Temporary Uterine Artery Embolization Followed by Hysteroscopy to Treat a Case of Acquired Uterine Arteriovenous Malformation (UAVM): Case Report with Systematic Literature Review
Article Information
Catena U1, Romito I1*, Mastrovito S1, Iacobelli V1, Campolo F2, Ianieri MM1, Cina A3, Scambia G1
1Department of Woman, Child and Public Health, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy
2Department of Surgical Sciences, City of Health and Science, University of Torino, Torino, Italy
3Department of Radiology, A. Gemelli Policlinic IRCCS Foundation, Rome, Italy
*Corresponding Author: Dr. Romito Ilaria, Department of Woman, Child and Public Health, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy
Received: 11 April 2020; Accepted: 20 April 2020; Published: 29 April 2020
Citation:
Catena U, Romito I, Mastrovito S, Iacobelli V, Campolo F, Ianieri MM, Cina A, Scambia G. Temporary Uterine Artery Embolization Followed by Hysteroscopy to Treat a Case of Acquired Uterine Arteriovenous Malformation (UAVM): Case Report with Systematic Literature Review. Obstetrics and Gynecology Research 3 (2020): 095-118.
Share at FacebookAbstract
Objective: This paper provides information about conservative surgery to correct uterine arteriovenous malformations (UAVMs). The main objectives are to review the current literature on this subject and to share our very interesting and challenging case of UAVM. Our innovative surgical approach consisted in a combined method with temporary uterine artery embolization (UAE) plus hysteroscopic treatment.
Materials and Methods: A search of MEDLINE, EMBASE, Web of Sciences, Scopus, ClinicalTrial.gov, OVID and Cochrane Library was performed. Any type of study has been considered including case reports. We identify articles published from the inception to July 2019. Three hundred sixty-three articles were identified: 286 articles were excluded for any reason. Overall, 77 articles were incorporated for further assessment.
Results: Four surgical techniques have been employed to treat 125 cases of UAVMs: uterine artery embolization (UAE) (69.9%),dilatation and curettage (D&C) (10.4%), operative hysteroscopy (14.4%), uterine artery ligation (4%). Two patients (1.6%) underwent combined approach. Failed procedures which required a new treatment were twenty-one (16.8%). Forty-five pregnancies after surgical conservative management of UAVMs were reported.
Conclusion: UAVM is a rare condition. In literature, there is no gold standard of treatment. For young women who wish to preserve fertility, a conservative surgical management should be recommended. As in our case, using a resorbable agent to perform UAE permitted a normal restoration of the flow in the uterine artery after the hysteroscopic resection.
Keywords
Fertility, Hysteroscopy, Uterine arteriovenous malformation, Uterine artery embolization
Fertility articles Fertility Research articles Fertility review articles Fertility PubMed articles Fertility PubMed Central articles Fertility 2023 articles Fertility 2024 articles Fertility Scopus articles Fertility impact factor journals Fertility Scopus journals Fertility PubMed journals Fertility medical journals Fertility free journals Fertility best journals Fertility top journals Fertility free medical journals Fertility famous journals Fertility Google Scholar indexed journals Hysteroscopy articles Hysteroscopy Research articles Hysteroscopy review articles Hysteroscopy PubMed articles Hysteroscopy PubMed Central articles Hysteroscopy 2023 articles Hysteroscopy 2024 articles Hysteroscopy Scopus articles Hysteroscopy impact factor journals Hysteroscopy Scopus journals Hysteroscopy PubMed journals Hysteroscopy medical journals Hysteroscopy free journals Hysteroscopy best journals Hysteroscopy top journals Hysteroscopy free medical journals Hysteroscopy famous journals Hysteroscopy Google Scholar indexed journals Uterine arteriovenous malformation articles Uterine arteriovenous malformation Research articles Uterine arteriovenous malformation review articles Uterine arteriovenous malformation PubMed articles Uterine arteriovenous malformation PubMed Central articles Uterine arteriovenous malformation 2023 articles Uterine arteriovenous malformation 2024 articles Uterine arteriovenous malformation Scopus articles Uterine arteriovenous malformation impact factor journals Uterine arteriovenous malformation Scopus journals Uterine arteriovenous malformation PubMed journals Uterine arteriovenous malformation medical journals Uterine arteriovenous malformation free journals Uterine arteriovenous malformation best journals Uterine arteriovenous malformation top journals Uterine arteriovenous malformation free medical journals Uterine arteriovenous malformation famous journals Uterine arteriovenous malformation Google Scholar indexed journals Uterine artery embolization articles Uterine artery embolization Research articles Uterine artery embolization review articles Uterine artery embolization PubMed articles Uterine artery embolization PubMed Central articles Uterine artery embolization 2023 articles Uterine artery embolization 2024 articles Uterine artery embolization Scopus articles Uterine artery embolization impact factor journals Uterine artery embolization Scopus journals Uterine artery embolization PubMed journals Uterine artery embolization medical journals Uterine artery embolization free journals Uterine artery embolization best journals Uterine artery embolization top journals Uterine artery embolization free medical journals Uterine artery embolization famous journals Uterine artery embolization Google Scholar indexed journals angiography articles angiography Research articles angiography review articles angiography PubMed articles angiography PubMed Central articles angiography 2023 articles angiography 2024 articles angiography Scopus articles angiography impact factor journals angiography Scopus journals angiography PubMed journals angiography medical journals angiography free journals angiography best journals angiography top journals angiography free medical journals angiography famous journals angiography Google Scholar indexed journals surgical treatment articles surgical treatment Research articles surgical treatment review articles surgical treatment PubMed articles surgical treatment PubMed Central articles surgical treatment 2023 articles surgical treatment 2024 articles surgical treatment Scopus articles surgical treatment impact factor journals surgical treatment Scopus journals surgical treatment PubMed journals surgical treatment medical journals surgical treatment free journals surgical treatment best journals surgical treatment top journals surgical treatment free medical journals surgical treatment famous journals surgical treatment Google Scholar indexed journals pregnancy articles pregnancy Research articles pregnancy review articles pregnancy PubMed articles pregnancy PubMed Central articles pregnancy 2023 articles pregnancy 2024 articles pregnancy Scopus articles pregnancy impact factor journals pregnancy Scopus journals pregnancy PubMed journals pregnancy medical journals pregnancy free journals pregnancy best journals pregnancy top journals pregnancy free medical journals pregnancy famous journals pregnancy Google Scholar indexed journals miscarriage articles miscarriage Research articles miscarriage review articles miscarriage PubMed articles miscarriage PubMed Central articles miscarriage 2023 articles miscarriage 2024 articles miscarriage Scopus articles miscarriage impact factor journals miscarriage Scopus journals miscarriage PubMed journals miscarriage medical journals miscarriage free journals miscarriage best journals miscarriage top journals miscarriage free medical journals miscarriage famous journals miscarriage Google Scholar indexed journals cesarean delivery articles cesarean delivery Research articles cesarean delivery review articles cesarean delivery PubMed articles cesarean delivery PubMed Central articles cesarean delivery 2023 articles cesarean delivery 2024 articles cesarean delivery Scopus articles cesarean delivery impact factor journals cesarean delivery Scopus journals cesarean delivery PubMed journals cesarean delivery medical journals cesarean delivery free journals cesarean delivery best journals cesarean delivery top journals cesarean delivery free medical journals cesarean delivery famous journals cesarean delivery Google Scholar indexed journals vaginal articles vaginal Research articles vaginal review articles vaginal PubMed articles vaginal PubMed Central articles vaginal 2023 articles vaginal 2024 articles vaginal Scopus articles vaginal impact factor journals vaginal Scopus journals vaginal PubMed journals vaginal medical journals vaginal free journals vaginal best journals vaginal top journals vaginal free medical journals vaginal famous journals vaginal Google Scholar indexed journals
Article Details
1. Introduction
A uterine arteriovenous malformation (UAVM) is a vascular abnormal connection between arteries and veins of the uterus, which creates enlarged, tangled vessels with a fast and turbulent flow [1]. This abnormal structure results in a direct connection between arteries and veins, while they are normally linked by capillaries. UAVMs are considered as rare, and the real incidence is unknown: less than 1000 cases are described in literature [2-4]. UAVM can be congenital or acquired. The acquired form often follows a spontaneous abortion with subsequent dilation and curettage, an interruption of pregnancy, an endometrial carcinoma, or a gestational trophoblastic disease [5-6]. Generally, women present with severe and life-threatening vaginal bleeding despite the onset of medical therapy [7]. Explorative laparotomy or total hysterectomy were once the only possible way to diagnose UAVM, upon pathological examination. After that, angiography became the gold standard for diagnosis. Lately, ultrasonography with color Doppler has been widely used to obtain a reliable diagnosis [8-10]. Treatments for these conditions are far from being standardized and range between expectation management mainly based on medical therapy, to invasive approaches, such as conservative surgery (uterine arterial embolization, dilatation and curettage, operative hysteroscopy, uterine arteries ligation) or demolitive surgery (hysterectomy) [11]. The treatment of choice depends on various factors such as pregnancy desire and patients’ haemodynamic parameters [12]. There have been several reports of pregnancy after conservative management of UAVMs, that seems to be feasible and reassuring on selected patients [13, 14]. In this paper, we report a successful case of a UAVM conservative management with combined temporary UAE plus hysteroscopic resection and we perform a retrospective systematic review of the available literature with regard to the conservative surgical treatment of acquired UAVMs and the fertility outcomes.
2. Methods
2.1 Search strategy
The data research was conducted using the following databases MEDLINE, EMBASE, Web of Sciences, Scopus, ClinicalTrial.gov, OVID and Cochrane Library querying for all articles related to temporary uterine artery embolization, hysteroscopy and UAVM. We used a combination of the following Medical Subjects Heading (MeSH): ((uterine) OR pelvic) AND arteriovenous AND (malformation OR fistula OR cirsoid aneurysm) AND (curettage OR D and C OR surgical treatment OR hysteroscopy OR uterine artery embolization) AND (bleeding OR hemorrhage). A systematic review was therefore performed following the Preferred Reporting Items for Systematic reviews and Meta-Analyses “PRISMA” guidelines [15]. We have selected articles published from inception to June 2019. We screened those record titles and abstracts retrieved from our searches. All full-text manuscript reference lists were analyzed in order to find additional eligible studies. This process was performed collaboratively by 2 authors (IR, SM).
2.2 Eligibility criteria
Studies with patients with acquired UAVMs were considered for the inclusion. Case reports were included in the selection. No language restrictions were initially applied. To avoid duplication, studies describing the same study population were included only once. The inclusion criteria were as follows: papers referring to acquired UAVMs treated by conservative surgical management (UAE, D & C, hysteroscopy, uterine ligature). Papers with congenital non acquired AVMs were excluded from the review as well as article not in English language, conference papers.reviews, and studies with information overlapping another publication. Also, we excluded studies reporting medical treatments and/or demolitive surgery (hysterectomy) as first line treatment.
2.3 Data extraction
From each eligible paper, we extracted and tabulated the following clinical data: author’s name and year; age; gravidity and parity; symptoms at the diagnosis, previous uterine surgical treatments; surgical management, time of follow-up, rate of failed procedures and pregnancy outcomes. Since most of the papers were case reports, we did not conduct a meta-analysis of these studies. The flow chart of the search strategy and the selection process is shown in Figure 1.
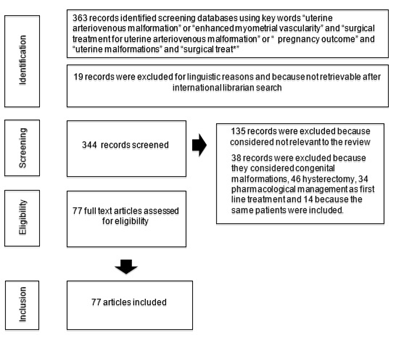
Figure 1: Study selection process.
3. Results
Our electronic database search revealed 363 articles of which 135 were excluded because they were after all, not relevant for the review, 19 records for linguistic reasons, 38 records because they included congenital AVMs, 46 records because they included demolitive surgery, 34 records because they included pharmacological management as first line treatment and 14 records because the same patients were included in latest records. Overall, 77 articles were incorporated for further assessment reporting 125 patients diagnosed with UAVM. The summary of all the papers is outlined in Table 1.
3.1 Patients characteristics
All patients were symptomatic and presented with acute abnormal vaginal bleeding, which was defined as severe. Mean age at diagnosis was 29.38 years, standard deviation (SD) was +/- 6.81 years (range 16-51). Among considered population, mean gravity and parity at the moment of the AVM diagnosis was respectively 2.34 years, SD+/- 1.68 years (range 0-8) and 1.02 years, SD +/- 1.10 years (range 0-5). Ninety-two patients (73.6%) presented with vaginal bleeding post interruption of pregnancy or spontaneous miscarriage. Twelve patients were (9.6%) diagnosed shortly after vaginal delivery and 4 (3.2%) after cesarean delivery; 1 patient (0.8%) presented after a diagnosis of chorioamnionitis. For 16 (12.8%) patients the cause of the UAVM remained unknown. Among all patients ninety-four patients (74%) underwent D&C before the occurrence of the UMAV.
3.2 Management and failed procedures
In terms of management, our search of current literature identified 85 patients that primarily underwent uterine artery embolization (69,6%) and this was the most common treatment option. Eighteen (14.4%) patients were treated with operative hysteroscopy. Five (4%) patients primarily had laparoscopic uterine artery ligation. Thirteen (10.4%) patients underwent D&C. Combined management was the treatment of choice for 2 (1.6%) patients. Of them, one (0.8 %) underwent UAE plus D&C, one (0.8%) had UAE plus operative hysteroscopy.
3.3 Failed procedures
Overall, failed procedures were 21 (16.8%): UAE was insufficient in 17 cases (19.5%). Among these patients fifteen (12%) required a second procedure and six (4.8%) had total abdominal hysterectomy performed due to uncontrolled bleeding (all among the UAE group). Of the patients treated by D&C and uterine ligation, 3 (2.4%) and 1 (0.8%), respectively, had a recurrence and required a second procedure. Two patients treated with combined method had no complications, and the procedures were successful.
3.4 Fertility outcomes
Follow-up data were available for 89 (71.2%) patients, with a mean follow-up of 22 months with SD +/- 11 (range 5-36). Follow-up data is described in table 2. Forty-five (50.6%) conceptions were observed, considering a positive blood beta-hcg. Delivery rate was 82.2% (37 patients). Four (10%) patients had a miscarriage. Four patients were lost to follow-up after positive b-hcg. Twenty-six patients had a term vaginal delivery. Six patients had a term caesarean section. Six patients reported obstetric complications such as pre-eclampsia, IUGR and pPROM. Twenty-eight patients with positive blood beta-hcg were reported after UAE.
|
Year |
Author |
Article Type |
N° |
Pt N° |
Age |
G |
P |
A |
Cause |
|||
|
1 |
1982 |
Forssman[1] |
case report |
1 |
20 |
2 |
0 |
1 |
D&C |
|||
|
2 |
1986 |
Brown[2] |
case report |
1 |
21 |
2 |
0 |
1 |
D&C |
|||
|
3 |
1986 |
Markoff[3] |
case report |
1 |
27 |
5 |
1 |
1 |
D&C |
|||
|
4 |
1987 |
Poppe[4] |
case report |
1 |
25 |
0 |
0 |
0 |
NS |
|||
|
5 |
1994 |
Ginsberg[5] |
case report |
1 |
42 |
2 |
1 |
1 |
D&C |
|||
|
6 |
1994 |
Manolitsas[6] |
case report |
1 |
21 |
3 |
1 |
1 |
D&C |
|||
|
7 |
1995 |
Chow[7] |
case report |
1 |
20 |
2 |
0 |
1 |
D&C |
|||
|
8 |
1996 |
Gaens[8] |
case report |
1 |
27 |
6 |
1 |
1 |
D&C |
|||
|
9 |
1997 |
Palmeri[9] |
case report |
1 |
16 |
1 |
0 |
1 |
D&C |
|||
|
10 |
1997 |
Hoffman[10] |
case series |
2 |
||||||||
|
1 |
24 |
2 |
0 |
1 |
D&C |
|||||||
|
2 |
21 |
1 |
0 |
1 |
D&C |
|||||||
|
11 |
1997 |
Arredondo-Soberon[11] |
case report |
1 |
33 |
3 |
0 |
1 |
NS |
|||
|
12 |
2001 |
Elia[12] |
case report |
1 |
29 |
6 |
3 |
1 |
D&C |
|||
|
13 |
2002 |
Kwon[13] |
case report |
1 |
26 |
2 |
1 |
1 |
D&C |
|||
|
14 |
2003 |
Gopal[14] |
case report |
1 |
42 |
6 |
0 |
1 |
D&C |
|||
|
15 |
2003 |
Takeuchi[15] |
case report |
1 |
29 |
3 |
0 |
1 |
D&C |
|||
|
16 |
2003 |
Chia[16] |
case report |
1 |
37 |
3 |
2 |
1 |
D&C |
|||
|
17 |
2003 |
Clarke[17] |
case report |
1 |
29 |
4 |
1 |
1 |
D&C |
|||
|
18 |
2003 |
Kelly[18] |
case report |
1 |
36 |
1 |
1 |
0 |
D&C |
|||
|
19 |
2003 |
Pope[19] |
case report |
1 |
19 |
2 |
1 |
1 |
D&C |
|||
|
20 |
2003 |
Chan[20] |
case report |
1 |
33 |
3 |
2 |
1 |
D&C |
|||
|
21 |
2003 |
Chen[21] |
case report |
1 |
51 |
3 |
2 |
1 |
D&C |
|||
|
22 |
2004 |
Winsor[22] |
case report |
1 |
30 |
1 |
0 |
1 |
D&C |
|||
|
23 |
2004 |
Batch[23] |
case report |
1 |
28 |
1 |
1 |
0 |
VD |
|||
|
24 |
2004 |
Irikoma[24] |
case report |
1 |
28 |
1 |
0 |
1 |
D&C |
|||
|
25 |
2004 |
Neto[25] |
case report |
1 |
21 |
1 |
0 |
1 |
D&C |
|||
|
26 |
2004 |
Aziz[26] |
case report |
1 |
30 |
1 |
0 |
1 |
D&C |
|||
|
27 |
2004 |
Amagada[27] |
case report |
1 |
17 |
1 |
0 |
1 |
D&C |
|||
|
28 |
2004 |
Nikolopoulous[28] |
case report |
1 |
39 |
1 |
0 |
1 |
D&C |
|||
|
29 |
2005 |
Ahn[29] |
case report |
1 |
37 |
3 |
1 |
1 |
D&C |
|||
|
30 |
2005 |
Ghi[30] |
case report |
1 |
29 |
1 |
1 |
0 |
VD |
|||
|
31 |
2006 |
Mccormick[31] |
case report |
1 |
21 |
0 |
0 |
0 |
NS |
|||
|
32 |
2006 |
Yahi-Mounta- sser[32] |
case report |
1 |
31 |
7 |
3 |
1 |
D&C |
|||
|
33 |
2006 |
Morikawa[33] |
case report |
1 |
39 |
8 |
3 |
1 |
D&C |
|||
|
34 |
2006 |
Phoon[34] |
case report |
1 |
31 |
1 |
0 |
1 |
D&C |
|||
|
35 |
2006 |
Delotte[35] |
case report |
1 |
33 |
2 |
1 |
1 |
D&C |
|||
|
36 |
2007 |
Lin[36] |
case report |
1 |
28 |
4 |
3 |
1 |
D&C |
|||
|
37 |
2007 |
Halperin[37] |
case series |
3 |
||||||||
|
1 |
27 |
2 |
1 |
1 |
D&C |
|||||||
|
2 |
24 |
3 |
0 |
1 |
D&C |
|||||||
|
3 |
28 |
4 |
1 |
1 |
D&C |
|||||||
|
38 |
2007 |
Rangarajan[38] |
case report |
1 |
22 |
2 |
0 |
1 |
D&C |
|||
|
39 |
2008 |
Bae[39] |
case report |
1 |
35 |
NS |
NS |
NS |
NS |
|||
|
40 |
2008 |
Bagga[40] |
case report |
1 |
24 |
2 |
1 |
1 |
D&C |
|||
|
41 |
2008 |
Dar[41] |
case report |
1 |
28 |
1 |
1 |
0 |
||||
|
42 |
2008 |
Bamberg[42] |
case report |
1 |
31 |
0 |
0 |
0 |
||||
|
43 |
2008 |
Singh[43] |
case report |
1 |
21 |
2 |
1 |
1 |
D&C |
|||
|
44 |
2008 |
Maldonado[44] |
case report |
1 |
21 |
1 |
D&C |
|||||
|
45 |
2009 |
Griffin[45] |
case report |
1 |
25 |
1 |
1 |
0 |
||||
|
46 |
2009 |
Taylor[46] |
case report |
1 |
37 |
3 |
1 |
1 |
D&C |
|||
|
47 |
2009 |
Vilos[47] |
case report |
1 |
19 |
1 |
0 |
1 |
D&C |
|||
|
48 |
2009 |
Wijesekera[48] |
case report |
1 |
27 |
1 |
0 |
1 |
D&C |
|||
|
49 |
2010 |
Guo[49] |
case report |
1 |
18 |
0 |
0 |
0 |
||||
|
50 |
2010 |
Kim[50] |
case series |
2 |
||||||||
|
35 |
4 |
2 |
1 |
D&C |
||||||||
|
20 |
1 |
0 |
1 |
D&C |
||||||||
|
51 |
2010 |
Wani[51] |
case report |
1 |
37 |
|||||||
|
52 |
2010 |
Przybojews-ki[52] |
case report |
1 |
21 |
|||||||
|
53 |
2011 |
Shaba[53] |
case report |
2 |
||||||||
|
1 |
30 |
1 |
1 |
D&C |
||||||||
|
2 |
45 |
4 |
0 |
1 |
D&C |
|||||||
|
54 |
2011 |
Vaknin[54] |
observational |
16 |
||||||||
|
1 |
27 |
2 |
1 |
1 |
D&C |
|||||||
|
2 |
24 |
3 |
0 |
1 |
D&C |
|||||||
|
3 |
27 |
1 |
1 |
0 |
CS |
|||||||
|
4 |
28 |
4 |
1 |
1 |
D&C |
|||||||
|
5 |
35 |
6 |
5 |
1 |
D&C |
|||||||
|
6 |
20 |
3 |
1 |
0 |
CS |
|||||||
|
7 |
36 |
5 |
4 |
0 |
VD |
|||||||
|
8 |
36 |
5 |
2 |
1 |
D&C |
|||||||
|
9 |
20 |
2 |
0 |
1 |
D&C |
|||||||
|
10 |
29 |
6 |
3 |
1 |
D&C |
|||||||
|
11 |
32 |
1 |
1 |
0 |
CS |
|||||||
|
12 |
31 |
4 |
3 |
1 |
D&C |
|||||||
|
13 |
29 |
3 |
2 |
0 |
CS |
|||||||
|
14 |
41 |
4 |
3 |
1 |
D&C |
|||||||
|
15 |
39 |
8 |
3 |
1 |
D&C |
|||||||
|
16 |
31 |
1 |
0 |
1 |
D&C |
|||||||
|
55 |
2012 |
Scioscia[55] |
case report |
1 |
/ |
36 |
1 |
0 |
1 |
D&C |
||
|
56 |
2012 |
Clarke[56] |
case report |
1 |
23 |
1 |
0 |
1 |
D&C |
|||
|
57 |
2012 |
Levy-Zauber- mann[57] |
case report |
1 |
29 |
3 |
2 |
0 |
D&C |
|||
|
58 |
2013 |
Chittawar[58] |
case report |
1 |
36 |
3 |
2 |
0 |
D&C |
|||
|
59 |
2013 |
Sharma[59] |
case report |
1 |
25 |
2 |
1 |
1 |
VD |
|||
|
60 |
2014 |
Woodhams[60] |
case series |
2 |
||||||||
|
1 |
33 |
1 |
D&C |
|||||||||
|
2 |
30 |
1 |
1 |
0 |
Chorioamniotitis |
|||||||
|
61 |
2015 |
Aslan[61] |
case report |
1 |
27 |
2 |
1 |
1 |
D&C |
|||
|
62 |
2015 |
Vilos[62] |
case series |
5 |
||||||||
|
1 |
19 |
1 |
0 |
1 |
D&C |
|||||||
|
2 |
32 |
3 |
1 |
1 |
D&C |
|||||||
|
3 |
30 |
1 |
0 |
1 |
D&C |
|||||||
|
4 |
18 |
1 |
1 |
0 |
VD |
|||||||
|
5 |
32 |
2 |
2 |
|||||||||
|
63 |
2015 |
Tullius[63] |
case report |
1 |
37 |
D&C |
||||||
|
64 |
2016 |
Calzolari[64] |
retrospective |
11 |
||||||||
|
1 |
18 |
1 |
0 |
1 |
D&C |
|||||||
|
2 |
28 |
2 |
0 |
1 |
D&C |
|||||||
|
3 |
37 |
2 |
1 |
1 |
D&C |
|||||||
|
4 |
23 |
2 |
1 |
1 |
D&C |
|||||||
|
5 |
44 |
2 |
1 |
1 |
D&C |
|||||||
|
6 |
26 |
2 |
1 |
1 |
D&C |
|||||||
|
7 |
30 |
1 |
0 |
1 |
D&C |
|||||||
|
8 |
34 |
2 |
1 |
1 |
D&C |
|||||||
|
9 |
21 |
1 |
0 |
1 |
D&C |
|||||||
|
10 |
32 |
2 |
1 |
1 |
D&C |
|||||||
|
11 |
31 |
1 |
1 |
0 |
VD |
|||||||
|
65 |
2017 |
Bandura[65] |
case series |
14 |
||||||||
|
1 |
25 |
1 |
1 |
0 |
VD |
|||||||
|
2 |
40 |
3 |
2 |
1 |
D&C |
|||||||
|
3 |
39 |
1 |
1 |
0 |
VD |
|||||||
|
4 |
25 |
2 |
1 |
0 |
VD/D&C |
|||||||
|
5 |
31 |
1 |
1 |
0 |
VD |
|||||||
|
6 |
30 |
2 |
2 |
0 |
VD/D&C |
|||||||
|
7 |
28 |
5 |
4 |
1 |
D&C |
|||||||
|
8 |
34 |
3 |
2 |
1 |
D&C |
|||||||
|
9 |
35 |
2 |
1 |
1 |
D&C |
|||||||
|
10 |
36 |
3 |
0 |
1 |
D&C |
|||||||
|
11 |
34 |
5 |
3 |
1 |
D&C |
|||||||
|
12 |
25 |
2 |
0 |
1 |
D&C |
|||||||
|
13 |
31 |
1 |
0 |
1 |
D&C |
|||||||
|
14 |
27 |
1 |
0 |
1 |
D&C |
|||||||
|
66 |
2017 |
Lehrman[66] |
case report |
1 |
23 |
3 |
0 |
1 |
D&C |
|||
|
67 |
2017 |
Evans[67] |
case report |
1 |
33 |
|||||||
|
68 |
2017 |
Ho[68] |
case report |
3 |
||||||||
|
1 |
22 |
3 |
3 |
1 |
||||||||
|
2 |
38 |
0 |
3 |
|||||||||
|
3 |
34 |
1 |
0 |
1 |
||||||||
|
69 |
2018 |
Wee[69] |
1 |
22 |
1 |
1 |
0 |
VD |
||||
|
70 |
2018 |
El agwany[70] |
case report |
1 |
38 |
3 |
3 |
0 |
CS |
|||
|
71 |
2018 |
Bettaiah[71] |
case report |
1 |
22 |
2 |
1 |
1 |
D&C |
|||
|
72 |
2018 |
Schwartz[72] |
case report |
1 |
37 |
|||||||
|
73 |
2018 |
Kaouther[73] |
case report |
1 |
28 |
4 |
2 |
1 |
RPOC (retained product of conception) |
|||
|
74 |
2019 |
Guida[74] |
case report |
1 |
28 |
2 |
0 |
1 |
||||
|
75 |
2019 |
Da joung[75] |
case report |
1 |
37 |
1 |
D&C |
|||||
|
76 |
2019 |
Kim[76] |
case report |
1 |
20 |
1 |
0 |
1 |
D&C |
|||
|
77 |
2019 |
Khan[77] |
case report |
1 |
30 |
1 |
0 |
1 |
D&C |
|||
Table 1: Demographics.
Table 2: Diagnosis, management and obstetric outcomes.
4. Case Report
A 33-year-old woman (IG 0P) with no relevant clinical history was referred in February 2019 to our gynaecology department after a miscarriage at 21 weeks of gestation, treated by evacuation with aspiration and curettage. After persistent uterine bleeding she started therapy with acetate norethisterone and tranexamic acid. In april 2019 she was admitted to our department due to secondary anemia requiring blood transfusion. The level of haemoglobin concentration decreased from 12.7 gr/dL to 7.2 gr/dL. Transvaginal ultrasonographic evaluation (2D and 3D scan) showed an anteverted uterus of 82x41x57mm and a thickened endometrium of 16mm. The uterine cavity was occupied by a hypervascular region on the posterior uterine wall of 21x16 mm, colour score 4, with a PSV > 100 cm/s (Figure 2). The b-hcg value was negative. Ovaries and cervix were normal. Based on clinical and imaging findings, a uterine arteriovenous malformation (UAVM) was considered. After multidisciplinary agreement, the patient underwent a computed tomography angiography (CTA) that confirmed the presence of a mass located between the endometrium and the myometrium with contrast enhancement (intense captation during arterial phase and early venous drainage) confirming the suspect of UAVM (Figure 3). The procedure was followed by a right uterine artery embolization with reabsorbable agent (Spongostan) (Figure 4) to decrease the ongoing vaginal bleeding and reduce the possible successive risk of intraoperative blood loss. Access through the right common femoral artery was performed, permitting the selective catheterization of hypogastric artery and of the right uterine artery. Spongostan was used to perform temporary UAE also in order to protect the ovary from permanent ischemic damage. There were no post-operative complications. After 24 hours from the UAE a second transvaginal ultrasound showed absence of hematic flow after the UAE . The uterine cavity was still enlarged by clots and the presence of hyperechoic lesion of mm13x14 (Figure 5). In the same day the patient underwent the hysteroscopic treatment. Hysteroscopy was performed with vaginoscopic approach, with a 5-mm diameter continuous-flow hysteroscope with oval profile, a 30° fore-oblique telescope and a 5 Fr operating channel (Office Continuous Flow Operative Hysteroscopy ‘size 5’; Karl Storz, Tuttlingen, Germany). Saline solution (NaCl 0.9%) was used as distension medium, which was provided through an electronic system of irrigation and aspiration (Endomat; Karl Storz, Tuttlingen, Germany). A stable intrauterine pressure of about 40 mmHg was obtained. The hysteroscopic view showed the uterine cavity filled with haemorrhagic material as well as parenchymatous material. The surgeon decided to undergo hysteroscopic resection using a bipolar 15 Frresectoscope (bipolar 15Fr office resectoscope; Karl Storz, Tuttlingen, Germany). The procedure was safe and successful (Figure 6). No post-operative complications were reported and resulted in a complete absence of symptoms. One month after surgery a normal menstrual cycle was restored and the ultrasonography showed a restoration of right uterine artery flow (Figure 7).
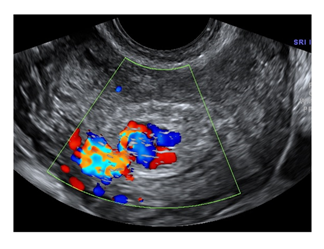
Figure 2: Hypervascular lesion into the uterine cavity.
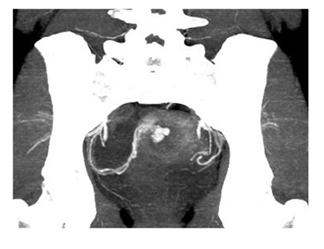
Figure 3: Computed tomography angiography (CTA).
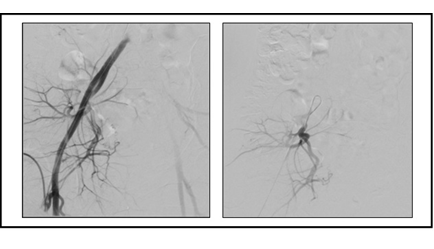
Figure 4: Selective embolization of right uterine artery with Spongostan.
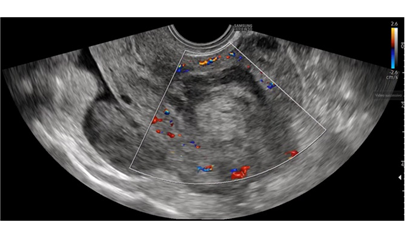
Figure 5: US view of hyperechoic lesion after temporary UAE.
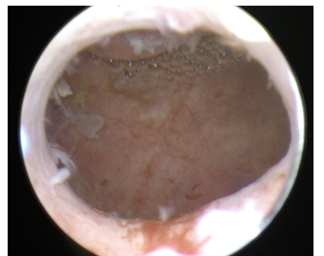
Figure 6: Uterine cavity after procedure.
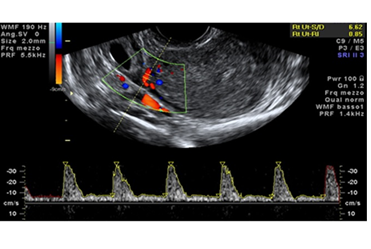
Figure 7: Restoration of right uterine artery flow.
5. Discussion
UAVM is a very rare condition but potentially life-threating. This paper described a case of UAVM treated by temporary UAE plus hysteroscopy and provided a systematic review of current available literature on UAVM conservative surgical management. UAVMs often occur in woman who previously underwent D&C, probably because the intrauterine trauma is involved in the pathogenesis of the disease [16]. This review confirmed this trend, as we found 74.4% patients with a acquired UMAV diagnosis after IVG o D&C for spontaneous miscarriage. Until not so long ago, the gold standard treatment was hysterectomy [17]. However, such a demolitive management is no longer acceptable, especially with stable hemodynamic conditions in young women. Among the conservative management, UAE was the most used but literature showed that UAE treatment alone is often not successful [18]. In fact, our series presented 19.5% failed UAE that required either further procedure. Among these patients, 6.9% had heavy recurrence of bleeding that lead to hysterectomy. Only 2 cases of combined surgical strategy were reported in available literature (UAE plus D&C and UAE plus hysteroscopy) in cases of UAVMs [54,75]. To our knowledge, this case report is the first to describe a combined method with temporary UAE and hysteroscopy. In fact, in our case, the UAE was performed with Spongostan that has an absorption time of only 15 days. This permitted a safe hysteroscopic treatment avoiding in the same time the subsequent ischemic damage. The use of UAE with no resorbable agent reduce definitively the blood flow to the uterus. Despite the presence of collateral vessels the reduction of the flow could create problems in subsequent pregnancies [20]. Moreover, it is still reported an increased incidence of miscarriage and stillbirth in pregnancy after UAVM embolization [20], which could be explained by a reduction of the uterine flow. Using of resorbable agent for the UAE could avoid this consequence. In any case there have been several case studies of pregnancy after conservative management of UAVMs. In fact, our review shows 45 cases of pregnancies, most of them after UAE treatment. Although we performed a systematic review our paper suffers of the lack of RCTs. Most papers are case reports and this does not allow a methodological analysis of the results. After all, we share a rare UAVM management with a combined method (UAE plus hysteroscopy) and for the first time the UAE is performed with a resorbable agent. In the same fashion the systematic review is the first one that report data only about conservative surgery.
6. Conclusions
In conclusion, UAVMs are very rare life-threatening lesions. There is not a gold standard of treatment. Conservative surgery management should be proposed to young women with pregnancy desire in stable hemodynamical conditions. Using a resorbable agent to perform UAE permitted a normal restoration of the flow in the uterine artery after the hysteroscopic resection but it needs RCT to have solid results about surgical and fertility outcomes.
Acknowledgements
Nothing to declare
Disclosure
Nothing to declare
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- Forssman L, Lundberg, J, Schersten T. Conservative treatment of uterine arteriovenous fistula. Acta Obstet. Gynecol. Scand 61 (1982): 85-87.
- Brown, R. L., Van Moore, A. & Smythe, A. R. Arteriographic management of uterine arteriovenous fistula. Am. J. Obstet. Gynecol 155 (1986): 491-493.
- Markoff G, Quagliarello J, Rosen R J, e al. Uterine arteriovenous malformation successfully embolized with a liquid polymer, isobutyl 2-cyanoacrylate. Am. J. Obstet. Gynecol 155 (1986): 659-660.
- Poppe W, Van Assche F A, Wilms G, et al. Pregnancy after transcatheter embolization of a uterine arteriovenous malformation. Am. J. Obstet. Gynecol 156 (1987): 1179-1180.
- Ginsberg N A, Hammer R, Parihk S, et al. Arteriovenous malformation of the uterus associated with a missed abortion. Ultrasound Obstet. Gynecol 4 (1994): 235-237.
- Manolitsas T, Hurley V, Gilford E. Uterine arteriovenous malformation--a rare cause of uterine haemorrhage. Aust. N. Z. J. Obstet. Gynaecol 34 (1994): 197-199.
- Chow T W, Nwosu E C, Gould D A, et al. Pregnancy following successful embolisation of a uterine vascular malformation. Br. J. Obstet. Gynaecol 102 (1995): 166-168.
- Gaens J, Desnyder L, Raat H, et al. Selective transcatheter embolization of a uterine arteriovenous malformation with preservation of the reproductive capacity. J. Belge Radiol 79 (1996): 210-211.
- Palmeri C, Ezenagu L, Norwick M, et al. Conservative Treatment of a Uterine Arteriovenous Malformation: A Case Report and Literature Review. Female Pelvic Med. Reconstr. Surg 3 (1997).
- Hoffman M K, Meilstrup J W, Shackelford D P, et al. Arteriovenous malformations of the uterus: an uncommon cause of vaginal bleeding. Obstet. Gynecol. Surv 52 (1997): 736-740.
- Scutiero G, Iafelice I, Greco P, et al. Acquired uterine arteriovenous malformation: management and treatment. Italian Journal of Gynaecology & Obstetrics 31 (2019).
- Elia G, Counsell C, Singer S J. Uterine artery malformation as a hidden cause of severe uterine bleeding. A case J. Reprod. Med 46 (2001): 398-400.
- Kwon J H, Kim G S. Obstetric iatrogenic arterial injuries of the uterus: diagnosis with US and treatment with transcatheter arterial embolization. Radiographics 22 (2002): 35-46.
- Gopal M, Goldberg J, Klein T A, et al. Embolization of a uterine arteriovenous malformation followed by a twin pregnancy. Obstet. Gynecol 102 (2003): 696-698.
- Takeuchi K, Yamada T, Iwasa M, et al. Successful medical treatment with danazol after failed embolization of uterine arteriovenous malformation. Obstet. Gynecol 102 (2003): 843-844.
- Chia Y N, Yap C, Tan B S. Pregnancy following embolisation of uterine arteriovenous malformation--a case report. Ann. Acad. Med. Singapore 32 (2003): 658-660.
- Clarke M J, Mitchell P J. Uterine arteriovenous malformation: a rare cause of uterine bleeding. Diagnosis and treatment. Australas. Radiol 47 (2003): 302-305.
- Kelly S M, Belli A M, Campbell S. Arteriovenous malformation of the uterus associated with secondary postpartum hemorrhage. Ultrasound Obstet. Gynecol 21 (2003): 602-605.
- Pope S L, Fleischer A C, Bream P R. Intramyometrial arteriovenous malformation: Sonographic diagnosis and treatment with embolization. J. Women’s Imaging (2003).
- Chan C C, Chu F, Pun T. Treating a recurrent uterine arteriovenous malformation with uterine artery embolization. A case report. J. Reprod. Med 48 (2003): 905-907.
- Chen A C Y, Sheu M H, Hung J H, et al. Three-dimensional magnetic resonance angiography guidance for conservative surgical management of pelvic arteriorvenous malformation. Acta Obstet. Gynecol. Scand (2003).
- Winsor S, Francis J A, Tran C, et al. Uterine arteriovenous malformation in pregnancy-a case series. Ultrasound Obstet. Gynecol (2004).
- Batch T, De Graef M, Kassem Z, et al. Acquired uterine arteriovenous fistula: Report of one case. J. Radiol (2004).
- Irikoma M, Yamamoto K. Uterine Arteriovenous Malformation Diagnosed Using Color Doppler Ultrasonography and MR Angiography. Japanese J. Med. Ultrason (2004).
- Poli-Neto O B, Víbrio Neto J B, Nogueira A A, et al. Embolização arterial seletiva em fístula arteriovenosa uterina pós-traumática. Radiol. Bras (2004).
- Aziz N, Lenzi T A, Jeffrey R B J, et al. Postpartum uterine arteriovenous fistula. Obstet. Gynecol 103 (2004): 1076-1078.
- Amagada J O, Karanjgaokar V, Wood A, et al. Successful pregnancy following two uterine artery embolisation procedures for arteriovenous malformation. J. Obstet. Gynaecol 24 (2004): 86-87.
- Nikolopoulos G, Murray A. Successful pregnancy outcome after surgical removal of arteriovenous malformation of the uterus. J. Obstet. Gynaecol 24 (2004): 315-316.
- Ahn H Y, Park I Y, Lee G, et al. Uterine arteriovenous malformation. Arch. Gynecol. Obstet 271 (2005): 172-175.
- Tullio Ghi, Susanna Giunchi, Cristina Rossi, et al. Three-dimensional power Doppler sonography in the diagnosis of arteriovenous malformation of the uterus. J. Ultrasound Med (2005).
- McCormick C C, Kim H S. Successful pregnancy with a full-term vaginal delivery one year after n-butyl cyanoacrylate embolization of a uterine arteriovenous malformation. Cardiovasc. Intervent. Radiol 29 (2006): 699-701.
- Yahi-Mountasser H, Collinet P, Nayama M, et al. Intra-uterine arteriovenous malformations. J. Gynecol. Obstet. Biol. la Reprod (2006).
- Morikawa M, Yamada T, Yamada H, et al. Effect of gonadotropin-releasing hormone agonist on a uterine arteriovenous malformation. Obstet. Gynecol (2006).
- Phoon C F, Lee S L, Kanagalingam D, et al. Subsequent pregnancy outcome after embolisation of uterine arteriovenous malformation. Ultrasound Obstet. Gynecol (2006).
- Delotte J, Chevallier P, Benoit B, et al. Pregnancy after embolization therapy for uterine arteriovenous malformation. Fertil. Steril (2006).
- Lin A-C, Hung Y-C, Huang L-C, et al. Successful treatment of uterine arteriovenous malformation with percutaneous embolization. Taiwan. J. Obstet. Gynecol 46 (2007): 60-63.
- Halperin R, Schneider D, Maymon R, et al. Arteriovenous malformation after uterine curettage: a report of 3 cases. J. Reprod. Med 52 (2007): 445-449.
- Rangarajan R D, Moloney J C, Anderson H J. Diagnosis and nonsurgical management of uterine arteriovenous malformation. Cardiovasc. Intervent. Radiol (2007).
- Bae S, Do YS, Shin SW, et al. Ethanol embolotherapy of pelvic arteriovenous malformations: An initial experience. Korean J. Radiol (2008).
- Rashmi Bagga, Preeti Verma, Neelam Aggarwal, et al. Failed angiographic embolization in uterine arteriovenous malformation: a case report and review of the literature. Medscape J. Med 10 (2008): 12.
- Dar P, Karmin I, Einstein M H. Arteriovenous malformations of the uterus: Long-term follow-up. Gynecol. Obstet. Invest (2008).
- Bamberg, C. OP07.04: Three-Dimensional Power Doppler Sonography in the diagnosis of Arteriovenous Malformations of the uterus and treated by selective uterine artery embolization. Ultrasound Obstet. Gynecol (2008).
- Singh S, Chowdhury V G C. Uterine AVM. Internet J. Radiol Volume 9 N (2007).
- Maldonado J, Perez C, Rodriguez W. AJR teaching file: Profuse vaginal bleeding seven weeks following induced abortion. Am. J. Roentgenol (2008).
- Griffin D W, Strand E A. Arteriovenous malformation of the uterus after a midtrimester loss: a case report. J. Reprod. Med 54 (2009): 333-336.
- Taylor E, Hitkari J. Hysteroscopic identification of a uterine arteriovenous malformation. J. Obstet. Gynaecol. Can 31 (2009): 1117-1118.
- Vilos A G, Vilos G A, De Vrijer B, et al. Fertility and pregnancy outcomes following uterine artery embolization (UAE) for uterine arteriovenous malformation (AVM). Gynecol. Surg (2010).
- Wijesekera N T, Padley S P, Kazmi F, et al. Embolization of uterine arteriovenous malformations associated with cyanotic congenital heart disease. Cardiovasc. Intervent. Radiol 32 (2009): 1075-1079.
- Guo N, Liu H, Peng Z. Uterine arteriovenous fistula necessitating hysterectomy after two unsuccessful embolizations in an 18-year-old patient. Ann. Vasc. Surg 24 (2010): 827.e9-827.e11.
- Kim T-H, Lee H-H. Presenting features of women with uterine arteriovenous malformations. Fertil. Steril 94 (2010): 2330.e7-2330.e10
- Wani N A, Shaheen F, Kousar T, et al. Uterine arteriovenous malformation diagnosed with multislice computed tomography: a case report. J. Reprod. Med 55 (2010): 166-170.
- Przybojewski S J, Sadler D J. Novel image-guided management of a uterine arteriovenous malformation. Cardiovasc. Intervent. Radiol.34 Suppl 2 (2011): S161- S166.
- Molvi S N, Dash K, Rastogi H, et al. Transcatheter embolization of uterine arteriovenous malformation: report of 2 cases and review of literature. J. Minim. Invasive Gynecol 18 (2011): 812-819.
- Vaknin Z, Sadeh-Mefpechkin D, Halperin R, et al. Pregnancy-related uterine arteriovenous malformations: experience from a single medical center. Ultraschall Med.32 Suppl 2 (2011): E92-E99.
- Scioscia M, Zantedeschi B, Trivella G, et al. A suggestive diagnosis of uterine arteriovenous fistula based on ultrasonography and hysteroscopy. European journal of obstetrics, gynecology, and reproductive biology 160 (2012): 116-117.
- Clarke J A, Viswanatha R K, Hamid R, et al. Diagnosis and management of life-threatening hypermenorrhagia caused by uterine arteriovenous malformation secondary to surgical termination of pregnancy: video evidence! BMJ Case Rep (2012).
- Levy-Zaubermann Y, Capmas P, Legendre G, et al. Laparoscopic management of uterine arteriovenous malformation via occlusion of internal iliac arteries. J. Minim. Invasive Gynecol 19 (2012): 785-788.
- Chittawar P B, Patel K, Agrawal P, et al. Hysteroscopic diagnosis and successful management of an acquired uterine arteriovenous malformation by percutaneous embolotherapy. Journal of mid-life health 4 (2013): 57-59.
- Goyal S, Goyal A, Mahajan S, et al. Acquired uterine arteriovenous malformation developing in retained products of conception: a diagnostic dilemma. J. Obstet. Gynaecol. Res 40 (2014): 271-274.
- Woodhams R, Ogasawara G, Ishida K, et al. Successful treatment of acquired uterine arterial venous malformation using N-butyl-2-cyanoacrylate under balloon occlusion. Acta radiologica short reports3 2047981614545910 (2014).
- Aslan H, Acar DK, Ekiz A, et al. Sonographic features and management options of uterine arteriovenous malformation. A case report. Med. Ultrason 17 (2015): 561-563.
- Vilos AG, Vilos GA, Hollett-Caines J, et al. Uterine artery embolization for uterine arteriovenous malformation in five women desiring fertility: pregnancy outcomes. Hum. Reprod 30 (2015): 1599-1605.
- Tullius TG Jr, Ross JR, Flores M, et al. Use of three-dimensional power Doppler sonography in the diagnosis of uterine arteriovenous malformation and follow-up after uterine artery embolization: Case report and brief review of literature. J. Clin. Ultrasound 43 (2015): 327-334.
- Stefano Calzolari, Mauro Cozzolino, Eleonora Castellacci, et al. Hysteroscopic management of uterine arteriovenous malformation. J. Soc. Laparoendosc. Surg (2017).
- Bandura P, Rawnaq T, Holzknecht A, et al. Management of Intrauterine Arteriovenous Malformation (AVM) in 14 Patients by Sonographically Guided Tisseel Application. Ultraschall Med 39 (2018): 48-55.
- Lehrman ED, Heller M, Poder L, et al. Transvaginal Obliteration of a Complex Uterine Arteriovenous Fistula Using Ethylene Vinyl Alcohol Copolymer. J. Vasc. Interv. Radiol 28 (2017): 842-843.
- Evans A, Gazaille RE, McKenzie R, et al. Acquired uterine arteriovenous fistula following dilatation and curettage: an uncommon cause of vaginal bleeding. Radiology case reports 12 (2017): 287-291.
- Ho C Y, Seow K M, Huang L W, et al. Fertility outcomes following pelvic embolization in women with acquired uterine arteriovenous malformation. Taiwan. J. Obstet. Gynecol (2017).
- Wee A, Saxena R, Bagchi T. Secondary post-partum haemorrhage from a true uterine arteriovenous malformation. J. Obstet. Gynaecol 38 (2018): 1169-1170.
- El Agwany A S, Elshafei M. Extensive uterine arteriovenous malformation with hemodynamic instability: Embolization for whole myometrium affection. European journal of obstetrics, gynecology, and reproductive biology 222 (2018): 188-191.
- Bettaiah R, Kamath S S. Laparoscopic Uterine Artery Ligation for Uterine Arteriovenous Malformation. J. Minim. Invasive Gynecol 25 (2018): 1124-1125.
- Schwartz E, Faller E, Akladios CY, et al. Total Laparoscopic Hysterectomy for Endometriosis and an Arteriovenous Malformation. J. Minim. Invasive Gynecol 26 (2019): 363-364.
- Dimassi K, Ben Amor A, Halouani A, et al. Successful management of acquired uterine arteriovenous malformation. Tunis. Med 96 (2018): 445-447.
- Guida M, Maffucci D, Iannuzzi G, et al. Successful pregnancy after uterine artery embolization for uterine arterovenous malformation: a rare case report. International journal of women’s health 10 (2018): 745-750.
- Shim D J, Choi S J, Jung J M, et al. Uterine arteriovenous malformation with repeated vaginal bleeding after dilatation and curettage. Obstetrics & gynecology science 62 (2019): 142-145.
- Tae Hee Kim, Nam Kyeong Kim, Seul Ki Kim, et al. Uterine Arteriovenous Malformation Treated by Hysteroscopic Excision. Gynecology and minimally invasive therapy 8 (2019): 132-134.
- Khan S, Saud S, Khan I, et al. Acquired Uterine Arteriovenous Malformation Following Dilatation and Curettage Treated with Bilateral Uterine Artery Embolization: A Case Report. Cureus 11 (2019): e4250.
