Spontaneous Bacterial Empyema - An Underdiagnosed Complication of Hepatic Hydrothorax
Article Information
Mohammed M. Uddin DO1, Neelambuj Regmi MD1, Muhammad Usama MD2, Anupamdeep Mehar MD1, Bachar Ahmad3, Tanveer Mir MD1*, Ayman Soubani MD4
1Department of Internal medicine, Detroit Medical Center, Wayne State University, Detroit, USA
2Department of Sleep Medicine. Cleveland Clinic. Cleveland, USA
3Wayne State University, Detroit, Michigan, USA
4Department of Pulmonary and Critical Care, Detroit Medical Center, Wayne State University. Detroit, USA
*Corresponding Author: Tanveer Mir MD, Department of Internal medicine, Detroit Medical Center, Wayne State University, Detroit, USA
Received: 07 December 2020; Accepted: 21 December 2020; Published: 08 January 2021
Citation: Mohammed M. Uddin, Neelambuj Regmi, Muhammad Usama, Anupamdeep Mehar, Bachar Ahmad, Tanveer Mir, Ayman Soubani. Spontaneous Bacterial Empyema - An Underdiagnosed Complication of Hepatic Hydrothorax. Archives of Clinical and Medical Case Reports 5 (2021): 64-69.
Share at FacebookAbstract
Spontaneous bacterial empyema (SBEM) is a life-threatening and underdiagnosed development of hepatic hydrothorax (HH), which is a significant complication of liver cirrhosis and portal hypertension. SBEM is the development of a spontaneous infectious process in a pre-existing pleural effusion without any evidence of pneumonia in patients with Hepatic Hydrothorax. Patients with SBEM has poor prognosis with significantly high rate of mortality and morbidity. We present the case of a 54-year-old female with history of decompensated liver cirrhosis secondary to alcohol use disorder, recurrent ascites, refractory bilateral pleural effusions who had developed SBEM associated with uncharacteristically high glycopleuria values. In this article, we will emphasize on recent data focusing on the diagnostic complications and treatment of cirrhotic patients with SBEM. Increased awareness of this uncommon condition will help clinicians recognize and address it early.
Keywords
SBEM; Hepatic hydrothorax; Cirrhosis; spontaneous bacterial empyema
SBEM articles; Hepatic hydrothorax articles; Cirrhosis articles; spontaneous bacterial empyema articles
Article Details
1. Introduction
Hepatic hydrothorax (HH) is described as the presence of a pleural effusion in patients with established evidence of liver cirrhosis or portal hypertension. Although it has prevalence of 5-12% in cirrhosis patient [1], the diagnosis of hepatic hydrothorax can be made if other etiologies of pleural effusion such as cardiovascular, pulmonary, rheumatologic, or malignancy are excluded. SBEM is described as the spontaneous development of an infectious process in the pleural fluid without any evidence of pneumonia or other systemic illnesses in patients with pre-existing hepatic hydrothorax. Although cases of SBEM are rare, it is important for clinicians to be mindful of its diagnostic complications and treatment as mortality rate can reach up to 20% without treatment [1].
2. Case Presentation
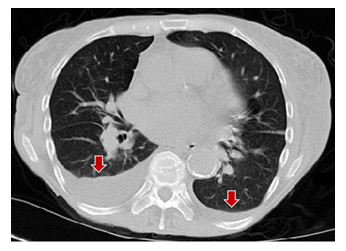
A 54-year-old female with a past medical history of decompensated liver cirrhosis with portal hypertension and recurrent ascites secondary to alcohol use disorder, recurrent bilateral pleural effusions (right more than left), who presented with new onset pleuritic chest pain, worsening dyspnea, epigastric abdominal pain, and acute encephalopathy lasting for 3 days. Pain was described as non-radiating, right sided chest pain that is relieved by lying on her right side. On admission, vitals were unremarkable except for tachycardia of 102 beats per minute. Physical examination revealed alert but not oriented. Lung exam showed decreased breath sounds on bilateral lower lung lobes. Abdomen was non-distended, negative for signs of fluid but had other stigmata of liver cirrhosis such as hepatosplenomegaly and skin findings. Her medication list included furosemide, spironolactone, thiamine, folic acid, pantoprazole, and multivitamin. Chest Xray showed mild cardiomegaly with bilateral pleural effusion (right > left). Computed Tomography (CT) thorax was performed, and it revealed moderate right and small left pleural effusions without any consolidation (Figure ). CT abdomen and pelvis showed increased liver nodularity, parenchymal heterogeneity and enlargement of portal veins corresponding to chronic liver disease. It also showed small perihepatic ascites without any liver mass and mild edema with inflammatory changes surrounding the distal pancreas. CT head was negative for acute changes. Serum amylase was 39 u/L, lipase was 15.6 u/L, liver function tests, kidney functions, electrolytes, B12, folate, TSH and ammonia level (20 ug/dL) were unremarkable. Thoracentesis of the right pleural effusion drained 700 ml of cloudy, purulent, dark brown fluid while the left pleural fluid was never tapped owing to very low volume of the pleural fluid.
Pleural fluid analysis showed total cell count 25391 cells/µL, white blood cell (WBC) 2391 cells/µL with neutrophils 33%, lymphocyte 25%, eosinophils 1%, mononuclear cells 41%, pH 7.28, glucose 103 mg/dl, albumin 1.8 g/dl, protein 4.5 g/dl, Lactate dehydrogenase (LDH) 217 U/L, fluid culture, grams stain and blood culture were negative. Cytology was negative for malignant cells. Pleural fluid protein to serum protein ratio of > 0.5 indicating exudative effusion. In addition, it revealed polymorphonuclear leukocytes (PMNs) >750 cells/µL with negative pleural fluid culture and serum to pleural fluid albumin gradient was 1.2 g/Dl. The final diagnosis was hepatic encephalopathy precipitated by SBEM. The patient was treated with ceftriaxone for five days resulting in the resolution of clinical symptoms. Patient’s previous fluid studies is highlighted in Table 1. At that time, multi-disciplinary team discussions (medicine, infectious disease and pulmonology) had concluded that the analysis findings were consistent with the diagnosis of uncomplicated hepatic hydrothorax and no treatment was recommended [2].
|
Serum |
Previous admission |
Current admission |
|
WBC (x103 /uL) |
8.5 |
9.2 |
|
Albumin (g/dL) |
3.3 |
3 |
|
LDH (u/L) |
278 |
150 |
|
Total Protein (g/dL) |
5.9 |
6.4 |
|
Blood cultures |
No growth |
No growth |
|
Pleural fluid |
||
|
Colour |
Orange/yellow |
Cloudy (purulent) and dark red/brown |
|
Appearance |
Hazy |
Cloudy |
|
Amount |
1300 ml |
700 ml |
|
Total cell count (cells/µL) |
1924 |
25391 |
|
White Blood Cell (cells/µL) |
924 |
2391 |
|
Differentials (%) |
Neutrophils 6%, Lymphocytes 10% |
Neutrophils 33%, Lymphocytes 25% |
|
Protein (g/dL) |
2.8 |
4.5 |
|
Albumin (g/dL) |
1.6 |
1.8 |
|
Serum-pleural albumin gradient (g/dL) |
1.7 |
1.2 |
|
Glucose (mg/dL) |
122 |
103 |
|
pH |
7.42 |
7.28 |
|
LDH (U/L) |
155 |
217 |
|
Gram stain |
Rare PMNs. No organisms. |
Few PMNs. No organisms. |
|
Fluid Culture |
No Growth |
No Growth |
|
Cytology |
--- |
Negative for malignant cells. |
Table 1: Biochemical and hematological investigations.
3. Discussion
Hepatic hydrothorax (HH) is described as the collection of significant pleural effusion, generally more than 500 ml, in a patient with end-stage liver disease without any underlying cardiac or pulmonary cause. It is an unusual complication of portal hypertension, with propensity to involve right lung in majority of the cases but can be left-sided or bilateral [3].SBEM, which is defined as the spontaneous infection of the pleural fluid, is a life-threatening complication of HH. A prospective study conducted by Xiol et al. reported that 43% of the episodes of SBEM in 120 cirrhotic patients with Hepatic Hydrothorax were not associated with Spontaneous Bacterial Peritonitis (SBP), thus making the diagnose more challenging [4].
SBEM remains to be underreported not only because patients with HH are rare in hospital settings but also because the diagnostic test, thoracentesis, is not routinely done in cirrhotic patients with hydrothorax. Although therapeutic thoracentesis can be advantageous in order to alleviate the symptoms of hepatic hydrothorax, the main disadvantage is that it can cause iatrogenic pneumothorax, which can be fatal. A prospective study conducted by Castellote et al revealed that there is an eight percent incidence of pneumothorax in post-thoracentesis patients who had liver cirrhosis complicated by hydrothorax, which only complicates to the diagnostic process [5].
There are multiple prognosticators for poor clinical outcome in patients with SBEM, which is important for clinicians to recognize as it will promote careful monitoring in particularly susceptible patients. They include high Model for End stage Liver Disease-Na (MELD) score, initial admission into the intensive care unit (ICU) and lastly, treatment failure with initial antibiotics [6]. In patients with hepatic hydrothorax who develop fever of unknown origin, worsening kidney functions, unexplained acute onset encephalopathy, or worsening pleuritic chest pain or shortness of breath, clinicians should have high degree of suspicion for the diagnosing SBEM. In such patients, early thoracentesis with fluid studies is warranted in order to identify the diagnostic criteria for SBEM which include (i) PMN count >250cells/µL with positive pleural fluid cultures or PMN count > 500 cells/µL with negative cultures, (ii) serum to pleural fluid albumin ratio >1.1g/dL or absence of other infectious etiologies on chest radiograph or CT and (iii) evidence of pleural effusion before the infectious episode or pleural fluid transudate characteristics during infection [7].
Although pathogenesis of SBEM is unknown, it is acknowledged that cirrhotic patients have impaired immune function secondary to decreased synthetic function of the liver, making them prone to infections and infection-related complications [8]. It was originally presumed that SBEM was the consequence of a direct translocation of bacteria from the peritoneal cavity into the pleural cavity through a diaphragmatic or other anatomical defect. However, later studies have revealed that about forty percent of the SBEM episodes were not associated with SBP and some episodes occurred without any evidence of ascites [7, 9]. In these cases, it was hypothesized that the underlying pathogenetic mechanism of SBEM was that transient bacteremia allowed organisms travel within the bloodstream and infect the pleural space. Studies done by Sese [9]have demonstrated that cirrhotic patients with hepatic hydrothorax have low ascites complement levels and opsonic activity, which enhances bacterial translocation. It can be hypothesized that defective local factors in pleuritic fluid can promote colonization by pathogenic bacteria, thereby enhancing risks for infection in these patients.Early studies by Sese also demonstrated that patients with lower total protein, lower levels of pleural fluid C3 and a higher Child-Pugh score were more prone to develop SBEM than their counterparts [9, 10].
Management of SBEM can be challenging due to poor liver function and renal dysfunction associated with cirrhotic patient. Use of third generation cephalosporin have shown promising effects [10]. Chest tube drainage is an alternative treatment option; the only indication includes formation of purulent materials in the pleural space [6]. If pus is not formed, chest tube drainage is not indicated for the treatment of SBEM even if fluid cultures are positive [6].
It is interesting to note that other treatment such as liver transplantation provided a good survival benefits in patients with recurrent SBEM. A prospective study performed by Xiol et al. have demonstrated that there were minimal or no variations in survival rates between a group of patients who had uncomplicated or non-refractory hydrothorax versus those who had refractory hydrothorax with recurrent SBEM requiring transplantation [11]. Although additional investigations are necessary to successfully evaluate the effectiveness of liver transplant in these patients, it can be inferred that transplantation can offer advantageous results and serve as an excellent therapeutic choice for cirrhotic patients with hydrothorax, even with or without the complications of SBEM.
Majority of pleural empyema is generally accompanied by low glycopleuria values while SBEM has characteristically high glycopleuria level. This case is peculiar in that the glycopleuria value was in the higher range (103 mg/dL) compared to what is characteristically seen in patients with SBEM. In a review article by Chaaban et al. [12] had suggested that the glycopleuria level in patients with SBEM can reach up to 80mg/dl which is particularly different when compared to the fluid studies in patients with pleural empyema, which is characterized by a low glucose level. Another significant finding in this case was that although traditional criteria of chest tube drainage were fulfilled, our patient with recurrent empyema did not require it and responded well to the antibiotic course.
4. Conclusion
SBEM can be easily missed. It is vital for physicians to include SBEM in the differential diagnosis in patients with HH who develop fever of unknown source, worsening renal functions or unexplained acute encephalopathy, especially if they have features related to poor outcome.
Acknowledgments
None.
References
- Garcia N, Mihas AA. Hepatic hydrothorax: pathophysiology, diagnosis, and management. Journal of clinical gastroenterology 38 (2004): 52-58.
- Lazaridis KN, Frank JW, Krowka MJ, et al. Hepatic hydrothorax: pathogenesis, diagnosis, and management. The American journal of medicine 107 (1999): 262-267.
- Roussos A, Philippou N, Mantzaris GJ, et al. Hepatic hydrothorax: pathophysiology diagnosis and management. Journal of gastroenterology and hepatology 22 (2007): 1388-1393.
- Xiol X, Castellvi JM, Guardiola J, et al. Spontaneous bacterial empyema in cirrhotic patients: a prospective study. Hepatology 23 (1996): 719-723.
- Castellote J, Xiol X, Cortes-Beut R, et al. Complications of thoracentesis in cirrhotic patients with pleural effusion. Revista Espanola de Enfermedades Digestivas: Organo Oficial de la Sociedad Espanola de Patologia Digestiva 93 (2001): 566-575.
- Tu CY, Chen CH. Spontaneous bacterial empyema. Current opinion in pulmonary medicine 18 (2012): 355-358.
- Allam NA. Spontaneous bacterial empyema in liver cirrhosis: an underdiagnosed pleural complication. Saudi journal of gastroenterology: official journal of the Saudi Gastroenterology Association 14 (2008): 43.
- Noor MT, Manoria P. Immune Dysfunction in Cirrhosis. Journal of clinical and translational hepatology 5 (2017): 50-58.
- Guarner C, Soriano G. Bacterial translocation and its consequences in patients with cirrhosis. European journal of gastroenterology & hepatology 17 (2005): 27-31.
- Sese E, Xiol X, Castellote J, et al. Low complement levels and opsonic activity in hepatic hydrothorax: its relationship with spontaneous bacterial empyema. Journal of clinical gastroenterology 36 (2003): 75-77.
- Xiol X, Tremosa G, Castellote J, et al. Liver transplantation in patients with hepatic hydrothorax. Transplant International 18 (2005): 672-675.
- Chaaban T, Kanj N, Akl IB. Hepatic Hydrothorax: An Updated Review on a Challenging Disease. Lung 197 (2019): 399-405.