Situation Analysis of Uncorrected Refractive Errors in Sub-Saharan Francophone African Countries
Article Information
Amassagou Dougnon1,*, Nouhoum Guirou1, Seydou Bakayoko1, Fatoumata Korika Tounkara1, Sadio Maiga1, Dolo Mathias1, Carole Melançon2, Lamine Traore1, Benoit Toussignant3, Kassoum Kayentao1
1University of Sciences, Techniques and Technologies of Bamako USTTB
2Optometrist Canada
3Montreal University
*Corresponding author: Amassagou Dougnon, University of Sciences, Techniques and Technologies of Bamako USTTB, Mali.
Received: 13 March 2022; Accepted: 21 March 2022; Published: 29 March 2022
Citation: Amassagou Dougnon, Nouhoum Guirou, Seydou Bakayoko, Fatoumata Korika Tounkara, Sadio Maiga, Dolo Mathias, Carole Melançon, Lamine Traore, Benoit Toussignant, Kassoum Kayentao. Situation Analysis of Uncorrected Refractive Errors in Sub-Saharan Francophone African Countries. Journal of Ophthalmology and Research 5 (2022): 48-65
Share at FacebookAbstract
Background: Uncorrected refractive errors (URE) are a serious public health problem by their magnitude, the multiple consequences they result in, but also by the inability of the countries of French-speaking Sub-Saharan Africa (FSSA) to meet the needs of the population. Governance problems, associated with human resources problems, financing problems for care, infrastructure and consumables, led us to initiate this study, the objective of which is to analyze the situation of UREs in FSSA with the stakeholders involved in the eye health system.
Materials and Methods: We carried out a cross-sectional survey of eye health actors and stakeholders in all of the French-speaking Sub-Saharan Africa countries from March 1st to August 31st, 2020. An online questionnaire was developed and translated into French, and then sent to the targeted eye health stakeholders involved in eye health. The survey and data collection were carried out in two phases: first by collecting information from the eye health officials of the countries which then enabled us to reach all the other actors in the country. Data were entered directly into SPSS 20 software followed by cleaning prior to analysis and presented as percent, mean or median, and standard deviation.
Result: A total of 500 questionnaires were sent to the various actors involved in eye health in the 21 countries of French-speaking Sub-Saharan Africa. The number of people who opened the questionnaire is 215, of which 151 have completed at least one question. Eye health policy documents existed in countries according to 95% of respondents. In the words of 76.6%, 54.6% and 85.2% of the participants respectively, the mechanisms for describing the tasks of the agents, for reporting to the actors and for collecting data existed. Also, according to respectively 61.5%, 58.8 % and 61.3% of respondents, the following are not effective: existence of documents of standard
Keywords
eye health French-speaking sub-Saharan Africa, eye health system, eye health policy, refractive error Sub-Saharan Africa, ametropia Africa, Management of vision disorders Sub-Saharan Africa
eye health French-speaking sub-Saharan Africa articles, eye health system articles, eye health policy articles, refractive error Sub-Saharan Africa articles, ametropia Africa articles, Management of vision disorders Sub-Saharan Africa articles.
Article Details
1. Intruduction
Uncorrected refraction errors (URE) are a severe public health problem in view of their magnitude and also by the multiple consequences they cause around the world. They are the leading cause of visual impairment and a major cause of blindness worldwide [1-3]. URE have consequences at both the individual and community level. Indeed, several studies have established the link between quality of life and visual impairment caused by refractive errors [4-11].
For those affected and their communities, these losses can lead to loss of education and employment status, reduced productivity, poor quality of life, reduced life expectancy, as well as an aggravating factor for the development of most lower-income countries [2,6,12-15].
Despite the uneven distribution of eye conditions by region, it is estimated that in Sub-Saharan Africa (SSA), UREs represent nearly 45% of the causes of vision disturbances and 13% of the causes of blindness [2,16]. With the impetus of the World Health Organization (WHO) and its partners, several SSA countries have signed the declaration of the Right to Sight Vision 2020 and adopted strategic documents to clearly define policies and national priorities in the field of eye health [17-19].
Despite all the efforts made by the actors involved in the partnership of the Vision 2020 objective, most SSA states remain far from achieving the sustainable development objectives related to the of the Right to Sight initiative [20-26].
The current observation is that the situation in French Sub-Saharan African (FSSA) countries remains even more worrying because of the mismatch between the growing needs of the population and current availability of eye health services [12,20,27-29]. The implementation of coordination strategies and the real weight of the eye health program in national health systems sufficiently demonstrated the limits of its governance policies [29].
Great efforts still need to be made in this region, in view of the galloping increase of the population and the multiple gaps such as the low level of access to existing eye care services, the often inadequate infrastructure and equipment, and the lack of human resources. Optometrists, who are key personnel in the screening and care of UREs, are quite numerous in the English-speaking SSA countries, but hardly appear in the public eye care systems of the FSSA countries.
Very few FSSA countries have recruited optometrists in public eye care structures, despite some availability of training for its human resources. Also, compared to the other linguistic regions of Sub-Saharan Africa, until 2020, the 21 FSSA countries only had two optometry training centers, in Mali and Cameroon, which does not allow the rate of UREs to be reduced and to dispose of this leading cause of visual disturbances [28,29].
It is clear that beyond the production of policy documents, most states in this region only contribute to the provision of premises and rely on the support of partners and non-governmental organizations (NGOs) which seem to be more involved in actions to combat visual impairment [3,25,30]. One of the characteristics of this region is also the lack of data on the real state of eye diseases. Very few FSSA countries have statistics on the prevalence of refractive errors in the population [25].
The few publications carried out either in schools or hospitals often indicate a lack of data for an entire region and do not allow the development of a management plan based on documented knowledge of the URE situation [31,32].
Governance problems, associated with human resources problems, financing problems for healthcare, infrastructure and consumables, led us to initiate this study, the objective of which is to analyze the situation of UREs in FSSA with the stakeholders involved in the eye health system.
2. Methods
2.1 Study design and framework
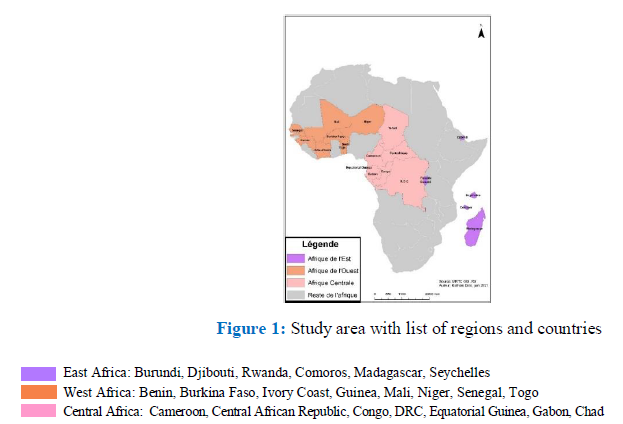
We carried out a cross-sectional and prospective survey of actors and stakeholders in eye health from all FSSA countries from March 1st to August 31st, 2020. The subdivision of regions and the list of countries are provided according to the classification of UNICEF and the FDA “French Development Agency” illustrated in figure 1. [33,34]
FSSA is made up of French speaking countries within SSA. These countries are characterized by their major delay in the implementation of actions to significantly reduce the rates of UREs. All these countries have in common a health system inherited from the former colonizer (France) and have similarities in their strategies and health indicators. In terms of the ratio of eye health human resources, none of the FSSA countries have the minimum required. Eye health programs in most countries have yet to provide for the integration of optometry into the eye health system [23,31,35-37].
Eye health care in FSSA countries is typically provided by NGOs, the private sector and the state. The health systems in these countries have a pyramidal structure comprising three levels (primary, secondary and tertiary) [38-40].
The primary level represents the operational unit of the health pyramid and is located in each health district to provide basic eye care and ensure hygiene education and awareness. The secondary level is responsible for the coordination, inspection, supervision and overall control of public and private health structures in a region. This level covers most eye conditions including surgery. The tertiary level, generally located in national hospitals, offers expertise and ensures training and research activities.
2.2 Study Population
In each country we applied the same process for the selection of targets:
The selection of primary targets: In the 21 countries of our study area, national coordinators (or managers) of eye health programs have been selected. The directory and contact of program coordinators was facilitated by the Mali Eye Health Coordinator. In some countries, when the coordinator or his assistant could not be contacted, we used the network of former students of the university center of the tropical ophthalmology institute of Africa (CHU-IOTA) (doctors, nurses or optometrists) to collect country information. The role of primary targets was to provide the list and addresses of actors and partners in eye health (ophthalmologists, optometrists, opticians, nurse ophthalmologists and NGOs) allowing the selection of secondary targets to participate in the survey.
Selection of secondary targets: In order to avoid redundancies, we have adopted a general rule of reasoned choice on a case-by-case basis. For ophthalmologists and optometrists, we selected five respondents per country from the list provided by the primary target of the country. In the event of more than five actors designated by specialty, we carried out a random drawing and all were selected if the list included less than five people. For ophthalmic technicians and opticians, we selected six agents per specialty from the list provided by the primary target of the country.
As this staff is generally the most numerous in the eye health system, we made a reasoned choice taking into account the geographical distribution of the agents who are often the best distributed in the regions. In case there were more than six regions in a country, a random choice was applied. In the event that there were less than six agents, we have retained the available staff. For technical and financial partners (NGOs) in eye health, we contacted the main representatives whose list was provided by the primary target of the country. In the event that a country had more than ten eye health partners, we randomly selected ten for our study.
2.3 Inclusion and exclusion criteria
We included in this survey all the actors of eye health active at the time of the survey and working in FSSA. Those not working at the time of the survey or working outside our study area were excluded.
2.4 Data Collection Techniques and Methods
An online questionnaire was developed based on the WHO Eye Care Service Assessment Tool (ECSAT) [41,42].
The questionnaire that was developed mainly took into account aspects related to UREs Before sending the questionnaire to collect the data, all the tools developed were translated into French and underwent the pre-tests with trainees in training at CHU-IOTA during the survey period, in order to refine their reliability and their validity and to ensure the quality of the data collected which allowed us to make formulations for the questions.
The survey and data collection were carried out in two phases:
We collected information from primary targets contacted by email and in some cases it was necessary to go through telephone calls to collect data on eye health resources and the list of NGOs and eye health partners. Collection of information by online questionnaire from all targets according to a predefined grid (see appendix) which takes into account the six chapters of the eye health systems assessment tool: (Leadership and governance, human resources, financial resources, delivery of eye care services, infrastructure and equipment, and information system) [41,42].
Before its implementation, the study protocol had been approved by the ethics committee of the Faculty of Medicine and Odonto-stomatology and that of the Faculty of Pharmacy (letter reference N° 2019/47/CE/FMPOS). Informed consent was obtained from all participants who received the questionnaire before answering the questions.
The questionnaires sent by email were accompanied by an informed consent form that had to be accepted before responding. We made several follow-up emails and often phone calls to encourage participants to complete the questionnaire.
2.5 Data management and analysis
All responses to the questionnaire were reviewed to identify likely filling errors. Then, data was entered directly into SPSS 20 software followed by cleaning before analyses. Data were presented as percentage, mean or median, and standard deviation.
3. Results
In total, 500 questionnaires were sent to the various actors involved in eye health in the 21 countries of FSSA. Among the 215 actors who opened the questionnaire, 151 completed at least one question. No actor from Equatorial Guinea, Rwanda or Seychelles opened the questionnaire. The countries that most participated in the survey were Mali, 20.5% (31/151), Côte d'Ivoire, 13.2% (20/151) and the Democratic Republic of Congo, 9.9% (15/151).
3.1 Leadership and governance
Respondents reported the existence of most of the mechanisms such as the eye health program manager at 95.2%, the organization chart of the program at 71.4% and the structures responsible for the dissemination of documents up to 75.0%. On the other hand, the existence of the documents on standards and procedures for the management of the UREs is not known according to 61.5% of respondents and the use of the management procedures by the directors is not as well-known to 45% of participants. (Table 1)
3.2 Finance
According to 59% of respondents a specific allocation to eye health does not appear in the budget of the Ministry of Health. (Table 1) Also, during the preparation of the documents of the national eye health committee, 2/3 of the respondents considered that the participation of actors outside the health system (education, finance) in the development of the programs was non-existent or not known. (Table 1)
3.3 Human resources
The job description was defined according to the positions held according to 76.6% of the respondents and 56.6% stated that they had benefited from continuous professional training since taking up their position, even though 61.3% of the respondents felt that there was no obligation to have continuing education in their career. The government has not taken enough measures for the geographic distribution and the implementation of strategies for human resource development, according to 45.9% and 39.2% of respondents, respectively. (Table 1)
3.4 Service delivery
Among the respondents, 55.5% said that their structure did not have an eyewear supply unit and 58.8% of them said that the costs of eyewear equipment were not affordable. The non-availability of low vision services and the non-existence of an equipment maintenance policy were reported by 57.6% and 55.5% of participants, respectively (Table 1).
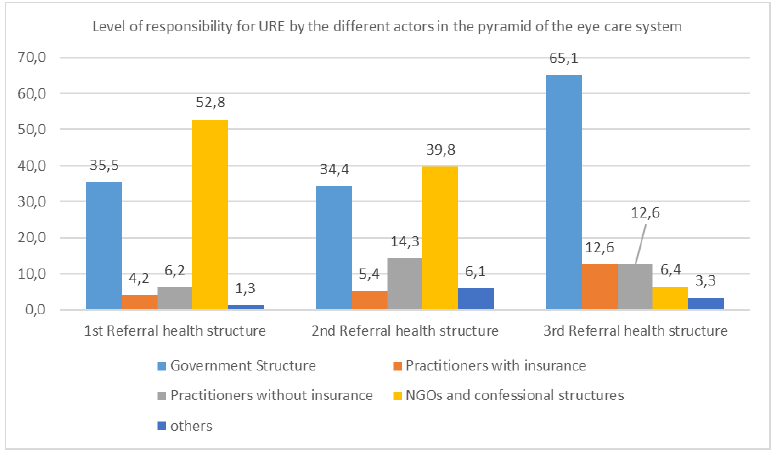
In the different levels of the health pyramid system, government structures play the leading role at the 3rd level of the pyramid in 65.1% while NGOs and faith-based structures occupy the leading role at the 1st and 2nd level of the pyramid in 52.8% and 39.8%, respectively (Figure 2).
Level of responsibility for URE by the different contributors in the pyramid of the eye care system
3.5 Information system
Although 85.2% of respondents stated the existence of a register to collect patient data, 61.5% of them also stated the unavailability of data for each patient at the level of the structures and 59.3% reported that there is no specification for refractive errors as a diagnosis in the report documents produced. (Table 1)
Table 1: Description of procedures, mechanisms and services in eye health programs
|
Theme / Intervention |
Yes |
No |
Unknown |
|
Leadership and governance |
|||
|
Existence of an eye health program manager |
20 (95.2) |
1 (4.8) |
|
|
Existence of an eye health program flowchart |
15 (71.4) |
5 (23.8) |
1 (4.8) |
|
Existence of a structure responsible for disseminating documents |
6 (75.0) |
0 (0.0) |
2 (25.0) |
|
Existence of standards and procedures documents for URE |
9 (34.6) |
16 (61.6) |
1 (3.8) |
|
Use of standards and procedures documents by actors |
4 (44.5) |
2 (22.2) |
3 (33.3) |
|
Existence of intervention for URE service increase |
20 (80.0) |
5 (20.0) |
|
|
Existence of administrative management procedure |
10 (45,5) |
7 (31,8) |
5 (22,7) |
|
Use of management procedures by managers |
6 (30,0) |
5 (25,0) |
9 (45,0) |
|
Existence of funding mechanism |
5 (22,7) |
9 (40,9) |
8 (36,4) |
|
Existence of reporting mechanism |
12 (54,6) |
5 (22,7) |
5 (22,7) |
|
Eye health program performance |
11 (52,3) |
9 (42,9) |
1 (4,8) |
|
Finances |
|||
|
Specific eye health allocation in the health ministry budget |
3 (17,7) |
10 (58,8) |
4 (23,5) |
|
Participation of other actors in the national eye health committee |
5 (31.2) |
5 (31.2) |
6 (37.6) |
|
Human Resources |
|||
|
Existence of task description for agents |
59 (76,6) |
16 (20,8) |
2 (2,6) |
|
Possibility of access to continuing education |
43 (56,6) |
33 (43,4) |
|
|
Existence of worker motivation plan |
36 (47,4) |
36 (47,4) |
4 (5,3) |
|
Existence of HR development strategies |
25 (33,8) |
29 (39,2) |
20 (27,0) |
|
Existence of measures for the geographical distribution of HR |
22 (29,7) |
34 (46,0) |
18 (24,3) |
|
Existence of continuous training obligation for HR |
22 (29,3) |
46 (61,3) |
7 (9,4) |
|
Service delivery |
|||
|
Existence of eye glasses supply unit |
15 (45,5) |
18 (55,5) |
|
|
Affordability of the cost of eye glasses equipment |
14 (41,2) |
20 (58,8) |
|
|
Maintenance policy existence |
15 (45,5) |
18 (55,5) |
|
|
URE case referral system |
17 (50,0) |
16 (47,1) |
1 (2,9) |
|
Existence of low vision service |
12 (36,4) |
19 (57,6) |
2 (6,0) |
|
Availability of a health insurance program |
23 (67,6) |
11 (32,4) |
|
|
Affordability of Eye Exam Costs |
18 (54,5) |
13 (39,4) |
2 (6,1) |
|
Existence of computerized health information system |
7 (24,1) |
20 (69,0) |
2 (6,9) |
|
Information system |
|||
|
Existence of patient registry |
23 (85,2) |
3 (11,1) |
1 (3,7) |
|
Regular data entry |
17 (63,0) |
7 (25,9) |
3 (11,1) |
|
Existence of data for each patient |
9 (34,6) |
16 (61,5) |
1 (3,89) |
|
Specification of RE in reports |
10 (37,0) |
16 (59,3) |
1 (3,7) |
|
Country data collection and centralization |
9 (32,2) |
13 (46,4) |
6 (21,4) |
|
Existence of an eye health survey for 5 years |
8 (29,6) |
10 (37,1) |
9 (33,3) |
|
Existence of computerized periodic reports on eye health |
6 (22,2) |
12 (44,5) |
9 (33,3) |
3.6 Infrastructures and Equipment
Most respondents stated that basic eye exam materials were available in their facility. (Table 2)
Regarding the materials for the spectacles workshop, their availability in the various structures was not effective in a large proportion (Table 2).
Table 2: Description of the material and equipment situation for the responsibility of URE
|
Equipment / Materials |
Exists and functional n(%) |
Exists and not functional n(%) |
does not exist n(%) |
|
Equipment for eye exams |
|||
|
Distance visual acuity chart |
26 (89,7) |
3 (10,3) |
|
|
Trial lenses |
27 (93,1) |
2 (6,9) |
|
|
Trial frames |
26 (89,7) |
1 (3,4) |
2 (6,9) |
|
Retinoscope |
16 (59,3) |
2 (7,4) |
9 (33,3) |
|
Ophthalmoscope |
24 (85,7) |
4 (14,3) |
|
|
Auto-refractometer |
22 (81,5) |
1 (3,7) |
4 (14,8) |
|
Phoroptor (Refractor) |
7 (29,2) |
1 (4,2) |
16 (66,7) |
|
Visual acuity chart projector |
19 (70,4) |
1 (3,7) |
7 (25,9) |
|
Slit lamp |
22 (78,6) |
2 (7,1) |
4 (14,3) |
|
Others (eye exam materials) |
3 (50,0) |
3 (50,0) |
|
|
Eyewear workshop equipment |
|||
|
Lensometer |
21 (77,8) |
6 (22,2) |
|
|
Manual grinder |
10 (45,5) |
12 (54,5) |
|
|
Semi-automatic grinder |
6 (30,0) |
2 (10,0) |
12 (60,0) |
|
Automatic grinder |
5 (25,0) |
1 (5,0) |
14 (70,0) |
|
Glass stock |
12 (52,2) |
2 (8,7) |
9 (39,1) |
|
Frame stock |
13 (56,5) |
1 (4,4) |
9 (39,1) |
|
Tool set (pliers, screwdriver) |
13 (56,5) |
10 (43,5) |
|
|
Pupillometer |
12 (54,5) |
10 (45,5) |
|
|
Others (tools for optical stores) |
2 (22,2) |
7 (77,8) |
|
4. Discussion
This study is aimed to provide a portrait of the system for managing UREs in FSSA, that should be integrated into the eye health care system. This WHO recommendation is a strategy for combating visual impairment and blindness [2,3]. Despite several positive points that emerge from the study, the first most obvious finding is the marked mismatch between the theoretical existence of health care policies including the management of UREs and the reality on the ground. These gaps can be found in governance, as well as in financial, human and infrastructure resources. In relation to leadership and governance in the global eye health care system, the study finds that in FSSA countries, the structures and essential documents that govern eye health policies exist according to 70% participants in the questionnaire. This finding is consistent with a recent study carried out in eight countries in SSA which concluded that countries had eye health programs in place and that they mostly had eye health policy documents aligned with the global strategy of eye health.[25]
The National Eye Health Strategic Plan document [43-45] seems to be the most widely used reference document in the various countries (43% of respondents). Usually the result of an internal consultation process, it therefore seems to better reflect the will of the national actors involved in the eye health system. Concerning more specifically the aspect of refractive error management, 57.1% of respondents specify that aspects relating to the management of refractive errors are clearly mentioned in these documents. These documents, in theory, should make it possible to provide effective answers to the problems of visual impairments encountered.
In addition to these policy documents, most survey participants (80.0%) attest that countries are adopting intervention strategies to broaden refraction error management services. This result is consistent with several studies that have demonstrated initiatives and actions aimed at detecting refractive errors, especially in schools, despite the frequent lack of human resources and expertise in the field.[17,19]
The analysis of the level of appropriation of policies by the actors involved in the eye health system paints a glowing but above all theoretical picture. Indeed, 65.4% of respondents are unaware of the existence of documents of standards and procedures for the management of refractive errors.
A more disappointing observation was that the respondents attesting to the existence of these documents claimed not to use them. A similar finding is reported by previous studies that revealed the lack of consistency between policy documents designed to operate in accordance with professional standards and the reality on the ground. [31,46,47]
The explanation suggested by these authors is in line with our own. There appears to be a mismatch between the reality on the ground and these documents, which do not take into account the routine activities relating to the functioning of the services and the constant interactions between the population and the health workers.[26,48-50]
In addition, 80% of respondents stated that the insufficient use of these reforms or policy documents would be due to a lack of involvement of other actors in the health system such as education and finance during their development. Another factor could be the lack of leadership within state and health care structures, which can undermine the motivation of health system actors in the implementation of these projects or policies. In fact, more than half of the participants were unaware or did not perceive the existence of a real motivation plan in the workplaces, even though their workload seemed reasonable. Studies have shown that this is justified by the fact that some managers at the head of eye health departments were not sufficiently equipped for the position, therefore with gaps in the coordination and improvement of motivation plans.[30,51-54]
We see the same kind of inconsistency when we analyze the financial side of the question: funding does not support the implementation of intervention programs or strategies to reduce visual impairments and blindness related to refractive errors. 58,8% of the respondents affirm that in the budgets of the ministries of health, the specific allocation to eye care does not exist while 77.3% of them ignore the mechanisms for financing eye health. The results of our study are in agreement with several assessment reports of eye health systems or in the strategic planning documents of countries such as Mali, Togo, Burkina Faso, the Comoros and Senegal [25,39,40,43,44,55].
This is how NGOs, instead of States, are called upon to assume the leading role in the management of refractive errors at the primary and secondary level of the health pyramid of health systems. Private structures, with or without insurance, operate at all levels of the health pyramid in proportions ranging respectively from 10.4% at the primary level to 25.1% at the tertiary level. (Figure 2) Governments intervene for the majority of cases at the tertiary level of the health system (65.1%) and constitute the second force at the primary and secondary level. This observation has been made by several authors who note that the contribution of states in eye care is generally the provision of premises and human resources, relying on the fact that several non-governmental partners support actions to combat blindness.[25,29]
Also, whether it takes place in government structures or in private structures, the costs of services related to refractive errors are borne by patients according to 64.7% and 88.2% of respondents, respectively. We know, from the respondents (67.6%), the existence of certain national or private health insurance programs in the countries, but cannot estimate their effectiveness at the level of all populations. In faith-based eye health structures or NGOs, nearly half of patients benefit from free access to certain care or services [25,26,30].
In our study, even if the majority of the participants (54.5%) assert that the costs related to the eye exam are within the reach of the population, the cost of the spectacle equipment seems to be high and not-affordable for the populations according to 69.7% of respondents in addition to recurring availability problems. The authors also agree in affirming that this constitutes one of the barriers to access to healthcare for the population, and partly justifies the major intervention of the partners in this field.[30,42,45,56] In addition to the costs associated with the provision of glasses, our study also reveals that the service is only available for half of the respondents and that in cases where the service is available, more than 54.5% say they do not have one of the essential equipment for cutting corrective lenses, which would reduce costs to patients.
The second observation in this study relates to the absence of a human resources development plan which results in the lack of access to professional care linked to URE, including examinations, the supply of glasses and low vision services.
Our study clearly demonstrates the lack of accessibility to care related to visual impairments and low vision, even though NGOs and the private sector seem to be involved in the eye health system. Beyond the costs that hinder accessibility, 67.6% of respondents' state that care is only available in large cities and more than half of respondents (55.5%) affirm that several care structures do not have a spectacle supply unit.
Our results intersect the information of several authors who mention that tertiary level care structures are generally those which have the most complete eye health offers, but in our French-speaking countries of sub-Saharan Africa, they exist only in capitals and some large cities.[25,30]
In addition, low vision services do not exist, according to 57.6% of respondents, and the cost of low vision services is largely assumed by patients according to 44% of respondents and by non-governmental actors according to 28% of them. However, the recommendations of the WHO are clear and aim to establish low vision units at all levels of the health pyramid. The reality on the ground shows a huge deficit in this provision.[56,57]
In the FSSA countries, the definition of the tasks of these main services in the eye health and visual impairments team seems to be accepted and the inter-collaboration is assumed because where it exists, the health actors are trained in the same structures and together ensure complete patient care including refractive errors. The example of the training of ophthalmologists, ophthalmology nurses and optometrists at the CHU-IOTA in Bamako is an integrating model example that facilitates collaboration between the different actors in eye health. [58] Recognized professional associations exist for ophthalmologists and ophthalmic nurses in different countries according to 90.9% and 71.4% of respondents respectively.
The International Occupational Classification (ISCO-08) recognizes ophthalmologists, ophthalmic nurses, optometrists, opticians and orthoptists as typical eye health personnel. [59] By their job definition, optometrists are important actors in the management of UREs.
Our study shows that the complete eye health team is not effective in all of French-speaking Sub-Saharan Africa: not only more than 60% of the structures in these countries do not have an optometrist according to the respondents, but 58% are even unaware of their formal existence. References in case of need for refractive error management exist according to 50% of respondents. However, clear data has demonstrated the need for competent and sufficient human resources to ensure the diagnosis and complete management of refractive error cases. [23,25,35,43,46,52,60-62]
Therefore, it is not surprising to find, in our study, that 66.2% of respondents do not know whether there is a strategic plan for human resources development. Likewise, almost half (46%) consider that the government is not taking enough measures to ensure that the distribution of eye health professionals meets the needs of regions or countries. Respondents (79.2%) also mention that educational institutions that train eye health professionals have very little involvement in the development of government plans and strategies for eye care human resources.
Finally, one last observation is required regarding the significant gaps related to the information system: this effects on the one hand the lack of data on patients, and on the other hand, the dissemination of existing information to stakeholders of the care system in terms of URE management procedures. Few periodic health information reports exist in these countries and those that do exist are not known to stakeholders according to 77.7% of respondents.
We observed that according to more than 70.3% of respondents, different countries have not organized a national public health survey including data on refractive errors for 5 years, hence difficulties in planning, monitoring and evaluating programs, epidemiological studies, in this space.
As part of this study, we first contacted the coordinators of the national eye health programs in order to have their adherence and backing for the conduct of the work. In the 21 countries of FSSA, only 5 countries have answered clearly and favourably. In order to continue the work, and we had to use an informal network of eye health actors (ophthalmologist, ophthalmology technician, and optometrist) trained at the CHU-IOTA in Bamako in Mali.
Through these contacts, with more than 500 emails sent, only 215 people opened the questionnaire. This followed reminder emails and several phone calls when the actors involved in this investigation were already familiar to each other. In the end, 151 people out of 500, answered at least one question; i.e. a response rate of 30.2%.
Eye care facilities generally have data collection records according to 85.2% of respondents and 63% say the records are properly documented. And according to 82.1% of respondents, internal periodic reports are published. However, a high proportion of respondents (59.3%) believe that a particular specification on refractive errors does not appear in these reports while more than 80% of the same respondents claim that diagnoses and patient profiles are the most common variables collected. This raises the question of the importance accorded by actors in the eye care system to refractive and low vision conditions.
From a global point of view, it appears that despite the existence of registers in most services, the collection and centralization of country data is not effective. It also emerges that government health structures are the main providers of health information, followed by NGO structures. Studies show that the levels of eye health data collection and dissemination depend on countries and partners who tend to collect data related to their own target. [25,30,56]
The limitations of this study include the limited number of participants. However, we believe that the selection bias is somewhat minimized since each category of stakeholders has been represented and the three countries that did not respond have geographic, economic and population similarities with other countries who participated in the survey.
In addition to this, the quality and the concordance of certain answers seem to include possible biases related to self-reporting due to respondents' interpretation of the standards to be given on the information. However, compared to face-to-face questionnaires which may lead to higher social desirability bias, these may be inferior.[63]
5. Conclusion
Although policy documents that comply with standards exist in the French-speaking area of SSA, several challenges remain to be taken up, in particular the involvement of all actors in the health system, the strengthening of governance, financial resources and human resources, as well as the information and supply system for materials and consumables.
It therefore becomes important to highlight the underlying problems of health systems which are often poorly understood by our usual techniques of quantitative data collection. Fine qualitative surveys could help us make a more in-depth diagnosis by taking into account all the interactions and allow decision-makers to make more informed decisions for the proper implementation of health systems policies.
Abbreviation's list
- AFD: “French Development Agency”
- ECSAT: Eye Care Service Assessment Tool
- FMPOS: Faculty of Medicine and Odonto-stomatology and that of the Faculty of Pharmacy
- FSSA: French Sub-Saharan African
- ISCO: International Occupational Classification
- NGO: Non-governmental organization
- URE: Uncorrected refraction errors
- CHU-IOTA: University center of the tropical ophthalmology institute of Africa
- SSA: Sub-Saharan Africa
- WHO: World Health Organization
Declarations
Acknowledgements
The authors thank the coordinators (managers) of the eye health programs in French-speaking sub-Saharan Africa for their valuable contribution to this survey.
Authors’ contributions
AD: was the principal investigator from the conception until the final version of the article
FKT; BT; KK: made contributions to analysis and interpretation of data and ensured the follow-up of the process
LT: facilitated contact with eye health program coordinators and data collection
MDs: ensured the production of maps of the study area
CM: ensured the translation of documents and the follow-up of the whole process
NG; SB; SM: ensured a proofreading and correction of the document
All authors made substantial contributions to conception, design and follow-up.
Funding
None
Availability of data and materials
The data that support the findings of this study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Faculty of Medicine and Odonto-stomatology and that of the Faculty of Pharmacy (letter reference N° 2019/47/CE/FMPOS) and complied with the Declaration of Helsinki. All participants should accept and sign the informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
All the authors declare that they have no competing interests.
References
- Abner G, Mario SP, and Myhill C et al., “EFA Global Monitoring Report Regional Overview-Monitoring the Education for All goals:Sub-saharan Africa,” J. Vis. Impair. Blind 1 (2012): 1–14, 2012.
- World Health Organization, World report on vision 214 (2019): 14.
- Burton Matthew J, Ramke Jacqueline, Marques Ana Patricia, Bourne Rupert RA, Congdon Nathan, Jones Iain Ah Tong, et al, “The Lancet Global Health Commission on Global Eye Health: vision beyond 2020,” The Lancet Global Health 9 (2021): e489–e551.
- Latorre-Arteaga S, Gil-González D, Enciso O, Phelan A, García-Muñoz A, and Kohler J. “Reducing visual deficits caused by refractive errors in school and preschool children: Results of a pilot school program in the Andean region of Apurimac, Peru,” Glob. Health Action 7 (2014).
- Resnikoff S, Pascolini D, Mariotti SP, and Pokharel GP. “Global magnitude of visual impairment caused by uncorrected refractive errors in 2004.,” Bull. World Health Organ. 86 (2008): 63–70.
- Nutheti Rishita, Shamanna Bindiganavale R, Nirmalan Praveen K, Keeffe Jill E, Krishnaiah Sannapaneni, Rao, Gullapalli N, et al. “Impact of impaired vision and eye disease on quality of life in Andhra Pradesh,” Investig. Ophthalmol. Vis. Sci 47 (2006): 4742–4748.
- Kymes SM and Lee BS. “Preference-based quality of life measures in people with visual impairment.,” Optom. Vis. Sci 84 (2007): 809–816.
- D. DJADI-PRAT J*, SARAGOUSSI JJ, LEBUISSON DA, ARSON B, “Traduction et validation d’une échelle de qualité de vie relative à la réfraction (NEI-RQL 42),” J. Fr. Ophtalmol 32 (2009): 1S36.
- Dandona L and Dandona R. “What is the global burden of visual impairment?,” BMC Med 4 (2006).
- McCarty CA, “Uncorrected refractive error,” British Journal of Ophthalmology, vol. 90, no. 5. BMJ Publishing Group 90 (2006).
- WHO, “GLOBAL INITIATIVE FOR THE ELIMINATION OF AVOIDABLE BLINDNESS” (2007).
- Mashayo ER, Chan VF, Ramson P, Chinanayi F, and Naidoo KS. “Prevalence of refractive error, presbyopia and spectacle coverage in Kahama District, Tanzania: a rapid assessment of refractive error,” Clin 98 (2015): 58–64.
- Mathenge W, Nkurikiye J, Limburg H, and Kuper H, “Rapid assessment of avoidable blindness in western Rwanda: Blindness in a postconflict setting,” PLoS Med 4 (2007): 1187–1194.
- Yamey and P. Hotez, “Neglected tropical diseases,” BMJ Br. Med. J 335 (2007): 269–270.
- World Health Organization WHO/PBL/97.61 Rev2, “Prevention of Blindness and Deafness: Global initiative for the elimination of avoidable blindness” (2000).
- Sabanayagam C and Cheng CY, “Global causes of vision loss in 2015: are we on track to achieve the Vision 2020 target?,” The Lancet Global Health 5 (2017): e1164–e1165.
- Faal H, C. G.-C. E. Health, and undefined 2007, “Convincing governments to act: VISION 2020 and the Millennium Development Goals,” ncbi.nlm.nih.gov, Accessed: (2020).
- Joseph Enyegue Oye and J. Enyegue Oye, “South west province eye care programme, Cameroon,” Community EyE Heal. J. 18 (2005).
- Evans JR, Morjaria P, and Powell C, “Vision screening for correctable visual acuity deficits in school-age children and adolescents,” Cochrane Database Syst. Rev (2018).
- Naidoo Kovin, Gichuhi Stephen, Basáñez María-Gloria, Flaxman Seth R, Jonas Jost B, Keeffe Jill, et al., “Prevalence and causes of vision loss in sub-Saharan Africa: 1990–2010,” Br. J 98 (2014): 612–8.
- United Nation, General Assembly Seventy-fifth session “Vision for Everyone: accelerating action to achieve the Sustainable Development Goals A/75/L.108 - E - A/75/L.108 -July 2021,” . Accessed: (2021).
- Gilbert C et al. “Standard Guidelines for Comprehensive School Eye Health Programs.” [Online].
- WHO Regional Office for Africa, “Core Competencies for the Eye Health Workforce in the WHO African Region” (2019).
- International Agency for the Prevention of Blindness IAPB, Standard school eye health guidelines for low and middle-income countries, IAPB School Eye Health Work Group, International Agency for the Prevention of Blindness February (2018).
- Bechange S, Jolley E, Virendrakumar B, Pente V, Milgate J, and Schmidt E. “Strengths and weaknesses of eye care services in sub-Saharan Africa: a meta-synthesis of eye health system assessments,” BMC Health Serv Res 20 (2020): 381.
- Sukati VN, Moodley VR, and Mashige KP, “A situational analysis of eye care services in swaziland,” J. Public Health Africa 9 (2018).
- Didier Gobbers, Éric Pichard, “L ’ organisation du système de santé en Afrique de l ’ Ouest,” adsp n° 30 mars (2000): 35–42, 2000.
- Naidoo K, Kempen JH, Gichuhi S, Braithwaite T, Casson RJ, Cicinelli MV et al. “Prevalence and causes of vision loss in sub-Saharan Africa in 2015: Magnitude, temporal trends and projections,” Br. J. Ophthalmol (2020).
- Alain Faujas, “Africa: Why Francophones are lagging behind Anglophones | News & Analysis,” THE AFRICA REPORT (2012).
- Lewallen S and Kello AB. “The need for management capacity to achieve VISION 2020 in Sub-Saharan Africa,” PLoS Medicine 6 (2009):12.
- Etya’ale D, Ackland P, Mason I, and Hopkins A. “Santé Oculaire Communautaire: Au-delà de VISION 2020?: mettre progressivement en place aujourd’hui les équipes de soins oculaires de demain,” cehjournal.org 9 (2012): 1–3.
- Graham, “Facing the crisis in human resources for eye health in sub-Saharan Africa,” Community Eye Health Journal 30 (2018): 85–87.
- Unicef, Classifications unicef pour La Situation des enfants en Afrique 2008, sur la base des regroupements régionaux des Nations Unies “Sous-régions et régions d’Afrique” (2008).
- Ernesto Hernández-Catá, Afrique subsaharienne Politique économique et perspectives de croissance 1998. Finances & Développement / Mars (1999).
- Palmer, F. Chinanayi, A. Gilbert, … D. P.-H. resources for, and undefined 2014, “Trends and implications for achieving VISION 2020 human resources for eye health targets in 16 countries of sub-Saharan Africa by the year (2020)”.
- Poz MRD, Gupta N, Quain E, and Soucat AL. “Manuel de suivi et d’évaluation des ressources humaines pour la santé: comprenant des applications spécialement adaptées aux pays à revenu faible ou intermédiaire,” World Heal. Organ (2009): 207.
- Sightsavers, “Stratégie de Santé Oculaire de Sightsavers (2013-2018).”
- KOUKPO, “SANTE PUBLIQUE AU SEIN DE LA CEDEAO A LA SUITE DE L’INITIATIVE DE BAMAKO?; EVALUATION ET ADAPTATION DES POLITIQUES DE SANTE Rapport (2014).
- Ministry of Health of Mali, Sightsavers, Mali Eye Health Systems Assessment Report (2017).
- Sarr B, Badu E, Bocoum S, Jolley E, and Schmidt E. “Eye Health Systems Assessment (EHSA) in Senegal,” (2018).
- WHO, “Eye care service assessment tool ECSAT,” WHO (2015).
- WHO, Catalogue of key eye health indicators in the African Region (2017).
- MINISTERE DE LA SANTE PROGRAMME NATIONAL DE LUTTE CONTRE LA CECITE, “PLAN STRATEGIQUE NATIONAL ‘VISION 2020’ - 2015-2019 - TOGO” (2015).
- Ministere de la sante Burkina Faso, “Plan strategique integre de lutte contre les maladies non transmissible (2014-2018)”.
- Ministre de la Santé et de la Lutte contre le Sida COTE D’IVOIRE, “STRATEGIE NATIONALE DE FINANCEMENT DE LA SANTE POUR TENDRE VERS LA COUVERTURE UNIVERSELLE,” Côte d’Ivoire (2012).
- Faal H, “Services de prise en charge des amétropies?: former du personnel pour répondre aux besoins,” Rev. Santé Ocul. Communaut 5 (2008).
- Etya’ale Daniel, “Accès aux soins oculaires: mieux et autrement,” Rev. Santé Ocul. Communaut 4 (2007): 25–48.
- Daniel Etya’ale. “Mise en œuvre des soins oculaires primaires: comment procéder en pratique,” REVUE DE SANTÉ OCULAIRE COMMUNAUTAIRE | VOLUME 7 | NUMÉRO 8 | JANVIER (2010). Accessed: Jul. 26, (2018).
- Lavigne Delville P, “Une politique publique de santé et ses contradictions. La gratuité des soins au Burkina Faso, au Mali et au Niger,” Cah. Etud. Afr 225 (2017): 196–198.
- Pente V et al., “Task-shifting eye care to ophthalmic community health officers (OCHO) in Sierra Leone: A qualitative study,” Journal of global health 11 (2021): 07001.
- Naidoo K, “Poverty and blindness in Africa,” Clin. Exp. Optom 90 (2007): 415–421.
- Etya’ale Daniel, “Accès aux soins oculaires: mieux et autrement,” Rev. Santé Ocul. Communaut (4): 25–48.
- Lewallen S et al, “Factors affecting cataract surgical coverage and outcomes: a retrospective cross-sectional study of eye health systems in sub-Saharan Africa,” BMC Ophthalmol 15: 67.
- du Toit, A. Palagyi, and G. Brian, “The development of competency-based education for mid-level eye care professionals: A process to foster an appropriate, widely accepted and socially accountable initiative,” Educ. Heal. Chang. Learn. Pract 23 (2010): 7.
- UNION DES COMORES, “POLITIQUE NATIONALE DE SANTE ( PNS ) Comores” (2005).
- World Health Organization, “Catalogue of Key Eye Health” Cat. key eye Heal. Indic. African Reg (2017): 1–59.
- Ryan B, “Models of low vision care: past, present and future,” Clin. Exp. Optom., 2014, Accessed: Sep. 14, (2015).
- Carole Melançon, Amassagou Dougnon et Abdulaye Diallo, « La naissance de la profession d’optométriste au Mali », L'Optometriste, janvier/février (2011).
- INTERNATIONAL STANDARD CLASSIFICATION OF OCCUPATIONS ISCO-08. Structure, group definitions and correspondence tables? Volume 1, International Labour Office - Genava:ILO (2012).
- Courtright, W. Mathenge, A. B. Kello, C. Cook, K. Kalua, and S. Lewallen, “Setting targets for human resources for eye health in sub-Saharan Africa: what evidence should be used?,” Hum. Resour. Health 14 (2016): 11
- International Agency for the Prevention of Blindness, “Standard Guidelines for Comprehensive School Eye Health Programmes,” 2018. Accessed: (2021).
- Palmer JJ et al., “Mapping human resources for eye health in 21 countries of sub-Saharan Africa: current progress towards VISION 2020,” Hum. Resour. Health 12 (2014): no. 1, p. 44, Jan. 2014, doi: 10.1186/1478-4491-12-44.
- M.-È. Gingras and H. Belleau, “Avantages et Désavantages du Sondage en Ligne comme Méthode de Collecte de Données?: une Revue de la littérature,” Montréal Canada, May 2015. Accessed: Oct. 07, (2021).