Systematic Review on Adherence, Barriers to Treatment and Impact of Airway Clearance in Bronchiectasis
Article Information
Alyssa Yue Hui Low1#, Just Sen Tan1#, Rethinam Ganesan2, Jaclyn Tan2, Albert Yick Hou Lim1,3,4*
1Yong Loo Lin School of Medicine, National University of Singapore, Singapore
2Department of Physiotherapy, Tan Tock Seng Hospital, Singapore
3Department of Respiratory and Critical Care Medicine, Tan Tock Seng Hospital, Singapore
4Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
*Corresponding author: Albert YH Lim, Department of Respiratory and Critical Care Medicine, Tan Tock Seng Hospital, 11 Jalan Tan Tock Seng 308433, Singapore
#Authors contributed equally to this study
Received: 26 September 2020; Accepted: 03 October 2020; Published: 12 October 2020
Citation: Alyssa Yue Hui Low, Just Sen Tan, Rethinam Ganesan, Jaclyn Tan, Albert Yick Hou Lim. Systematic Review on Adherence, Barriers to Treatment and Impact of Airway Clearance in Bronchiectasis. Archives of Clinical and Biomedical Research 4 (2020): 481-497.
Share at FacebookAbstract
Background and objective: Chest physiotherapy (CPT) is an integral standard of treatment for patients with bronchiectasis. This study aims to analyse patients’ adherence to CPT, barriers to adherence and the impact on respiratory outcomes.
Methods: A systematic literature review was conducted through electronic searches of Pubmed, Embase and Cochrane databases from 1st January 2010 to 20th March 2020 for adherence and or non-adherence rates to CPT of patients with cystic fibrosis (CF) and non-CF bronchiectasis (NCFB).
Results: A total of thirteen publications with a study duration ranging from 1 to 16 months were qualified for inclusion. The paediatric population had a higher mean adherence rate than the adult population (range: 51% to 61% vs. 41% to 51%). The commonest CPT modalities were positive expiratory pressure (PEP) and flutter devices. Patients with high adherence of CPT had a significantly lower rate of hospitalisation than patients with low adherence rate (0.5 episodes/year vs. 1.4 episodes/year). A low adherence to CPT was associated with more pulmonary exacerbations. Patients with higher burden of treatment, perceived necessity of CPT and higher socio-economic status were more adherent to CPT. However, the effect of adherence to CPT on lung function and the quality of life (QoL) was inconclusive.
Conclusions: The current literature suggests that adherence rate to CPT is poor amongst patients with NCFB and CF. There is a greater need for better understanding of the clinical consequences and economic impact of CPT on patients with NCFB.
Keywords
Bronchiectasis; Cystic Fibrosis; Chest physiotherapy; Adherence; Barriers; Outcomes
Article Details
Abbreviations:
CPT- chest physiotherapy; CF- cystic fibrosis; NCFB- non-cystic fibrosis bronchiectasis; PEP- positive expiratory pressure; UK- United Kingdom; USA- United States of America; ABPA- allergic bronchopulmonary aspergillosis; GERD- gastro-esophageal reflux disease; CFRD- cystic fibrosis related diabetes mellitus; COPD- chronic obstructive pulmonary disease; HRQoL- Health-related quality of life; LCQ- Leicester Cough Questionnaire; SGRQ- St George's Respiratory Questionnaire; FEV1- forced expiratory volume in 1 second; FVC- forced vital capacity; PRISMA- Preferred Reporting Items for Systematic Reviews and Meta-Analyses; MeSH- Medical Subject Headings; BMI- mean body mass index; QoL- quality of life; HFCWO- High frequency chest wall oscillation; BMQ- Beliefs about Medicine Questionnaire; ACT- Airway clearance technique; HFCWO- High-frequency chest wall oscillating device; FD- flutter device; PEP- Positive expiratory pressure devices; ACBT- active cycle breathing technique; AD- autogenic drainage; P+PD- Percussion and postural drainage; MARS- Medication Adherence Report Scale; HBM- Health Belief Model; QoL-B- Quality of Life Questionnaire-Bronchiectasis; DPD- Daily Phone Diary
1. Introduction
Non-cystic fibrosis bronchiectasis (NCFB) is a chronic respiratory disease with abnormal permanent dilatation of bronchi [1]. It is characterised by a variety of symptoms, including, cough, excess sputum production, dyspnoea, weight loss, haemoptysis, airway inflammation and recurrent chest infections [2]. The disease can be caused by many aetiologies which are often unidentifiable and idiopathic [3, 4]. In adults, previous pulmonary infections constitute a significant proportion of the aetiologies of NCFB [3, 5]. The other less common aetiologies include immune-related causes, allergic bronchopulmonary aspergillosis (ABPA), connective tissue disease, gastro-esophageal reflux disease (GERD) and sinobronchial syndrome [3]. The major cause of bronchiectasis in the younger population is cystic fibrosis (CF). CF is a genetic disease that results in chronic progressive obstructive lung disease and manifests itself systemically through nutrient malabsorption, liver cirrhosis and CF-related diabetes mellitus (CFRD). CF is not curable and therefore, the focus of the treatment is on the optimisation and maintenance of lung function, as well as the reduction of exacerbations and morbidities [6].
The prognosis of patients with NCFB is poor with mortality rates of 10.6% over a 3.5-year period, 20.4% over a 5-year period and 29.7% over a 13-year period [7-10]. The main cause of deaths was respiratory failure secondary to respiratory infections [9, 10]. Although the global prevalence of NCFB is largely unknown, the trend of prevalence of NCFB is increasing worldwide [3, 11, 12]. The management of it is challenging with limited treatment options. The treatment of NCFB focuses on airway clearance, treatment of chest infections and prevention of exacerbations such as influenza vaccination [13]. Chest physiotherapy (CPT) facilitates airway clearance of secretions and is widely promoted as the key component in the management of bronchiectasis [13]. Antibiotics are used to treat acute exacerbations, eradicate infections, reduce bacterial load and suppress infections [1, 14]. Bronchodilators are used for patients with concomitant respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD).
The British Thoracic Society (BTS) guidelines for NCFB in adults recommend twice daily CPT for patients with persistent productive cough [15]. There are many different types of CPT techniques, such as postural drainage, chest wall percussions, vibrations, as well as, using positive expiratory pressure devices (e.g. Acapella, Flutter) [16, 17]. The adherence rate to CPT ranges from 14% to 60%, and is influenced by the treatment modality [18, 19]. The outcomes of NCFB treatment on health-related quality of life (HRQoL) can be evaluated by the Leicester Cough Questionnaire (LCQ) and St George's Respiratory Questionnaire (SGRQ), with both including symptoms of exacerbation [20, 21]. Other methods of evaluating the effectiveness of treatment include measuring forced expiratory volume (FEV1) in 1 second (i.e. FEV1% predicted), forced vital capacity (FVC) and exercise tolerance.
In the study of CPT, although there is a lack of studies with good methodological quality in demonstrating its efficacy and effectiveness, regular CPT has been broadly advocated in international guidelines as a pillar of the management of bronchiectasis. Poor adherence to treatment is well recognized, and significantly contributes to treatment failures in medical interventions. Therefore, it is imperative to examine factors influencing adherence to CPT in patients with bronchiectasis. Additionally, as there are very few evidence based treatment for bronchiectasis, it is also important to determine if CPT plays a role on the disease progression, lung function, exacerbations and quality of life of patients with bronchiectasis [22]. We undertook a literature review to determine whether compliance with CPT influences the clinical outcomes of patients and if it is associated with the duration of CPT treatment.
2. Materials and Methods
A systematic literature review was conducted with the aim of identifying publications that reported the adherence rates to CPT in patients with either CF or NCFB. This was done in accordance with the Cochrane Handbook of Systematic Reviews and Meta-analysis and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines [23].
2.1 Search criteria
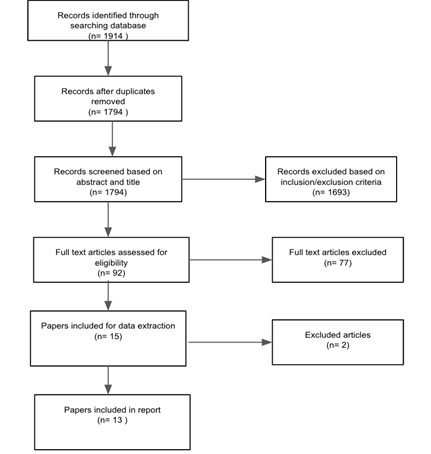
The present study was based on a search of the Pubmed, Embase and Cochrane databases using a combination of Medical Subject Headings (MeSH) and non-MeSH key terms with Boolean operator as shown in Table 1. The following search strategy was used: (“Bronchiectasis” OR “Cystic Fibrosis” OR “Cystic fibrosis bronchiectasis”) AND (“Chest Physiotherapy” OR “Chest Physical Therapy” OR “Airway Clearance” OR “Respiratory Therapy”) AND (“Compliance” Or “Adherence” OR “Persistence” OR “Daily treatment”). All searches underwent double-blind screening by three researchers (J.S.Tan, A.Y.H. Low, A.Y.H. Lim) and full-text articles of potentially appropriate abstracts were reviewed. Duplicates were removed and conflicts were resolved by consensus. Search strategy was supplemented by review of reference lists, bibliographies including the BTS guidelines and investigator files. A PRISMA flow diagram of the review and selection of articles is shown in Figure 1.
|
#1 |
Bronchiectasis [All Fields] OR Cystic Fibrosis [All Fields] OR Cystic Fibrosis Bronchiectasis [All Fields] |
|
#2 |
Bronchiectasis [MeSH Terms] OR Cystic Fibrosis [MeSH Terms] |
|
#3 |
#1 OR #2 |
|
#4 |
Chest Physiotherapy [All Fields] OR Chest Physical Therapy [All Fields] OR Airway Clearance [All Fields] OR Respiratory Therapy [All Fields] |
|
#5 |
Respiratory Therapy [MeSH Terms] |
|
#6 |
#4 OR #5 |
|
#7 |
Compliance [All Fields] OR Adherence [All Fields] OR Persistence [All Fields] OR Daily Treatment [All Fields] |
|
#8 |
Patient Compliance [MeSH Terms] |
|
#9 |
#7 OR #8 |
|
#10 |
#3 AND #6 AND #9 |
|
#11 |
Publication Date: 2010/01/01 to 2020/03/20 |
Table 1: Search strategy.
2.2 Study Inclusion and Exclusion Criteria
All studies were considered eligible if they fulfilled the following criteria: original publications, inclusion of a cohort of patients with CF or NCFB, adherence rates to CPT reported. Abstracts, letters to editors, case study reports, review papers and non-English language papers were excluded.
2.3 Data Extraction
Data was extracted from selected papers using a standardised method into a preformatted database by a single researcher. All extracted data was then verified by a second researcher. Any disagreement between investigators was resolved independently by a third investigator. Data extracted for study design and patient demographics included author name, year of publication, study design, treatment modalities, study population, mean age, gender and mean percent predicted FEV1 (Table 2). Data extracted regarding adherence includes the methods used to measure adherence, adherence criteria, adherence rates and other findings/outcomes associated with adherence (Table 3).
3. Results
A total of 1794 articles were identified. Of these, 92 articles were screened in full paper review after excluding articles during title and abstract review. During the full paper review, 79 articles were excluded and 13 articles fulfilled the criteria for the systemic review (Figure 1) [19, 24-36]. The characteristics of the thirteen included studies are shown in Table 2. There were eight cross-sectional studies, three prospective studies, one interview-based study, one was a combination of a randomized clinical trial and a retrospective study (Table 2). All the studies were on CF patients apart from one study on NCFB patients. There were a total of 990 patients involved in the 13 studies with sample sizes ranged from 36 to 153 participants. Eight studies were conducted in the United States of America (USA) [26, 27, 31-36] two in Northern Ireland [24, 30], two in Brazil [19, 29], and one in Canada [28]. The mean age of paediatric and adult study populations ranged from 11.2 to 12.2 years and 28.2 to 64 years respectively (Table 2). The study duration ranged from 1 to 16 months. Five (38.5%) studies reported the type of chest physiotherapy modalities [24-27, 29, 30, 32, 33, 35]. High frequency chest wall oscillation (HFCWO) therapy was assessed in two studies [31, 36] and a variety of airway clearance devices were assessed in three studies [19, 28, 34]. The adherence rates were measured by either using a self-reported questionnaire, daily phone diary or a built-in chronometer.
In terms of study outcomes, five studies reported on the association between adherence and lung function [24, 29, 31, 34, 36]. One study reported hospitalization rates and duration of stay in hospital [29]. Two studies reported on the association between adherence and quality of life [24, 29]. Four studies reported on the barriers to adherence [19, 29, 32, 33]. Ten studies reported on patient’s perceptions and/or its association with adherence [26-30, 32-36]. Three studies compared adherence rates amongst various types of CPT [19, 28, 34].
(#) Seventy seven articles were excluded as they do not report adherence rate on CPT, literature review papers, abstracts and non-English language papers; (*) Two articles were excluded as limited data on adherence to CPT provided and duplicated cohort
|
References |
Study design |
Treatment modalities (Duration) |
Study population (n) |
Mean age (SD) (years) |
Male (n (%)) |
Mean predicted FEV1% (SD) |
|
McCullough AR [24,25] |
Prospective |
ACT (not specified) |
Adult patients with NCFB (n=75) |
64 (8) |
24 (32) |
61 (25) |
|
Feiten TDS [29] |
Cross-sectional |
ACT (not specified) |
Paediatric patients with CF (n=66) |
12.2 (3.2) |
31 (47) |
90 (24) |
|
Goodfellow N [30] |
Cross-sectional |
ACT (not specified) |
Paediatric patients with CF (n=100) |
median (range):10.1 (0.2-18.6) |
44 (44) |
84 (4.5) |
|
Mikesell CL [31] |
Prospective |
HFCWO |
Paediatric and adult patients with CF (n=85) |
15.6 (4.7) |
43 (51) |
97.5 (20) |
|
Sawicki GS [32] |
Cross-sectional |
CPT (not specified) |
Paediatric and adult patients with CF (n=18) |
median (range):18 (16-21) |
8 (44) |
91(range: 38-127) |
|
Zanni RL [33] |
Cross-sectional |
ACT (not specified) |
Paediatric and adult patients with CF (n=83) |
NR |
NR |
NR |
|
Flores JS [19] |
Cross-sectional |
PEP, FD, ACBT, AD, P+PD |
Paediatric and adult patients with CF (n=63) |
23.1 (6.3) |
31 (49) |
NR |
|
Modi AC [34] |
Retrospective |
HFCWO, FD, P+PD (16 months) |
Paediatric and adult patients with CF (n=153) |
14.3 (7.9) |
84 (55) |
86.7 (19.1) |
|
Sherman AC [35] |
Prospective |
ACT (not-specified) |
Adult patients with CF (n=66) |
27.15 (9.1) |
30 (45.4) |
65.5 (24.8) |
|
Dempster NR [26] |
Cross-sectional |
ACT (not specified) |
Paediatric patients with CF (n=33) |
13.33 (2.4) |
15 (44.5) |
NR |
|
Grossoehme DH [27] |
Cross-sectional |
ACT (not specified) |
Paediatric patients with CF (n=45) |
13.8 (2.2) |
18 (40) |
85.7 (20.8) |
|
Pakhale S [28] |
Cross-sectional |
Acapella, HFCWO, P+PD, PEP |
Adult patients with CF (n=42) |
30.6 (10.7) |
25 (59.5) |
54.9 (20.7) |
|
Oates GR [36] |
Prospective |
HFCWO |
Paediatric patients diagnosed with CF (n=110) |
11.2 (4.7) |
NR |
NR |
Table 2: Study design and demographics of study population.
3.1 The rate of adherence on CPT
The rate of adherence of CPT in the paediatric study population was higher than the adult study population (mean range: 51% to 61% vs. 41% to 51% respectively) [24, 28, 29, 30, 35, 36]. The CPT modalities associated with the highest rate of adherence was flutter device (83.3%), followed by positive expiratory pressure (PEP) (68.8%), active cycle of breathing (34%), autogenic drainage (28.6%), percussion and autogenic drainage (14.3%) [19]. Adolescents with CF were more likely to achieve moderate adherence with flutter devices compared with percussion and postural drainage and HFCWO therapy [28, 34]. The method of assessment of adherence varied widely across studies. Some studies stratified patients into high, moderate and low adherence groups [19, 34, 36]. Whilst other studies stratified patients into adherent or non-adherent groups [24, 28, 30, 32, 33, 35]. This causes comparison of adherence rates across studies to be more challenging.
3.2 The effect of adherence of CPT on lung function and pulmonary exacerbations
The effect of adherence to CPT on lung function varied amongst studies (Table 3). Three studies reported no significant association between adherence and lung function [24, 29, 36]. However, 2 other studies reported a positive association between percent predicted FEV1 and the rate of adherence to CPT [31, 34]. It was found that patients with better lung function felt a lesser need to be compliant to CPT [19]. Feiten and co-workers reported that low adherence to CPT was associated with patients who had advanced lung disease and frequent hospitalizations [29]. Pulmonary exacerbation rate was assessed in two studies [24, 31]. One study reported fewer pulmonary exacerbations among patients with higher adherence to CPT [31]. Meanwhile, the other study reported no association between pulmonary exacerbations and adherence to CPT [24].
3.3 The effect of adherence of CPT on the quality of life
Two studies reported on the association between quality of life (QoL) and adherence to CPT [24, 29]. McCullough and co-workers reported that adherence to CPT was associated with a higher burden of treatment and a poorer QoL [24]. The same study reported that patients with more symptoms were more likely to adhere to CPT. Conversely, Feiten and co-workers reported that patients with moderate or poor adherence to CPT were associated with a lower score of QoL on the domains of emotion, physical, treatment burden, health perceptions, social and respiratory functioning [29].
3.4 Patients’ perceptions and socio-economic status
Ten studies reported on the association between patients’ perceptions of CPT, adherence to CPT, and or barriers to adherence [26-30, 32-36]. Factors affecting perception of CPT were the perceived importance of CPT, patients’ understanding of the treatment, difficulty of use and self-efficacy. Children whose parents had strong beliefs regarding their child’s use of CPT were significantly associated with a high rate of adherence of CPT [33]. Five studies reported that positive perception of CPT were associated with higher adherence to CPT [26, 27, 30, 32, 35]. Two studies reported that greater self-efficacy was an independent predictor of adherence [27, 35]. A high annual household income (more than $50,000), maternal college education, and more adults in the household were associated with higher adherence rate to CPT [34, 36].
3.5 Barriers to adherence of CPT
The lack of time was the commonest reason for not performing CPT [19, 32, 33]. The other reasons were competing priorities, heightened awareness of disease trajectory, privacy concerns, and lack of perceived consequences from non-adherence [32].
|
References |
Methods of assessment |
Definition of adherence |
Rate of adherence |
Outcomes associated with adherence |
|
McCullough AR [24,25] |
1) Self-reported Medication taking Scale (MARS) questionnaire and an additional question. |
1) Scoring ≥4 (≥80%) on this scale at all data collection points. |
41% (n = 30) |
1) No association with pulmonary exacerbation. 2) No association with predicted FEV1 (%). 3) High adherence to CPT associated with lower QoL-B score. 4) High adherence to CPT associated with higher burden of treatment. |
|
Feiten TDS [29] |
1) Questionnaire developed from a previous study: consisting objective questions |
1) High adherence: always or rarely failed to perform the ACT recommended. 2) Moderate adherence: often failed to perform the ACT recommended. 3) Poor adherence: never or almost never performed the ACT recommended. |
1) High adherence: 59% (n=39) 2) Moderate/ poor adherence: 41% (n=27) |
1) No association with lung function. 2) Moderate or poor adherence to CPT associated with higher number of hospitalisations. 3) Moderate or poor adherence to CPT associated with poor QoL. 4) Moderate or poor adherence to CPT associated with more severe disease (Lower S-K clinical score). 5) Moderate or poor adherence to CPT associated with "Feeling tired" and "not liking the recommended technique". |
|
Goodfellow N [30] |
1) MARS questionnaire 2) A composite adherence measurement |
1) The MARS questionnaire: Higher scores indicated higher levels of self-reported adherence. 2) A composite adherence measurement: low-adherer if they scored less than 80% in any one of the methods described. |
1) Child self-reported: High adherence: 61% (n=61). 2) Composite adherence measurement: High adherence: 52 (52%) |
1) High adherence to CPT associated with younger age. 2) High adherence to CPT associated with strong parental necessity beliefs. 3) No association with parental depressive symptoms. |
|
Mikesell CL [31] |
1) Vest System model 105 equipped with a novel data recorder for recording: Duration and the number of sessions of HFCWO therapy used were recorded. |
Adherence was measured as the measured average daily therapy time as a percentage of the prescribed daily therapy time. |
69% (n= 59) |
1) High adherence to CPT associated with better pulmonary function. 2) High adherence to CPT associated with fewer pulmonary exacerbations. 3) High adherence to CPT associated with younger child. 4) High adherence to CPT associated with shorter therapy time. 5) High adherence to CPT associated with assistance with treatment. |
|
Sawicki GS [32] |
1) Interview: self-reported levels of adherence to treatment. |
Participants are considered non-adherent if they report that they are often or always non-compliant to their CPT. |
Patients self-reported: 72.2% (n=13) |
1) Parents and adolescents reported that adherence to nebulizer treatments and chest physical therapy was the most difficult. 2) Reported barriers to adherence included time pressures, competing priorities, heightened awareness of disease trajectory, privacy concerns, and lack of perceived consequences from non-adherence. 3) Facilitators identified for adherence included recognizing the importance of therapies, developing strong relationships with care teams, establishing structured routines, and focusing on shifting responsibilities from a parent to their adolescent child. |
|
Zanni RL [33] |
1) In-clinic ACT questionnaire. 2) Patient demonstration of ACT. |
Adherent defined as consistently performed ACT as prescribed by the healthcare provider. |
1) Adherent with correct technique: 37% (n= 31). 2) Adherent with incorrect technique:10% (n=8). 3) Non-adherent: 53% (n=44) |
1) Effective ACT was reported by 90% of patients who adhered and 80% of who did not adhere to ACT. 2) Patients adhered to ACT had less barriers to CPT than non- adherent to ACT (56% vs. 75%). 3) Common barriers to ACT were finding the time to perform treatments (49%), equipment fatigue (37%). |
|
Flores JS [19] |
1) Questionnaire adapted from other studies. |
1) High adherence: every day or almost every day. 2) Moderate adherence: 3–5 days a week. 3) Poor adherence: <3 days a week. |
1) High adherence: 60% (n = 38). 2) Moderate adherence: 19% (n = 12). 3) Poor adherence: 21% (n = 13). |
1) Lower than high school education level was an independent factor for poor adherence. 2) High adherence to PEP and FD device techniques. 3) Reasons for poor adherence to ACT were “not enough time to do ACT” (28%), “cannot be bothered” (16%), and “do not enjoy ACT technique” (8%). Many (32%) provided no reason. |
|
Modi AC [34] |
1) Daily phone diary (DPD): uses a cued recall procedure to track parents, adolescents, and adults through their activities over the past 24 hours to assess adherence. |
Patients who used their assigned ACT twice daily for 20min/session |
Level of adherence to ACT (percussion vs. FD vs. vest therapy) 1) Low adherence (n = 22): 14% vs. 15% vs.14%. 2) Medium adherence (n = 75): 40% vs. 67% vs. 42%. 3) High adherence (n = 56): 46% vs. 14% vs. 44% |
1) Group-based trajectory modelling revealed the best-fitting solution was a three-group model: low-adherence (14%), medium-adherence (49%), and high-adherence (37%) groups. 2) ACT type was the only significant predictor of adherence trajectories (FD was the most preferred modality of ACT. 3) Family income greater than $50,000 were 1.87 times more likely to be in the high-adherence trajectory group. 4) Patients with better FEV1% predicted were slightly more likely to be in the high adherence group. |
|
Sherman AC [35] |
1) Cystic Fibrosis Treatment Questionnaire (CFTQ) for self-reporting of adherence 2) MARS, includes 9 items to which subjects respond on a 5-point scale |
1) Persistent Adherence defined as always doing treatment or missing no more 2) Higher MARS score represented greater adherence. |
High persistent adherence: 45.5% (n = 30)
|
1) Social cognitive predictor variables (i.e., self-confidence in overcoming barriers), outcome expectations (i.e., perceived necessity of ACT and concerns about its disruptive effects), and subjective norms (i.e., perceptions of being influenced by others) assessed at baseline were significantly related to persistent adherence, except subjective norms. 2) Fewer baseline concerns about ACT and greater self-efficacy were independent predictors for persistence adherence. |
|
Dempster NR [26] |
1) Self-Care Inventory-Cystic Fibrosis (SCI-CF) assesses adherence to the various aspects of treatment. 2) Health Belief Model (HBM) Scale- questionnaire consists of 72 items composed of five subscales measuring children’s and parents’ health beliefs about adherence: (a) susceptibility, (b) severity, (c) benefits, (d) barriers, and (e) cues to action. |
A 5-point Likert-type scale (1 = never do it as recommended and 5 = always do it as recommended without fail) |
Child’s self-reported (SD: 0.78, Range: 2-5) Mean: 4.03 (SD: 0.85, Range:2-5) |
1) For parents, the HBM variables (susceptibility, Severity, Benefits, Barriers, Cues to action) were significantly related to children’s adherence to CPT, oral antibiotics, and vitamins. 2) A positive correlation was found between children and parent reports of overall adherence |
|
Grossoehme DH [27] |
1) 2 Daily Phone Diary (DPD) calls were scheduled with participants during the 3 weeks following recruitment at the clinic |
Perfect adherence = 100% (ratio of DPD reported treatment frequency divided by prescribed treatment frequency) |
Perfect adherence: 20% (n= 9) |
1) Greater perceived utility of treatment, treatment-supportive norms from close friends (but not family), and greater self-efficacy predicted greater intentions to perform ACT. 2) Treatment intentions predicted airway clearance adherence. |
|
Pakhale S [28] |
1) CF Treatment Regimen and Adherence Form |
Categorized participants as adherent or non-adherent according to whether they performed the treatment at the frequency recommended by the health care professional (HCP). |
Adherent to HCP recommendation - P+PD: 6 (19.4%) - PEP: 4 (50%) - HFCWO: 1 (20%) - Acapella: 0 (0%) |
1) Participants’ adherence was greater when calculated in relation to participants’ understanding of treatment recommendations than when calculated in relation to actual HCP treatment recommendations. |
|
Oates GR [36] |
1) Objective adherence data from HFCWO device: 2 readings were recorded within 2 days of study enrolment, and the second approximately 5 weeks after baseline. The difference between the 2 readings, divided by the number of days between them, provided an average daily use of the HFCWC vest. |
Adherence defined as a ratio of mean-to-prescribed daily use (%). 3 categories: |
Low adherence: 28% (n=31) Moderate adherence: 37% (n = 41) High adherence: 35% (n = 38) |
1) Self-reports overestimated actual objective adherence to airway clearance therapy 2) Overestimation of the subject's adherence increased with lower income 3) Maternal college education, annual income >$50,000, and more adults in the household were independently related to better adherence. 4) Current adherence to ACT with HFCWO was not associated with lung function over 12 months. |
Table 3: Methods, definition, rate and outcomes of adherence to CPT.
4. Discussion
The management of NCFB is challenging with a major focus on pharmacological interventions. Pharmacological interventions are often expensive, have undesirable side effects, and are potentially time consuming such as nebulisation therapies. However, non-pharmacological interventions such as CPT, provides independent application, allows patients to have full control over the therapy, has no side effects and is often easy to use. However, to yield desirable effects, CPT needs to be performed on a long-term basis with patient’s adherence to treatment, motivation and the understanding of the benefits.
From our systemic review, we observed that higher adherence rate to CPT were associated with the paediatric population, higher treatment burden, the use of a flutter device, perception of the importance of CPT, higher annual household income, and the maternal education level of the affected child. There are two potential explanations for the higher rate of adherence to CPT in the paediatric population. Firstly, parents who strongly believe in the efficacy of CPT are more likely to ensure their children adhere to CPT [30]. Secondly, the adherence to CPT is also dependent on the assistance and support from the parents and carers. This is especially true for children of younger age as they can neither comprehend the benefits of CPT nor can they perform CPT independently.
Patients with more severe underlying respiratory diseases have a higher burden of treatment. They tend to have more symptoms and hence, lower QoL than patients with lower burden of treatment. Patients with more severe lung disease are more likely to adhere to their treatment regime [24, 25]. It is noteworthy that the overall QoL will improve with regular treatment of airway clearance. Two studies reported the adherence of CPT on CPT modalities [19, 34]. Flutter device was found to have a higher rate of adherence than other CPT modalities such as HFCWO, percussion and postural drainage, or PEP devices. The flutter device is easily mastered, portable and enables self- treatment thereby increasing adherence [34].
Mikesell and co-workers reported fewer pulmonary exacerbations among patients who had greater rate of adherence of CPT [31]. However, it is contrary to another report which did not find any significant difference in pulmonary exacerbation between the adherent and non-adherent group [24]. This may be explained by the differences in disease severity, the differences in duration of CPT, and the treatment modality used in these two studies. These two studies were unable to discern the direction of the relationship between adherence and pulmonary exacerbation.
The recognition of the necessity of CPT plays an important role in determining adherence. Goodfellow and co-workers used a multi-method approach assessment on adherence of treatment in children with CF [30]. They found out that children whose parents strongly believe in the treatment and children of younger age were significant independent predictors of the child’s adherence to CPT [30]. It is therefore important for the physicians to iterate the importance of CPT to the patients and carers, and to cultivate a strong belief in the treatment.
The time pressure is the commonest barrier for adherence to CPT [19]. To encourage adherence, treatment regime tailored to the needs and characteristics of the patients should be simple and not time-consuming. Additionally, CPT modalities that involve the use of devices (e.g. Acapella) should be considered as it improves mobilisation of mucus from airways, resulting in a shorter therapy session.
An important shortcoming of this review is small sample size with short duration of the studies which may not be enough to determine the effectiveness of the CPT on clinical outcomes. Follow up studies with bigger study populations over longer periods may overcome this limitation, and likely provide additional and important information on factors that may predict adherence of the CPT and its efficacy on treatment of bronchiectasis. The development of an ideal novel CPT device should focus on easy accessibility, usability, self-treatment and enabling treatment response monitoring.
5. Conclusion
In summary, our systemic review demonstrated that adherence to CPT is associated with reduction in pulmonary exacerbations and hospitalisations. A higher annual household income, perception on the importance of CPT, and higher education level of carers are predictors of adherence of CPT. The time pressure is the main barrier to the adherence of CPT. In addition, the lack of knowledge on of CPT on NCFB is significant especially with an anticipated worldwide increase of the prevalence NCFB. There is a greater need for better understanding of the clinical consequences and economic impact of CPT on patients with NCFB.
Acknowledgements
We thank Ms. Sandra Lawton and Dr. Priyanka Prasad for proof reading the manuscript.
Conflict of Interest
All the authors declare that they have no financial and no competing interests.
References
- McShane PJ, Naureckas ET, Tino G, et al. Non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med 188 (2013): 647-656.
- King PT, Holdsworth SR, Freezer NJ, et al. Characterisation of the onset and presenting clinical features of adult bronchiectasis. Respir Med 100 (2006): 2183-2189.
- Chandrasekaran R, Mac Aogáin M, Chalmers JD, et al. Geographic variation in the aetiology, epidemiology and microbiology of bronchiectasis. BMC Pulm Med 18 (2018): 1-14.
- Manasa J, Katzenstein D. Page 1 of 27 1. Heal (San Fr. 2015;(646):1-27.
- Patel IS, Vlahos I, Wilkinson TMA, et al. Bronchiectasis, exacerbation indices, and inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 170 (2004): 400-407.
- Paranjape SM, Mogayzel PJ. Cystic fibrosis. Pediatr Rev 35 (2014): 194-205.
- Gaillard EA, Carty H, Heaf D, et al. Reversible bronchial dilatation in children: Comparison of serial high-resolution computer tomography scans of the lungs. Eur J Radiol 47 (2003): 215-220.
- Goeminne PC, Scheers H, Decraene A, et al. Risk factors for morbidity and death in non-cystic fibrosis bronchiectasis: a retrospective cross-sectional analysis of CT diagnosed bronchiectatic patients. Respir Res 13 (2012): 21.
- Goeminne PC, Nawrot TS, Ruttens D, et al. Mortality in non-cystic fibrosis bronchiectasis: A prospective cohort analysis. Respir Med 108 (2014): 287-296.
- Loebinger MR, Wells AU, Hansell DM, et al. Mortality in bronchiectasis: A long-term study assessing the factors influencing survival. Eur Respir J 34 (2009): 843-849.
- Quint JK, Millett ERC, Joshi M, et al. Changes in the incidence, prevalence and mortality of bronchiectasis in the UK from 2004 to 2013: A population-based cohort study. Eur Respir J 47 (2016): 186-193.
- Seitz AE, Olivier KN, Adjemian J, et al. Trends in bronchiectasis among medicare beneficiaries in the United States, 2000 to 2007. Chest 142 (2012): 432-439.
- Polverino E, Goeminne PC, McDonnell MJ, et al. European Respiratory Society guidelines for the management of adult bronchiectasis. Eur Respir J 50 (2017).
- Hnin K, Nguyen C, Carson Chahhoud KV, et al. Prolonged antibiotics for non-cystic fibrosis bronchiectasis in children and adults. Cochrane Data base of Systematic Reviews 2015.
- Pasteur MC, Bilton D, Hill AT. British thoracic society guideline for non-CF bronchiectasis. Thorax 65 (2010).
- Lee AL, Burge AT, Holland AE. Airway clearance techniques for bronchiectasis (Review). Cochrane Database of Systematic Reviews 2015.
- Hill AT, Sullivan AL, Chalmers JD, et al. British thoracic society guideline for bronchiectasis in adults. Thorax 74 (2019).
- Narayanan S, Mainz JG, Gala S, et al. Adherence to therapies in cystic fibrosis: a targeted literature review. Expert Rev Respir Med 11 (2017): 129-145.
- Flores JS, Teixeira FÂ, Rovedder PME, et al. Adherence to airway clearance therapies by adult cystic fibrosis patients. Respir Care 58 (2013): 279-285.
- Murray MP, Turnbull K, MacQuarrie S, et al. Validation of the Leicester Cough Questionnaire in non-cystic fibrosis bronchiectasis. Eur Respir J 34 (2009): 125-131.
- Wilson CB, Jones PW, O’Leary CJ, et al. Validation of the St. George’s respiratory questionnaire in bronchiectasis. Am J Respir Crit Care Med 156 (1997): 536-541.
- Muñoz G, De Gracia J, Buxó M, et al. Long-term benefits of airway clearance in bronchiectasis: A randomised placebo-controlled trial. Eur Respir J 51 (2018).
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6 (2009).
- McCullough AR, Tunney MM, Quittner AL, et al. Treatment adherence and health outcomes in patients with bronchiectasis. BMC Pulm Med 14 (2014): 1-10.
- McCullough AR, Tunney MM, Elborn JS, et al. “All illness is personal to that individual”: A qualitative study of patients’ perspectives on treatment adherence in bronchiectasis. Heal Expect 18 (2015): 2477-2488.
- Dempster NR, Wildman BG, Masterson TL, et al. Understanding Treatment Adherence With the Health Belief Model in Children With Cystic Fibrosis. Heal Educ Behav 45 (2018): 435-443.
- Grossoehme DH, Szczesniak RD, Mrug S, et al. Adolescents’ Spirituality and Cystic Fibrosis Airway Clearance Treatment Adherence: Examining Mediators. J Pediatr Psychol 41 (2016): 1022-1032.
- Pakhale S, Baron J, Armstrong M, et al. Lost in translation? How adults living with Cystic Fibrosis understand treatment recommendations from their healthcare providers, and the impact on adherence to therapy. Patient Educ Couns 99 (2016): 1319-1324.
- Feiten T dos S, Flores JS, Farias BL, et al. Respiratory therapy: a problem among children and adolescents with cystic fibrosis. J Bras Pneumol 42 (2016): 29-34.
- Goodfellow NA, Hawwa AF, Reid AJM, et al. Adherence to treatment in children and adolescents with cystic fibrosis: A cross-sectional, multi-method study investigating the influence of beliefs about treatment and parental depressive symptoms. BMC Pulm Med 15 (2015): 1-10.
- Mikesell CL, Kempainen RR, Laguna TA, et al. Objective measurement of adherence to out-patient airway clearance therapy by high-frequency chest wall compression in cystic fibrosis. Respir Care 62 (2017): 920-927.
- Sawicki GS, Heller KS, Demars N, et al. Motivating adherence among adolescents with cystic fibrosis: Youth and parent perspectives. Pediatr Pulmonol 50 (2015): 127-136.
- Zanni RL, Sembrano EU, Du DT, et al. The impact of re-education of airway clearance techniques (REACT) on adherence and pulmonary function in patients with cystic fibrosis. BMJ Qual Saf 23 (2014).
- Modi AC, Cassedy AE, Quittner AL, et al. Trajectories of adherence to airway clearance therapy for patients with cystic fibrosis. J Pediatr Psychol 35 (2010): 1028?1037.
- Sherman AC, Simonton-Atchley S, Campbell D, et al. Persistent adherence to airway clearance therapy in adults with cystic fibrosis. Respir Care 64 (2019): 778-785.
- Oates GR, Stepanikova I, Rowe SM, et al. Objective versus self-reported adherence to airway clearance therapy in cystic fibrosis. Respir Care64 (2019): 176-181.