The Adolfsson-Björnsson Activity Scale (ABAS) Improves Description of Patient Characteristics
Article Information
Lars Adolfsson1, Per Lundin1,2, Hanna Björnsson Hallgren1*
1Department of Biomedical and Clinical Sciencies, Division of Orthopedics, Linköping University, Sweden
2Department of Orthopedics, Västervik County Hospital, Sweden
*Corresponding author: Hanna Björnsson Hallgren, Department of Biomedical and Clinical Sciencies, Division of Orthopedics, Linköping University, Sweden
Received: 22 March 2022; Accepted: 29 March 2022; Published: 28 April 2022
Citation: Lars Adolfsson, Per Lundin, Hanna Björnsson Hallgren. The Adolfsson-Björnsson Activity Scale (ABAS) Improves Description of Patient Characteristics. Archives of Clinical and Biomedical Research 6 (2022): 408-417.
Share at FacebookAbstract
Background and purpose: Age and gender have been regarded important for surgical decision making and used as inclusion criteria for clinical trials. Individual demands and level of activity have been less considered. A self-administered scale, defining subjectively assessed level of activity involving the upper extremities was therefore developed. The primary purpose of this study was to present the scale. Secondarily to investigate its reliability and correlation with age and gender.
Patients and Methods: A scale with 8 categories ranging from extremely demanding to non-demanding activities, separated according to hand dominance, was constructed. Reliability testing was performed on 103 healthy individuals of both genders with a wide age range (20-86). 241 patients, median age 58 years (range 18-97), with different upper extremity injuries completed the scale. Participants were instructed to mark activities representative for their normal activity level. Correlation with age and gender was then investigated using Spearman Correlation Coefficient (SCC).
Results: The level of activity ranged from 1, corresponding to minimal use of the arm, to 8 defined as elite sports. For test-retest Intraclass Correlation Coefficient (ICC) was 0.89 for the dominant and 0.90 for the non-dominant arm. Correlations between gender, age and level of activity were weak.
Interpretation: The scale was found reliable and feasible to use. Age and gender were weakly correlated with level of activity and patients with low and high activities found in all ages and both genders. The activity scale allows improved description of patients included in clinical trials and can aid in treatment decision making but is primarily not intended for measurement of treatment outcome.
Keywords
Activity; Self-assessed; Subjective; Scale; Upper extremity; Gender; Age
Activity articles; Self-assessed articles; Subjective articles; Scale articles; Upper extremity articles; Gender articles; Age articles
Article Details
1. Introduction
Choosing the right treatment for the right patient can be challenging. Traditionally age, gender and radiological findings have been important factors in decision making of orthopedic treatments, especially in upper extremity surgery [1]. The outcome after injuries and disorders has often been assessed by one of many existing scores and measures such as range of motion, grip strength and pain scales [2]. Rarely has the patients’ own appreciation of the functional status been requested, perhaps because this is, by definition, subjective and therefore difficult to quantify and measure [3]. Individual subjective activity level has just recently been recognized as an important factor to consider in treatment of orthopedic injuries and to interpret expectations. The subjective activity level may also be used in research to describe a cohort of patients and as an explanatory variable of patients’ satisfaction [4]. In the new Swedish national guidelines for distal radius fracture treatment, activity level is pointed out as one of the most important factors for decision making [5]. A shoulder specific activity assessment scale has been described [6], but for self-assessment of the entire upper extremity we are not aware of any such instrument being presented. To capture the patient´s own appreciation of the level of activity before and after an injury or disorder affecting the entire upper extremity, we designed an activity scale. The primary purpose of this study was to present the new scale defining the subjective activity level of patients with upper extremity injuries or disorders. Secondary purposes were to investigate the reliability of the scale and its´ correlations with age and gender.
2. Patients and Methods
2.1 Design and evaluation of the activity scale
In 2012 the first author (LA), when preparing a study on wrist injuries, realized that patient satisfaction of the treatment was not only dependent on the type of injury, result of functional scores, gender, and age but also the patients´ functional demands. In order to better describe and understand how the patients used their extremity prior to the injury, a number of descriptions were collected involving both patients and healthy individuals. Finally, a list of 36 activities was compiled ranging from extremely hard work or elite level sports to no use of the arm.
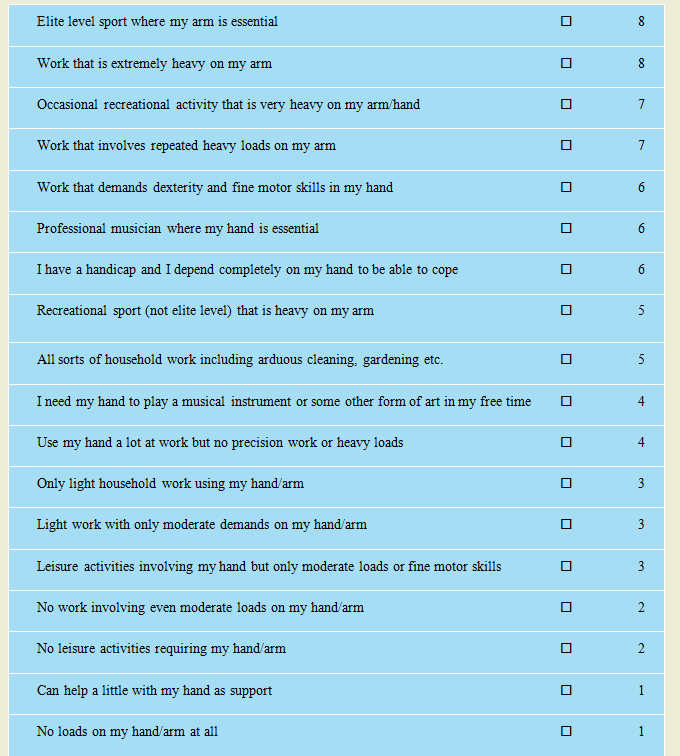
The list was then discussed with 8 healthy subjects, 4 of each gender, between the ages 19 and 84, and in consensus some of the items could be grouped together resulting in a list of 18 descriptions of activities. These were then categorized yielding 8 categories representing the scale values. The activities regarded as most demanding were given the category 8 and no use of the arm category 1. The scale was then adjusted to be used separately for the dominant and non-dominant arm and figures of the different categories were removed from the forms presented to the patients to reduce bias. 2 versions of the scale were produced, 1 intended for description of the situation before the injury or disorder to be treated (figure 1) and 1 for describing the current situation used for follow-ups in which the initial question was rephrased to ask about today’s status.
ABAS (Adolfsson Björnsson Activity Scale)
Mark the statements that best correspond with the activities you use your dominant arm for when you are healthy and uninjured: (dominant=right for right-handed, left for left-handed). You can mark several alternatives that apply.
The scale was translated into English for use by English speaking patients and for this publication according to a standard process [7]. The scale was translated into English, and then retranslated back into Swedish by 2 professional translators whose native language is Swedish.
The back-translation was then compared with the original version by a professional translator not involved in prior steps in the process and any discrepancies were resolved by a consensus discussion within the group of translators. Testing of criterion validity in relation to a standard reference was not done due to lack of a standard scale to compare with. Intra-rater reliability testing of the Swedish scale version was done using Intra Class Correlation (ICC) on 103 individuals, median age 48 years (range 20-86), 48 men and 55 women, all without any upper extremity complaints. They all completed the scale on 2 occasions with 2 weeks interval [8]. The individuals were patients with lower extremity disorders at any of the author’s orthopedic departments or individuals with some relation to the authors.
2.2 Patients
241 patients, median age 62 years (range 18-97), 88 men and 153 women completed the scale. They were patients with different upper extremity injuries identified when seeking care at any of the 3 including orthopaedic departments. 83 patients had a trauma-related rotator cuff tear, 55 were men and 28 women, median age 53 years (range 37–76). 103 patients had a proximal humeral fracture, 13 men and 90 women with median age 73 years (range 27–97). 55 patients with median age 62 years (range 18–86), 20 men and 35 women, had an elbow, forearm or a wrist fracture (table 1). The fracture patients completed the scale with 7–10 days recall after their injuries and the patients with rotator cuff tears before having surgery.
2.3 Use of the scale
Using the given alternatives in the scale, all patients were instructed to describe their subjective assessment of the individual level of activity before having sustained their respective injuries, both for the dominant and the non-dominant arm.
A short instruction of the purpose of the scale was given but no directions or guiding during completion and the number of chosen alternatives was unlimited. The highest category indicated in the scales was used as the maximum self-assessed level of activity for each patient.
2.4 Statistics
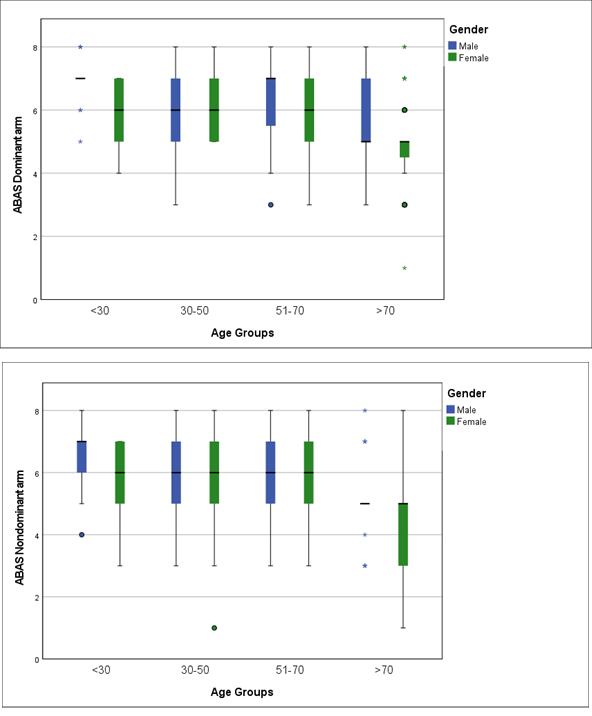
Descriptive statistics including mean and median values were used to describe the total cohorts’ age, gender and reported ABAS in the dominant and non-dominant arms. The study cohort was further divided by diagnosis and described with the same parameters. The total cohort was also divided into age groups (<30yr, 30-50yr, 51-70yr and >70yr) and by gender to investigate the relationship between ABAS, age and gender (figure 2a, 2b). Intra-rater reliability was calculated for non-injured individuals using ICC [8]. Based on the 95% confident interval of the ICC estimate, values between 0.75 and 0.90, and greater than 0.90 are indicative of, good and excellent reliability, respectively [9]. Calculations of correlations between ABAS, age, and gender in the total cohort and divided by the different diagnoses were done using Spearman correlation coefficient (SCC).
A coefficient of less than 0.10 was considered a negligible correlation, 0.10-0.39 weak, 0.40-0.69 moderate 0.70-0.89, strong correlation and 0.90-1.00 a very strong correlation [10, 11]. P-values of < 0.05 were considered statistically significant. All analyses were performed using SPSS for Windows IBM Statistics for Windows, Version 27, released 2020, IBM Corp.
|
Total study cohort (n) |
344 |
|
Gender, M/F (n) |
143/201 |
|
Age, median (range) |
58 (18-97) |
|
Activity level dominant arm, mean (range) |
5.9 (1-8) |
|
Activity level non-dominant arm, mean (range) |
5.6 (1-8) |
|
Study cohort divided by diagnosis: |
|
|
Proximal humeral fracture (n) |
103 |
|
Gender, M/F (n) |
13/90 |
|
Age, median (range) |
73 (27-97) |
|
Activity level dominant arm, mean (range) |
5.3 (1-8) |
|
Activity level non-dominant arm, mean (range) |
5.0 (1-8) |
|
Elbow, forearm and wrist fracture (n) |
55 |
|
Gender, M/F (n) |
20/35 |
|
Age, median (range) |
62 (18-86) |
|
Activity level dominant arm, mean (range) |
5.9 (3-8) |
|
Activity level non-dominant arm, mean (range) |
5.6 (3-8) |
|
Rotator cuff tears (n) |
83 |
|
Gender, M/F (n) |
55/28 |
|
Age, median (range) |
53 (37-76) |
|
Activity level dominant arm, mean (range) |
6.3 (3-8) |
|
Activity level non-dominant arm, mean (range) |
6.0 (3-8) |
|
Non injured individuals (n) |
103 |
|
Gender, M/F (n) |
48/55 |
|
Age, median (range) |
48 (20-86) |
|
Activity level dominant arm, mean (range) |
6.2 (3-8) |
|
Activity level non-dominant arm, mean (range) |
5.8 (3-8) |
n = number of patients; M=man; F=female
Table 1: The total number of patients in the study cohort including non-injured individuals. Age, gender and reported pre-injury activity level in the dominant and non-dominant arms. The study cohort also divided by diagnosis and their respective reported pre-injury activity level in the dominant and the non-dominant arm.
3. Results
All scale forms were understood by every patient without additional support, and fully completed. ABAS intra-rater reliability was good (ICC= 0.89) in the dominant arm and excellent (ICC=0.90) in the non-dominant arm. The mean ABAS value for the entire study cohort was 5.9 (range 1–8) for the dominant arm and 5.6 (range 1–8) for the non-dominant arm. As illustrated in figure 2a and 2b, a range from 1 to 8 in the rated activity level was found in the oldest age group (>70 years) and 3-8 in the other age groups. There was a weak but significant correlation between the scale value and age (dominant arm r=-0.33, non-dominant arm r=-0.35) and gender (dominant arm r=-0.15, non-dominant arm r=-0.14) in the total cohort (table 2). When dividing the cohort into diagnostic subgroups the correlations were still weak. In 6 out of 20 correlation analyses there was a non-significant p-value, see table 2, figure 2a and b.
|
Activity level dominant arm |
P -value |
Activity level non-dominant arm |
P -value |
|
|
Total study cohort (n=344) |
||||
|
Gender, M/F (143/201) |
-0.15 |
.004* |
-0.14 |
.008* |
|
Age, median 58 (range 18-97) |
-0.33 |
.001* |
-0.35 |
.001* |
|
Study cohort divided by diagnosis: |
||||
|
Proximal humeral fracture (n=103) |
||||
|
Gender, M/F (13/90) |
-0.10 |
.296 |
-0.09 |
.347 |
|
Age, median 73 (range 27-97) |
-0.40 |
.001* |
-0.39 |
.001* |
|
Elbow, forearm and wrist fracture (n=55) |
||||
|
Gender, M/F (20/35) |
-0.37 |
.005* |
-0.29 |
.031* |
|
Age, median 62 (range 18-86) |
-0.34 |
.010* |
-0.30 |
.025* |
|
Rotator cuff tear (n=83) |
||||
|
Gender, M/F (55/28) |
0.03 |
.774 |
0.02 |
.828 |
|
Age, median 53 (range 37-76) |
0.25 |
.026* |
0.19 |
.087 |
|
Healthy (n=103) |
||||
|
Gender, M/F (48/55) |
-0.21 |
.033* |
-0.12 |
.249 |
|
Age, median 48 (range 20-86) |
-0.20 |
.046* |
-0.26 |
.007* |
n = number of patients, m=men, f=female p – values < 0.05 considered significant
*= significant p-value reflecting a valid correlation analysis
Table 2: The correlation calculated with Spearman correlation coefficient between age, gender, and the reported pre-injury activity level in the dominant and the non-dominant arm in the total cohort and divided by diagnosis.
4. Discussion
This study demonstrates that this new subjective self-administered activity level scale comprising the entire upper extremity is reliable and feasible. It also demonstrates that self-assessed level of activity may vary considerably between seemingly homogenous patients if only age, gender and diagnosis are considered as background variables to describe a treatment group. This may have implications not only to explain patients´ satisfaction with the result of a given treatment but also for group comparisons between treatment alternatives. Patient expectation is testified to be an important factor to consider when evaluating treatment satisfaction [12]. If the desired level of activity cannot be regained after an injury and treatment, this may explain dissatisfaction of the treatment even if other often reported variables such as pain, range of motion and strength are considered acceptable. The activity scale described here is however not primarily intended as a tool to assess outcome but as an instrument to make treating physicians aware of patients’ diversity in preinjury activity and to ensure that randomized trials are based on truly comparable groups. As demonstrated by the recently published national guidelines for treatment of distal radius fractures, level of activity is recognized as an important factor to consider in tailoring the appropriate treatment and the activity scale presented here may serve as a tool to assess this and describe a patient cohort [5]. The potential impact of individual activity level has previously been recognized in treatment of anterior cruciate ligament injuries since it became evident that the outcome was dependent on the respective patients´ level of activity [13-15]. Brophy et al. (2009) described an activity scale exclusively for the shoulder and found that the reported level of activity correlated with age and the 3 included diagnoses, instability, rotator cuff disease and osteoarthritis [16]. In another study by Brophy et al. (2016) a correlation between socioeconomic factors and the level of activity was found and a slightly higher level for men than women attributed to both manual labor and sports [17]. In the present study of nearly 350 individuals, patients of both genders with an age range from 18-97; we found gender and age to be weakly correlated with different levels of activity in both arms. Our results, without strong correlation between age or gender, and level of activity, may be related to that we included a higher number of patients than Brophy et al. and all with diagnoses related to trauma. The results from a few of our calculations in the subgroup analyses did not have sufficient statistical power and should be interpreted with caution. Patient selection and different diagnoses might have influenced these analyses by uneven distribution of gender and ages. Most patients with proximal humeral fractures and distal radius fractures were for example females older than 70 years. This patient distribution is in accordance with the literature which mainly reports on older females meaning that the knowledge of men with these fractures is scarce [18-20]. Uneven age and gender distribution is also usually found in reports of rotator cuff tears where middle-aged men are over-represented, especially in trauma related tears [21,22]. The strength of the ABAS is that it is constructed to be used for the entire upper extremity and considers hand-dominance which potentially may influence activity level for individuals with specific demands. Further, the reliability testing was performed on individuals of both genders with a wide age range. The scale was found easy to use and understandable by the patients, but a potential weakness is that it is dependent on basic linguistic requirements. Content and criterion validity has not been possible to test since no comparable instrument has been found. The scale was intended as a tool for individual, subjective self-assessment and not for inter-individual or group comparisons. By adding the scale at follow up visits and comparing with preinjury rated activity level the scale may allow for improved interpretation of treatment results as well as serve as a tool in patient education to moderate expectations.
5. Conclusion
In conclusion the ABAS scale was found reliable and feasible to use. Age and gender were weakly correlated with the level of activity and patients with low and high activities were found in all ages and both genders. The activity scale allows improved description of patients included in clinical trials and can aid in treatment decision making.
Author’s Contributions
Lars Adolfsson: Designing the scale and the study. Data analyses and manuscripts writing.
Per Lundin: Data collection, data analysis and writing the manuscript. Corresponding author.
Hanna Björnsson Hallgren: Collecting data, analyses of data and manuscripts writing.
Ethics, Funding, and Potential Conflicts of Interest
The study was approved by the Swedish Ethical Review Authority DNR 2021-02964 and funded by the Regional Research Council in the Southeast region of Sweden. All participants received oral and written information of the study and informed consent was obtained. No conflict of interest exists for any of the authors, their immediate families, and any research foundations with which they are affiliated. None have received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgement
To Terez Zara Hanqvist for administrational work with data.
References
- Schumaier AP, Bedeir YH, Dines JS, Kenter K, Gulotta LV, Dines DM, et al. Quantifying the Impact of Patient-Specific Factors and Disease Severity on Clinical Decision Making in Cuff Tear Arthropathy: A Case-Based Survey. HSS journal : the musculoskeletal journal of Hospital for Special Surgery 15 (2019): 276-285.
- Harvie P, Pollard TC, Chennagiri RJ, Carr AJ. The use of outcome scores in surgery of the shoulder. The Journal of bone and joint surgery British volume 87 (2005): 151-154.
- Swiontkowski MF, Buckwalter JA, Keller RB, Haralson R. The outcomes movement in orthopaedic surgery: where we are and where we should go. The Journal of bone and joint surgery American volume 81 (1999): 732-740.
- Hawke LJ, Shields N, Dowsey MM, Choong PFM, Taylor NF. Physical activity levels after hip and knee joint replacement surgery: an observational study. Clinical Rheumatology 38 (2019): 665-674.
- se [Internet]. Swedish national guidlines on radius fractures (2021). Available from: https://d2flujgsl7escs.cloudfront.net/external/Nationellt+v%C3%A5rdprogram+f%C3%B6r+behandling+av+distala+radiusfrakturer.pdf
- Brophy RH, Beauvais RL, Jones EC, Cordasco FA, Marx RG. Measurement of shoulder activity level. Clinical orthopaedics and related research 439 (2005): 101-108.
- Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine 25 (2000): 3186-3191.
- Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. Journal of clinical epidemiology 60 (2007): 34-42.
- Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. Journal of chiropractic medicine 15 (2016): 155-163.
- Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J 24 (2012): 69-71.
- Schober P, Boer C, Schwarte LA. Correlation Coefficients: Appropriate Use and Interpretation. Anesthesia & Analgesia 126 (2018): 1763-1768.
- Swarup I, Henn CM, Gulotta LV, Henn RF, 3rd. Patient expectations and satisfaction in orthopaedic surgery: A review of the literature. J Clin Orthop Trauma 10 (2019): 755-60.
- Hambly K. The use of the Tegner Activity Scale for articular cartilage repair of the knee: A systematic review. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 19 (2010): 604-614.
- Saleh KJ, Mulhall KJ, Bershadsky B, Ghomrawi HM, White LE, Buyea CM, et al. Development and Validation of a Lower-Extremity Activity Scale: Use for Patients Treated with Revision Total Knee Arthroplasty. JBJS 87 (2005):1985-94.
- Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clinical orthopaedics and related research 198 (1985): 43-49.
- Brophy R, Levy B, Chu S, Dahm D, Sperling J, Marx R. Shoulder activity level varies by diagnosis. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 17 (2009): 1516-1521.
- Brophy RH, Lin KM, Skillington SA, Hepper CT, Smith MV. Shoulder Activity Level is Associated With Type of Employment and Income in the Normative Population Without Shoulder Disorders. Clinical orthopaedics and related research 474 (2016): 2269-2276.
- Fraser AN, Bjørdal J, Wagle TM, Karlberg AC, Lien OA, Eilertsen L, et al. Reverse Shoulder Arthroplasty Is Superior to Plate Fixation at 2 Years for Displaced Proximal Humeral Fractures in the Elderly: A Multicenter Randomized Controlled Trial. The Journal of bone and joint surgery American volume 102 (2020): 477-85.
- Hevonkorpi TP, Launonen AP, Huttunen TT, Kannus P, Niemi S, Mattila VM. Incidence of distal radius fracture surgery in Finns aged 50 years or more between 1998 and 2016 – too many patients are yet operated on? BMC musculoskeletal disorders 19 (2018): 70.
- Jonsson E, Ekholm C, Salomonsson B, Demir Y, Olerud P. Reverse total shoulder arthroplasty provides better shoulder function than hemiarthroplasty for displaced 3- and 4-part proximal humeral fractures in patients aged 70 years or older: a multicenter randomized controlled trial. Journal of shoulder and elbow surgery 30 (2021): 994-1006.
- Maher A, Leigh W, Brick M, Young S, Millar J, Walker C, et al. Gender, ethnicity and smoking affect pain and function in patients with rotator cuff tears. ANZ J Surg 87 (2017): 704-708.
- Ranebo MC, Björnsson Hallgren HC, Holmgren T, Adolfsson LE. Surgery and physiotherapy were both successful in the treatment of small, acute, traumatic rotator cuff tears: a prospective randomized trial. Journal of shoulder and elbow surgery 29 (2020): 459-470.