Serum Free T4 Concentration: More Accurate and Reliable than TSH as an Indicator of Thyroid Gland Function
Article Information
Ashraf K Mena1, Udaya M Kabadi1, 2*
1Veterans affairs A Medical Center, Phoenix, US
2Broadlawns Medical Center, University of Iowa College of Medicine, Iowa, US
*Corresponding author: Udaya M Kabadi, Chief, Endocrinology, Broadlawns Medical Center, Adjunct Professor of Medicine, University of Iowa, Iowa City, Des Moines University, Des Moines, 1801 Hickman Road, IA 50314, US
Received: 21 December 2020; Accepted: 29 December 2020; Published: 06 January 2021
Citation:
Ashraf K Mena, Udaya M Kabadi. Serum Free T4 Concentration: More Accurate and Reliable than TSH as an Indicator of Thyroid Gland Function. Archives of Internal Medicine Research 4 (2021): 001-008.
Share at FacebookAbstract
Objective: To compare the accuracy and reliability of Free T4 or TSH determination as the single initial screening test in assessment of thyroid function.
Methods: Retrospective review of 3,022 thyroid function tests (free T4 and TSH) performed during a 12 month period in a laboratory at a major academic medical center was conducted. A probable diagnostic category for each test was determined by a retrospective detailed review of medical records of subjects with discrepant serum free T4 and TSH concentrations.
Results: In 284 tests (9.4%) the appropriate diagnosis could not be arrived at if serum TSH concentration alone was used for interpretation of thyroid function. Alternatively, serum free T4 concentration alone was unable to provide accurate diagnosis in 132 (4.4%) subjects. Multivariate analysis determined that free T4 is more reliable than TSH as an initial test for the diagnosis of thyroid function as expressed by odds ratio (OR) 2.14 with confidence interval (CI) 1.96 - 2.34, p< 0.01. The sensitivity and specificity for diagnosis of thyroid disorder were superior for Serum free T4 concentration (91% and 94%) respectively when compared with serum TSH level (84% and 86%). However, the sensitivity and specificity for both laboratory tests assessed in conjunction improved further ( 98% for both) in comparison to either of the tests evaluated individually in diagnosis of thyroid disorder.
Conclusions: Free T4 may be more accurate and reliable than TSH as a single initial screening laboratory test in assessment of thyroid function. However, both performed simultaneously increases the reliability and accuracy in determination of thyroid functional state.
Keywords
Thyroid Function, Free T4, TSH, Free T3
Thyroid Function articles; Free T4 articles; TSH articles; Free T3 articles
Article Details
1. Introduction
The function of the thyroid gland involves synthesis, storage and release of thyroid hormones, thyroxine and triiodothyronine akin to any other endocrine gland. Historically, serum total T4 measurement was performed. Total T4 is a combination of physiologically appropriate free T4 and inactive T4 bound to proteins and therefore is not likely to be reliable test in assessment of thyroid function.
Probably therefore, serum TSH concentration was and continue to be recommended as an initial screening laboratory test to assess a functional thyroid disorder in the population by major organizations including American Association of Clinical Endocrinologists, American College of Endocrinology, American Thyroid Association, Endocrine Society, American association of Family Practice, American College of physicians, College of American Pathologists [1-7].
However, comparative data regarding utility of Free T4 and TSH as a single initial test in determination of thyroid function in the literature is sparse. Therefore, we compared accuracy and reliability of serum free T4 or TSH concentration as an initial screening laboratory test in interpretation of thyroid function in a large population of subjects at an academic medical center. We also examined the accuracy and precision of both tests assessed in conjunction simultaneously in determination of thyroid function.
2. Methods
The study was approved by institutional review board at the medical center. Retrospective review of 3,022 thyroid function tests (serum free T4 and TSH concentrations) performed in adults during a 12 month period in a laboratory at a major academic medical center was conducted. We determined a probable diagnostic category of thyroid function by concurrent examination of both serum free T4 and TSH concentrations according to guidelines of American Association of Clinical Endocrinologists, American College of Endocrinology and American Thyroid Association as well as extensive literature review [8-19]. Detailed examination of medical records of subjects with abnormal serum free T4 and/ or TSH levels was conducted to establish diagnoses of the most likely thyroid functional disorder in these subjects.
Serum Free T4 and TSH concentrations were determined by a commercial kit* based on Micro particle Enzyme Immunoassay (MEIA) technology (IMX free T4 assay, IMX ultrasensitive human TSH assay, Abbott Diagnostics, Inc., Abbott Park, Illinois). The comparison between free T4 and TSH for precise diagnosis were conducted by determining Odds Ratios (OR) with multivariate analysis. Sensitivity and specificity indices for accurate and precise diagnosis of thyroid function were also determined for either serum free T4 or TSH concentration individually or both tests in conjunction.
3. Results
Normal range of values established previously in the laboratory for serum Free T4 and TSH levels were 0.71-1.85 ng/dl and 0.5-5 ulu/ml respectively. Simultaneously, lowest levels determined by the assays were for serum Free T4 and TSH levels were 0.40 ng/dl and 0.003 uU / ml respectively. Both serum Free T4 and TSH concentrations were within normal ranges established previously by the laboratory in 2412 blood samples indicating thyroid state, Serum free T4 was subnormal and TSH was > 20 uU/ ml in 67 blood samples indicating definitive presence of primary hypothyroidism. 52 blood samples with supernormal Free T4 and suppressed TSH concentration (< 0.01mU/ml) established the diagnosis of primary hyperthyroidism.
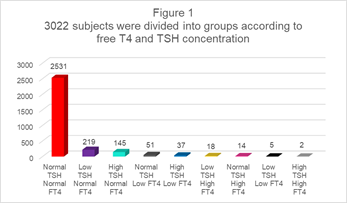
Thus, the appropriate diagnosis of thyroid function could be arrived at with utilizing either serum free T4 or TSH concentration and confirmed by application of both tests in 2531 blood samples. However, in 491 blood samples, either serum Free T4 and/ or TSH concentration were abnormal though not consistent with definitive diagnoses of a euthyroid state, primary hypothyroidism or primary hyperthyroidism (Figure 1). These abnormal tests included the following groups: 1) normal free T4 and subnormal TSH (Table1), 2) normal free T4 and elevated TSH (Table 2), 3) low free T4 and normal TSH (Table 3), 4) High Free T4 and normal TSH (Table 4), 5) low freeT4 and low TSH (Table 5), 6) high free T4 and high TSH (Table 6).
|
Category |
Number of tests |
|
Hyperthyroidism |
3 |
|
Euthyroid on Synthroid replacement or Suppression |
120 |
|
Euthyroid on prednisone |
48 |
|
Euthyroid on antidepressant medications (Fluoxetine, sertraline, tricyclic antidepressants, i.e., desipramine hydrochloride) |
17 |
|
Euthyroid with non-thyroidal illness* |
22 |
|
Graves’ or MNTG following antithyroid Rx |
6 |
|
Euthyroid with etiology undetermined |
3 |
*Hospitalized subjects
Table 1: Specific diagnostic categories for 219 tests, showing normal free T4 and low TSH concentrations.
|
Category |
Number of subjects |
|
Subclinical hypothyroidism |
89 |
|
Recovery of subacute thyroiditis |
5 |
|
Recovery of non-thyroidal illness |
16 |
|
Euthyroid on metoclopramide |
3 |
|
Reset thyrostat* |
32 |
*Hospitalized subjects
Table 2: Specific diagnostic categories for 145 tests, showing normal free T4 and high TSH.
|
Category |
Number of tests |
|
Central Hyperthyroidism |
11 |
|
Non-Thyroidal illness* |
20 |
|
Euthyroid on Dilantin |
3 |
|
Euthyroid on salsalate |
12 |
|
Graves’ or MNTG following antithyroid Rx |
4 |
|
Euthryoid with etiology undetermined |
1 |
*Hospitalized subjects
Table 3: Specific diagnostic categories for 51 tests, showing low free T4 and normal TSH.
|
Category |
Number of Tests |
|
Hyperthyroidism |
4 |
|
Euthyroid on heparin |
3 |
|
Non-thyroidal illness* |
5 |
|
Graves’ or MNTG following antithyroid Rx |
2 |
*Hospitalized subjects
Table 4: Specific diagnostic categories for 14 tests, showing high free T4 and normal TSH.
|
Category |
Number of Tests |
|
Central hypothyroidism |
1 |
|
Non-thyroidal illness* |
2 |
|
Graves’ or MNTG following antithyroid Rx |
2 |
*Hospitalized Subjects
Table 5: Specific diagnostic categories for 5 tests, showing low free T4 and low TSH.
|
Category |
Number of Tests |
|
Central Hyperthyroidism |
1 |
|
Hypothyroid on amiodarone* |
1 |
*due to lack of conversion of T4 to active T3
Table 6: Specific diagnostic categories for 2 tests, showing high free T4 and high TSH.
In subjects with these incongruous or indeterminate abnormal results, the diagnoses of thyroid disorder was established on extensive review of medical records based on guidelines recommended by various organizations as well as review of the literature [6-18]. With these abnormal results, Serum TSH concentration alone failed to document appropriate diagnosis of the thyroid disorder in 284 (9.4%) subjects. Alternatively, the measurement of serum free T4 concentration alone was unable to provide accurate diagnosis in 132 (4.4%) subjects. Multivariate analysis for appropriate diagnosis of thyroid function in these subjects documented Odds Ratio (OR) 2.14 with confidence Interval (CI) 1.94- 2.28 in favor of Free T4 concentration compared to TSH level. Finally, the accurate diagnosis was documented in 419 out of 436 (97%) subjects if both tests were utilized simultaneously for assessment of thyroid function. Thus, sensitivity indices for serum TSH or Free T4 individually and if used in conjunction for establishing accurate diagnoses of thyroid disorder were 84%, 91% and 98 % respectively. Specifically indices were 86% for serum TSH, 94 % for serum Free T4 and 98% using both tests together in arriving at the accurate diagnosis of the thyroid disorders.
4. Discussion
Serum TSH concentration is presently recommended as a screening laboratory test for diagnosis of thyroid dysfunction by several reputed organizations [1-7]. Determination of serum Free T 4 level is recommended to be determined only in presence of abnormal serum TSH concentration. This study demonstrates that diagnosis of thyroid dysfunction is likely to be inaccurate in majority of subjects if based on subnormal serum TSH concentration alone. The most frequently considered diagnosis of ‘sub clinical’ hyperthyroidism is likely to be erroneous in many subjects [10, 11, 13, 15, 17-23]. The states with low TSH include central hypothalamic or hypopituitary hypothyroidism, euthyroid sick state, euthyroid Graves' disease, multinodular nontoxic goiter with autonomous nodules prior to as well as following antithyroid drug therapy, euthyroidism on levothyroxine replacement or suppressive therapy, euthyroidism with a single autonomous or hot nodule as well as drug induced decline of serum TSH level. Similarly, minor elevation (<10 uU/ ml) of serum TSH level is not always an expression of subclinical primary hypothyroidism [8-10, 17-23]. Moreover, minor elevation of TSH with normal Free T4 Levels in elderly may not be ‘true’ subclinical hypothyroidism since therapy with levothyroxine is likely to result in shortening survival [24-26]. Thus, it is apparent that Free T4 level is more accurate than TSH in determination of effective thyroid gland function in the elderly. Alternatively, normal serum TSH level may not indicate normal thyroid function especially in subjects with abnormal free T4 concentration [17-23].
Finally, management of thyroid dysfunction based on determination of serum TSH level alone is likely to pose challenges. Daily dose of levothyroxine is often increased repeatedly based on persistently unchanged elevated serum TSH level. Documentation of lack of appropriate rise in serum free T4 level unravels lack of compliance, inappropriate administration or rarely, a lack of absorption of levothyroxine. Moreover, daily levothyroxine dose is unfortunately frequently reduced because of low TSH in subjects with central hypothyroidism due to presumptuous presence of primary hypothyroidism on the part of the providers [26]. Similarly, in subjects with hyperthyroidism determination of serum TSH level alone without concurrent assessment of serum free T4 concentration is unlikely to provide efficacy of therapy with antithyroid drugs or post radioiodine therapy as serum TSH is better correlated with circulating thyroid stimulating immunoglobulin when compared with either Free T4 or Free T3, [13, 17, 27]. Finally, this study also demonstrated that serum TSH concentration was less sensitive or specific in comparison to serum free T4 level as single diagnostic laboratory test in assessment of thyroid function. The superiority of Free T4 may be attributed to it being a true expression of thyroid gland function. In contrast, serum TSH level denotes the physiologic effect of thyroid hormones primarily T3 on secretion of TSH by the pituitary thyrotrophs as well as release of thyrotropin releasing hormone (TRH) by the hypothalamus. Thus, serum TSH level is an index of function of pituitary thyrotrophs. Therefore, simultaneous determination of both free T4, an expression of thyroid gland function and TSH level, an expression of thyroid hormone function provide the most accurate diagnosis in almost all subjects.
Therefore, in conclusion, determination serum TSH concentration alone may be inaccurate and unreliable as a single laboratory test in assessment of thyroid function and therefore may not be utilized as a screening test irrespective of the assay methodology since serum TSH concentrations determined by 3rd generation supersensitive assay or 2nd generation assay were not significantly different [29]. Serum Free T4 level instead appears to be a more reliable and precise in diagnosis of thyroid disorder. However, we believe that, both serum free T4 and TSH concentrations must be performed simultaneously for most accurate determination of thyroid functional state. Occasionally, determination of serum Free T3 and Reverse T3 concentrations may be required for establishing accurate diagnosis of hypothalamic or hypo pituitary hypothyroidism [28, 30].
References
- Roti E, Gardini E, Magotti M G, et al. Are thyroid function tests too frequently and inappropriately requested?. J Endocrinol Invest 22 (1999): 184-190.
- Megan J DiFurio. This newsletter is produced in cooperation with the College of American Pathologists’ Public Affairs Committee (2005).
- Henry Burch, David Cooper, Jeffrey Garber, et al. Hyperthyroidism and other Causes of Thyrotoxicosis: Management Guidelines of the American Thyroid Association and American Association of Clinical Endocrinoloigists. Endocrine Practice 17 (2011): 456-520.
- Jeffrey Garber, Rhoda Cobin, Hossein Gharib, et al. Clinical Practice Guidelines for Hypothyroidism in Adults: Cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocrine Practice 18 (2012): 988-1028.
- S. Preventive Services Task Force. Screening for Thyroid Dysfunction: Recommendation Statement. Am Fam Physician 91 (2015).
- Michael L LeFevre. U.S. Preventive Services Task Force Screening for thyroid dysfunction: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 162 (2015): 641-650.
- Ross DS, Burch HB, Cooper DS, et al. American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid 26 (2016): 1343-1421.
- Kabadi UM. Subclinical Hypothyroidism: Natural Course of the Syndrome during a Prolonged Follow up Study. Arch Intern Med 153 (1993): 958-961.
- Kabadi UM. Cech R.: Normal Thyroxine and Elevated Thyrotropin Concentrations: Evolving Hypothyroidism or Persistent Euthyroidism with Reset Thyrostat. Endochrinol. Invest 20 (1997): 319-326.
- Kabadi, UM. Thyrotropin Dysregulation during a Non-Thyroidal Illness: Transient Hypothalamic Hypothyroidism?. Journal of Endocrinological Investigation 24 (2001): 178.
- Kabadi, UM. Impact of corticosteroids on thyroid-stimulating hormone. The Journal of Musculoskeletal Medicine 18 (2001): 343.
- Huber G, Staub JJ, Meier C, et al. Prospective study of the spontaneous course of subclinical hypothyroidism: prognostic value of thyrotropin, thyroid reserve, and thyroid antibodies. J Clin Endocrinol Metab 87 (2002): 3221-3226.
- Mark Helfand. U.S. Preventive Services Task Force Screening for subclinical thyroid dysfunction in nonpregnant adults: a summary of the evidence for the U.S. Preventive Services Task Force Ann Intern Meds 20 140 (2004): 128-141.
- Papi G, Pearce EN, Braverman LE, et al. A clinical and therapeutic approach to thyrotoxicosis with thyroid-stimulating hormone suppression only. Am J Med 118 (2005): 349-61.
- Kabadi UM. Role of Thyrotropin in Metabolism of Thyroid Hormones in Non-Thyroidal Tissues. Metabolism Clinical & Experimental 55 (2006): 748-750.
- Papi G, Uberti ED, Betterle C et al. Subclinical hypothyroidism. Curr Opin Endocrinol Diabetes Obes 14 (2007): 197-208..
- Sharma S, Kabadi UM. Euthyroid Sick Syndrome. Primary Care Reports 14 (2008): 1-12.
- Leung AM, Braverman LE. Iodine-induced thyroid dysfunction. Curr Opin Endocrinol Diabetes Obes 19 (2012): 414-419.
- Lee S, Farwell AP. Euthyroid Sick Syndrome. Compr Physiol 6 (2016): 1071-1080.
- Cavalieri R R. The effects of nonthyroid disease and drugs on thyroid function tests, Review. Med Clin North Am 75 (1991): 27-39.
- Koulouri O, Moran C, Halsall D, et al. Pitfalls in the measurement and interpretation of thyroid function tests. Best Pract Res Clin Endocrinol Metab 27 (2013): 745-762.
- Irene Campi, Danila Covelli, Carla Moran, et al. The Differential Diagnosis of Discrepant Thyroid Function Tests: Insistent Pitfalls and Updated Flow-Chart Based on a Long-Standing ExperienceFront. Endocrinol 11 (2020): 432.
- Shui-Boon Soh, Tar-Choon Aw. Laboratory Testing in Thyroid Conditions - Pitfalls and Clinical Utility. Ann Lab Med 39 (2019): 3-14.
- Alon Grossman, Ilan Feldhamer, Joseph Meyerovitch. Treatment with levothyroxin in subclinical hypothyroidism is associated with increased mortality in the elderly. Eur J Intern Med 50 (2018): 65-68.
- Manuel R Blum, Baris Gencer , Luise Adam, et al. Impact of Thyroid Hormone Therapy on Atherosclerosis in the Elderly With Subclinical Hypothyroidism: A Randomized Trial. J Clin Endocrinol Metab 103 (2018): 2988-2997.
- Owain Leng, Salman Razvi. Hypothyroidism in the older population. Thyroid Res 12 (2019): 2.
- Maria Fleseriu, Ibrahim A Hashim, Niki Karavitaki, et al. Hormonal Replacement in Hypopituitarism in Adults: An Endocrine Society Clinical Practice Guideline. Journal of Clinical Endocrinology & Metabolism 101 (2016): 3888-3392.
- Kabadi UM. Serum Thyrotropin in Graves’ disease: a more reliable index of circulating thyroid stimulating immunoglobulin (TSI) level than thyroid function?. Endocrine Practice 13 (2007): 615-619.
- Kabadi UM, Fox I. Comparison Between Serum TSH Determination by 2nd and 3rd Generation TSH Assays. Endocrine Practice (1997): 284-286.
- Kabadi UM. Low Reverse T3: A Reliable, Sensitive and Specific in Diagnosis of Central Hypothyroidism. American Thyroid Association (2019).