed journals Oligometastases medical journals Oligometastases free journals Oligometastases best journals Oligometastases top journals Oligometastases free medical journals Oligometastases famous journals Oligometastases Google Scholar indexed journals gynecological malignancies articles gynecological malignancies Research articles gynecological malignancies review articles gynecological malignancies PubMed articles gynecological malignancies PubMed Central articles gynecological malignancies 2023 articles gynecological malignancies 2024 articles gynecological malignancies Scopus articles gynecological malignancies impact factor journals gynecological malignancies Scopus journals gynecological malignancies PubMed journals gynecological malignancies medical journals gynecological malignancies free journals gynecological malignancies best journals gynecological malignancies top journals gynecological malignancies free medical journals gynecological malignancies famous journals gynecological malignancies Google Scholar indexed journals stereotactic body RT articles stereotactic body RT Research articles stereotactic body RT review articles stereotactic body RT PubMed articles stereotactic body RT PubMed Central articles stereotactic body RT 2023 articles stereotactic body RT 2024 articles stereotactic body RT Scopus articles stereotactic body RT impact factor journals stereotactic body RT Scopus journals stereotactic body RT PubMed journals stereotactic body RT medical journals stereotactic body RT free journals stereotactic body RT best journals stereotactic body RT top journals stereotactic body RT free medical journals stereotactic body RT famous journals stereotactic body RT Google Scholar indexed journals chemotherapy articles chemotherapy Research articles chemotherapy review articles chemotherapy PubMed articles chemotherapy PubMed Central articles chemotherapy 2023 articles chemotherapy 2024 articles chemotherapy Scopus articles chemotherapy impact factor journals chemotherapy Scopus journals chemotherapy PubMed journals chemotherapy medical journals chemotherapy free journals chemotherapy best journals chemotherapy top journals chemotherapy free medical journals chemotherapy famous journals chemotherapy Google Scholar indexed journals
Article Details
1. Significance of Radiation Therapy for Ovarian Cancer
The initial management for ovarian cancer (OC) is a staging laparotomy/primary debulking surgery followed by either systemic chemotherapy or observation. Historically, adjuvant whole abdominal radiation therapy (RT) has been used; however, it should not be used to treat epithelial OC because it is unable to deliver a curative radiation dose to an entire anatomic region, with multiple dose-limits in normal tissues [1]. And it is clearly recommended for palliative settings, particularly in patients who fail chemotherapy.
In recent years, remarkable technological advances have been made in RT by incorporating new imaging modalities, sophisticated computers and software, and new delivery systems. Two-dimensional RT, based on plain radiography, has been largely replaced by three-dimensional RT based on CT imaging. Intensity-modulated RT allows the creation of irregularly shaped radiation doses that conform to the tumor while avoiding critical organs. Further advancement of this technique was achieved by volumetric modulated arc therapy, which allows even better dose conformity and further reduction of the treatment duration [2]. Image-guided RT enabled the integration of various imaging modalities directly into the linear accelerator, which resulted in daily monitoring of patient positioning, tumor position, and alterations in patient anatomy, allowing immediate detection of changes from the imaging findings at the planning stage and enabling modification of the irradiation procedure [3]. These advancements have enabled stereotactic body RT, which can be used for oligometastatic tumors anywhere in the body [4]. The concept of an oligometastatic state was first proposed by Hellman and Weichselbaum [5] as an intermediate state between limited primary lesions and polymetastatic cancers. Oligometastases from gynecological malignancies have been considered as one of the most promising candidates for stereotactic body RT. Kowalchuk et al. [6] studied OC patients treated with SBRT and concluded that SBRT was associated with high rates of local control, impressive survival, and minimal toxicity in ovarian cancer, especially with a median biologically efficient dose >35 Gy and treatment for lymph nodes. Furthermore, Fields et al. [7] demonstrated that SBRT destroys chemoresistant tumor clones, stimulates the innate immune response, exposes tumor neoantigens, and can be used in women who have had prior RT. Based on these results, clinicians should consider SBRT as an effective and safe option for patients with oligometastatic OC.
2. Radiation Therapy for Ovarian Clear Cell Cancer
Ovarian clear cell cancer (OCCC) is a histological subtype of epithelial OC with distinct behavior. OCCC is more likely to be detected at an early stage than high-grade serous cancers, and when confined within the ovary, the prognosis is good. However, advanced disease is associated with a very poor prognosis and resistance to standard treatments. Hogen et al. [8] studied 163 patients with stage I or II OCCC; 44 (27%) patients were treated with adjuvant RT and 119 (73%) had no adjuvant RT post-surgery. As a result, they did not find a progression-free or overall survival (OS) benefit for adjuvant RT. Roy et al. [9] compared the outcomes of patients with stage IC or II OCCC treated with adjuvant chemotherapy versus chemoradiotherapy. As a result, adjuvant chemotherapy was associated with a lower risk of failure compared to chemotherapy alone. However, there was no difference in the OS between both groups. Ogasawara et al. [10] concluded in their review that the efficacy of RT for OCCC is uncertain, and a prospective randomized controlled trial is required to evaluate adjuvant RT for high-risk early stage OCCC.
Brown et al. [11] evaluated the effectiveness of definitive involved-field RT in 102 selected patients with locoregional recurrent epithelial OC. Among them, they reported that eight OCCC patients had higher 5-year OS and progression-free survival rates than other patients. Westhoff et al. [12] studied 53 patients with recurrent OCCC. Twenty-four (45.3%) patients received RT. They found that RT was associated with improved survival. Furthermore, recurrent OCCC can be treated with curative intent if the relapse is solitary, and completely resected or encompassed with RT [13]. Therefore, RT may be unsuitable in adjuvant therapy but may be of use in locoregional recurrent OCCC.
3. Proton Beam Therapy for OC
Recent advancements in RT have enabled the use of heavy charged particles, including protons, neutrons, and heavy ions (i.e., helium, carbon, nitrogen, argon, and neon). Proton beam therapy (PBT) is the most common form of heavy charged particle RT for a variety of malignancies. It allows the delivery of high radiation doses to tumor cells and very low or zero doses to normal cells, which is recognized as an ideal treatment modality for malignant diseases, especially for organs-at-risk, with less toxicity. It is confirmed to be safe, precise, and efficient, with tolerable toxicity. However, its cost varies and building sites are required to install and maintain the PBT treatment machine.
A good PBT target is believed to be pediatric tumors, because the long-term side effects of RT, such as secondary malignancies and medical morbidity, can be reduced. For adult malignancies, possible good PBT targets were reported as follows: prostate cancer, uveal melanoma, chordoma and chondrosarcoma, breast cancer, lung cancer, brain tumors, head and neck cancers, and gastrointestinal malignancies [14]. In gynecologic neoplasms, the majority of patients who were treated with PBT had cervical cancer, although several cases of vaginal cancer and endometrial cancer were reported. We report a case of recurrent OCCC in the sigmoid colon that was successfully treated with PBT [15]. In this case, the recurrent tumor was solitary and PBT enabled the administration of a relatively high dose of 66 Gy to the target tumor. The irradiation field was reduced by three times to minimize damage to normal tissues, especially the small intestine (Figure 1). The patient has been disease-free for more than 10 years after discontinuation of PBT. Although only one case of recurrent OC was reported to be treated with PBT [15], PBT may be a potential option for chemotherapy-resistant, localized, recurrent OC. Patients with OCCC might be good candidates for PBT because OCCC is less sensitive to standard platinum-based chemotherapy [15].
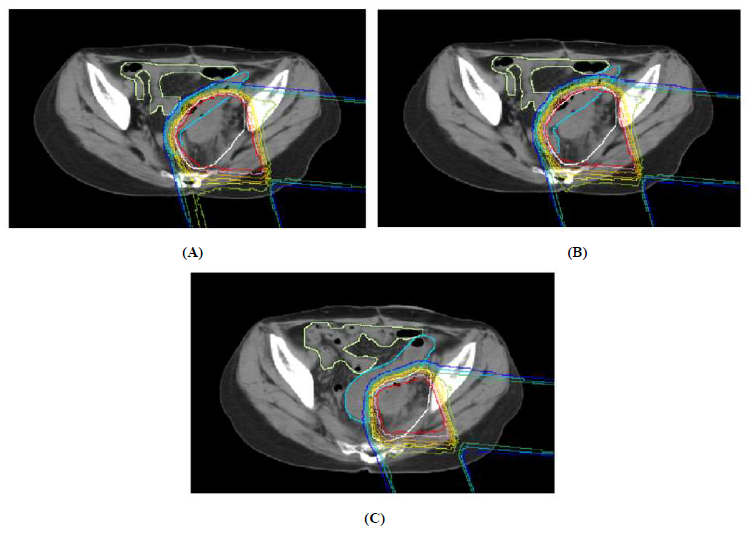
Figure 1A: Treatment plan of PBT with isodose distribution in axial view (A, 0-40 GyE; B, 42-48 GyE; C, 50-66 GyE).
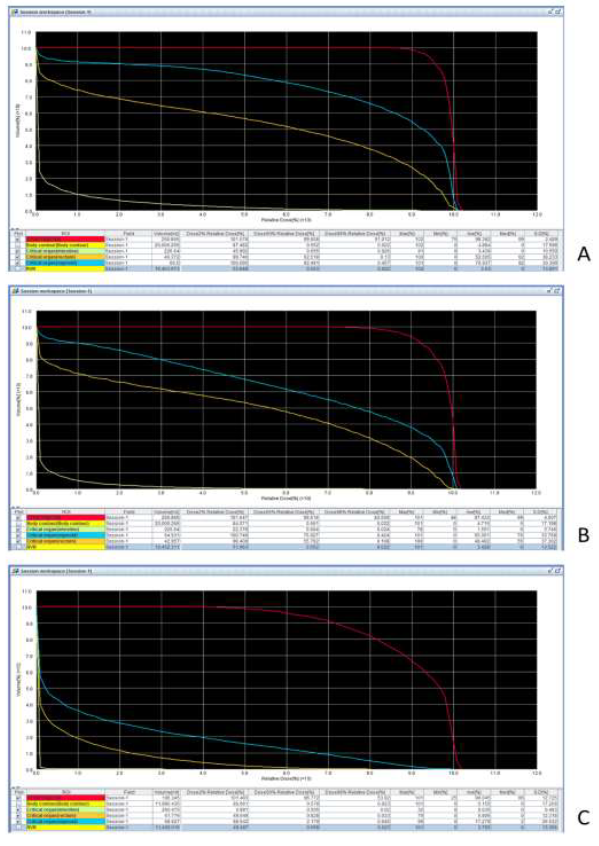
Figure 1B: Dose volume histogram of each PBT plan (A, 0-40 GyE; B, 42-48 GyE; C, 50-66 GyE; red: CTV; blue: sigmoid colon; yellow: rectum; green: small intestine).
Acknowledgement
We would like to thank Editage (www.editage.com) for English language editing.
Conflict of Interest
The authors declare no competing interest.
References
- Fabian A, Krug D, Alkatout I. Radiotherapy and Its Intersections with Surgery in the Management of Localized Gynecological Malignancies: A Comprehensive Overview for Clinicians. Journal of Clinical Medicine 10 (2021): 93.
- Boon IS, Au Yong TPT, Boon CS. Assessing the role of artificial intelligence (AI) in clinical oncology: Utility of machine learning in radiotherapy target volume delineation. Medicine (Basel) 5 (2018): 131.
- Sterzing F, Engenhart-Cabillic R, Flentje M, Debus J. Image-Guided Radiotherapy. Deutsches Ärzteblatt International 108 (2011): 274-280.
- Hanna GG, Landau D. Stereotactic body radiotherapy for oligometastatic disease. Clinical Oncology 27 (2015): 290-297.
- Hellman S, Weichselbaum RR. Oligometastases. Journal of Clinical Oncology 13 (1995): 8-10.
- Kowalchuk RO, Waters MR, Richardson KM, et al. Stereotactic body radiation therapy in the treatment of ovarian cancer. Radiation Oncology 15 (2020): 108.
- Fields EC, McGuire WP, Lin L, et al. Radiation Treatment in Women with Ovarian Cancer: Past, Present, and Future. Frontiers in Oncology 7 (2017): 177.
- Hogen L, Thomas G, Bernardini M, et al. The effect of adjuvant radiation on survival in early stage clear cell ovarian carcinoma. Gynecologic Oncology 143 (2016): 258-263.
- Roy S, Hoskins P, Tinker A, et al. Adjuvant Treatment of Early Ovarian Clear Cell Carcinoma: A Population-Based Study of Whole Abdominal Versus Pelvic Nodal Radiotherapy. Journal of National Comprehensive Cancer Network 19 (2020): 172-180.
- Ogasawara A, Sato S, Hasegawa K. Current and future strategies for treatment of ovarian clear cell carcinoma. Journal of Obstetrics and Gynaecological Research 46 (2020): 1678-1689.
- Brown AP, Jhingran A, Klopp AH, et al. Involved-Field Radiation Therapy for Locoregionally Recurrent Ovarian Cancer. Gynecologic Oncology 130 (2013): 300-305.
- Westhoff GL, Fuh KC, Longacre TA, et al. Radiation Therapy for Recurrent Clear-Cell Cancer of the Ovary. International Journal of Gynecological Cancer 26 (2016): 1608-1614.
- Huang H-J, Yang L-Y, Tung H-J, et al. Management and clinical outcomes of patients with recurrent/progressive ovarian clear cell carcinoma. Journal of the Formosan Medical Association 119 (2020): 793-804.
- Mitin T and Zietman AL. Promise and Pitfalls of Heavy-Particle Therapy. J Clin Oncol 32 (2014): 2855-2863.
- Kino T, Ando N, Ogawara Y, et al. Proton beam therapy for recurrent ovarian carcinoma: A case report. Journal of Obstetrics and Gynaecological Research 45 (2019): 1952-1956.
