Role of National Public Health Institutes for a Stronger Health System in Africa
Article Information
Haftom Taame Desta*, 1, Natalie Mayet2, Alex Riolexus Ario3, Raji Tajudeen1
1Africa Centers for Disease Control and Prevention (Africa CDC), African Union Commission
2National Institute for Communicable Diseases (NICD), South Africa
3International Association of National Public Health Institutes -Africa (IANPHI)
*Corresponding author: Haftom Taame Desta, Africa Centers for Disease Control and Prevention (Africa CDC), African Union Commission.
Received: 07 December 2022; Accepted: 15 December 2022; Published: 26 December 2022
Citation: Haftom Taame Desta, Natalie Mayet, Alex Riolexus Ario, Raji Tajudeen. Role of National Public Health Institutes for a Stronger Health System in Africa. Fortune Journal of Health Sciences 5 (2022): 603-609.
Share at FacebookAbstract
Background: Functional National Public Health Institutes (NPHIs) are critical for effective surveillance, outbreak detection and response, provision of specialized diagnostic services, research and capacity building to guide health policies and strategies through science and data. Many countries in Africa lack fully functioning NPHIs and remain ill prepared to respond to public health threats with the required speed and agility.
Objective: The main objective of this study was to map and generate information on the status of NPHI establishment in Africa, understand the legal frameworks used by the countries to establish NPHIs, and describe the different models of NPHIs on the continent.
Methods: A semi-structured questionnaire was administered online by the Africa CDC between 18 July 2021 and 26 May 2022. Data were collated, filtered and analyzed using Microsoft Excel and Arc GIS for mapping of NPHI establishment status by country. Informed consent was obtained from all participating institutions.
Result: Of the 55 African Union Member States, 40 (72.7%) responded to the online survey. Among the member states that responded, 12 reported being fully established, 17 indicated that they were at an advanced stage, six (6) had started the process, and five (5) reported not having a plan to develop an NPHI. Among the fully established and advanced-stage NPHIs, 17 (58.6%) are autonomous and semiautonomous, three (10.3%) are a network of institutions, and nine (31%) are structured as departments under the Ministries of Health. The most common functions of the NPHIs are research (26), surveillance and disease intelligence (24), epidemic preparedness and response (24), workforce development (19), public health informatics (15), and health promotion (10).
Conclusion: Success in building strong health systems in Africa requires countries to have strong
Keywords
NPHI, legal framework, public health functions, fully established
Article Details
1. Introduction
NPHIs are science-based institutions responsible for the coordination of public health functions nationally, including disease surveillance, epidemic preparedness and response, research, laboratory diagnosis, health workforce development, and other health-related functions [1-3]. Functional NPHIs are critical for effective outbreak response, guiding health policies and strategies through science and data, building health workforce capacity, accelerating the implementation of the International Health Regulations (2005), and implementing a robust disease surveillance system [4-6].
Establishing and maintaining a strong NPHI facilitates the effective and efficient implementation of national and international health-related commitments. NPHI provides the platform for the coordination of resources and health-related information, sometimes sharing laboratory and office infrastructure and providing scientific and epidemiology capacity and expertise [7]. NPHIs have been found to be a sound and viable model for low-resource countries to strengthen national public health infrastructure and capacity to competently address current and imminent public health threats. NPHIs also create a central focus for human resources in public health and provide a career path and nucleus of public health professionals to carry out core functions. Moreover, experience from developing countries has demonstrated that established NPHIs are a resource for national health security. Thus, the role of well-functioning NPHIs becomes essential for crisis management and to improve health outcomes [8-9]. Most countries in Africa lack fully functioning NPHIs and are less prepared to respond to public health threats [10-11]. The development and structure of NPHIs in Africa varies from country to country. The spectrum ranges from countries with no organized, government-led public health functions to those with fully developed NPHIs. The International Association of National Public Health Institutes (IANPHI) has a stage development tool that countries can use to assess the stage of development for different core functions of an NPHI [12].
The African CDC in collaboration with the IANPHI, the United States Centers for Disease Control and Prevention (US-CDC) and other partners has taken a number of steps to strengthen existing NPHIs, support the efforts of countries establishing an NPHI, and advocate for NPHI development in countries where one does not exist. Some of the efforts include conducting high-level advocacy, providing onsite mentorship and technical assistance, and developing standard documents to guide and monitor the establishment and development of NPHIs in Africa. It has developed two key documents, the Framework for establishing an NPHI and the Legal Framework for instituting the NPHIs [1,13], and advocated for the networking of NPHIs on the continent for timely information and experience sharing through various mechanisms, such as the NPHI Expert Task Team at Africa CDC, IANPHI and the Regional Integrated Surveillance and Laboratory Network (RISLNET).
The main objective of this study was to map and generate information on the status of NPHI establishment in Africa, understand the legal frameworks used by the countries to establish NPHIs, and describe the different models of NPHIs on the continent.
2. Materials and Methods
A semi-structured questionnaire was administered online to the Directors of NPHIs or their equivalent institutions in all 55 African Union Member States between 18 July 2021 and 26 May 2022. To improve the response rate, we made several follow-ups and had in-person meetings with focal persons in the respective countries. Data were collated, filtered and analyzed using Microsoft Excel and Arc GIS for mapping of NPHI establishment status by country.
For the purpose of analysis, autonomous and semiautonomous institutions are categorized together and are defined as a single institution established with a national legal framework by an Act of Parliament, Presidential decree or Ministerial/Cabinet decree to nationally coordinate and lead at least the following functions: Disease Surveillance, Laboratory Diagnosis, Emergency Preparedness and Response, and Public Health Research. A network of institutions is an institution or unit that is established with a legal framework to coordinate public health functions falling under or being conducted by other parastatal institutions at the national level. The network of institutions is different from autonomous/semiautonomous institutions in such a way that the public health functions for the network of institutions fall into more than one operationally and technically independent institution. Legal frameworks for the establishment of the NPHIs referring to Cabinet decisions, Prime-Minister/President’s decrees, and Regulations are considered as Ministerial decree.
The objectives and purpose of the study were stated at the beginning of the survey questionnaire to seek informed consent, and all participants agreed to participate and completed the survey.
3. Results
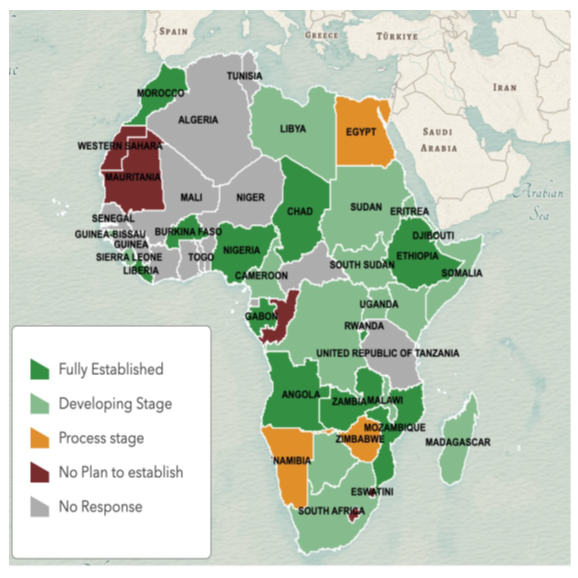
Of the 55 African Union Member States, 40 (72.7%) responded to the online survey. The highest response rate was from countries in the Southern Africa Regional Collaborating Centers (RCCs), where all 10 member states submitted responses. This was followed by countries from East Africa (85.7%, 12), Central Africa (77.7%, 7), West Africa (40%, 6), and North Africa (71.4%, 5). Among the members states that responded, 12 reported being fully established, 17 advanced stage, six (6) starting the process, and five (5) as not having a plan to develop an NPHI. Regional distribution of the fully established NPHI covers Southern Africa (Zambia, Mozambique, and Angola), West Africa (Nigeria, Burkina Faso, Liberia), Central Africa (Burundi, Chad, Gabon), East Africa (Ethiopia, Djibouti), and North Africa (Morocco). Countries that do not have a plan to establish NPHI include Lesotho, Eswatini, Congo, Mauritania, and Saharawi Arab Republic. See Figure 1.
Among the NPHIs that are fully established and at an advanced stage of development, 12 were established by an Act of Parliament, 12 by a Presidential decree, and 5 by a Ministerial decree. See Table 1.
Table 1: Legal frameworks used to establish NPHIs in Africa
|
NPHIs Established by |
||
|
Act of Parliament |
Presidential/ Prime-Minister Decree |
Ministerial Decree |
|
Djibouti |
Angola |
Cameroon |
|
Gabon |
Burkina Fasso |
DRC |
|
Liberia |
Burundi |
Mauritious |
|
Zambia |
Morroco |
Sudan |
|
Botswana |
Chad |
Ethiopia |
|
Cabo Verde |
Mozambique |
|
|
Eritrea |
Nigeria |
|
|
Guinea Bissau |
Kenya |
|
|
Malawi |
Libya |
|
|
Somalia |
Nigeria |
|
|
South Africa |
Uganda |
|
|
South Sudan |
Madagascar |
|
Table 1 shows the different legal frameworks used to establish NPHIs among countries with fully established NPHIs or in advanced stages of development.
Three models of NPHIs were identified: autonomous and semiautonomous institutions, networks of institutions, and departments under the Ministry of Health. Seventeen (17) NPHIs were autonomous and semiautonomous, four (04) network of institutions, and eight (08) were structured as a department under the Ministries of Health, as shown in Table 2. Of the well-established and developing NPHIs, 19 have strategic plans partially funded by governments. The government covers on average 40% (range: 1-95%) of the total NPHI’s annual budget, although it varies from country to country.
Table 2: Three types of NPHI models commonly used in Africa
|
Autonomous |
Network of Institutions |
Department under MoH |
|
Botswana |
DRC |
Angola |
|
Burkina Fasso |
Kenya |
Chad |
|
Burundi |
Djibouti |
Gabon |
|
Cabo Verde |
Uganda |
Cameroon |
|
Ethiopia |
Eritrea |
|
|
Guinea Bissau |
Mauritious |
|
|
Liberia |
Chad |
|
|
Morocco |
Sudan |
|
|
Mozambique |
||
|
Nigeria |
||
|
Zambia |
||
|
Libya |
||
|
Malawi |
||
|
Nigeria |
||
|
Somalia |
||
|
South Africa |
||
|
South Sudan |
Table 2 shows the three models of NPHIs that are commonly used in Africa. These include autonomous/semiautonomous institutions, a network of institutions and a department under the Ministry of Health responsible for core public health functions at the national level.
The most common functions of NPHs are research (26), surveillance and disease intelligence (24), epidemic preparedness and response (24), workforce development (19), public health informatics (15), and health promotion (10), as depicted in Table 3.
Table 3: Core functions of NPHIs by country. (The core mandates of the NPHIs are conducting surveillance and disease intelligence, emergency preparedness and response, public health research, laboratory diagnosis and systems, workforce development, public health informatics, and health promotion).
|
Country |
Surveillance |
EPR |
Research |
Laboratory |
Workforce |
Public Health Informatics |
Health Promotion |
|
Botswana |
Yes |
Yes |
Yes |
Yes |
No |
No |
No |
|
Cabo Verde |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Cameroon |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
No |
|
DRC |
Yes |
Yes |
Yes |
Yes |
No |
No |
No |
|
Eritrea |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Guinea Bissau |
No |
No |
No |
Yes |
No |
No |
No |
|
Kenya |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
No |
|
Libya |
No |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Malawi |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
|
Mauritious |
Yes |
Yes |
Yes |
No |
No |
Yes |
Yes |
|
Nigeria |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
|
Somalia |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
No |
|
South Africa |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
|
Sudan |
No |
No |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Uganda |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Madagascar |
No |
No |
Yes |
No |
Yes |
No |
Yes |
|
Angola |
Yes |
Yes |
Yes |
Yes |
No |
No |
No |
|
Burkina Fasso |
Yes |
Yes |
Yes |
Yes |
No |
No |
No |
|
Burundi |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Morroco |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
Yes |
|
Chad |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
No |
|
Djibouti |
Yes |
Yes |
Yes |
Yes |
No |
No |
No |
|
Ethiopia |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
|
Gabon |
Yes |
No |
Yes |
Yes |
No |
No |
No |
|
Liberia |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Mozambique |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
No |
|
Nigeria |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
|
Zambia |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
4. Discussion
In response to a question about the establishment status of NPHI, 18 countries indicated that they have a fully established NPHI. Deep diving to the information given, only 12 satisfy the definition for a fully established NPHI stated in the Africa CDC Framework for the development of NPHIs, which refers to a fully established NPHI as an autonomous or semiautonomous network of institutions mandated to conduct at least functions related to disease surveillance, emergency preparedness and response, laboratory systems, and research at the national level with full operational capacity and independence [9]. Countries such as Eritrea, Gabon, and Sudan have established their institutions as a department under the Ministry of Health, and the latter two countries do not have disease surveillance, emergency preparedness and response as core functions, while Libya and Guinea Bissau have networks of institutions without disease surveillance and laboratory systems as their core functions. A study conducted by the WHO indicated that 39 countries in Africa have well-established NPHIs, of which 28 are members of the International Association of National Public Health Institutes (IANPHI) [14]. These countries include Libya, Egypt, Sudan, Somalia, Kenya, Zimbabwe, Botswana, South Africa, Cameroon, Madagascar, and Tanzania. However, these countries responded to our survey that their NPHIs are either in the developing stage or on process. The discrepancy can be attributed to the difference in defining NPHI as an example Kenya Medical Research Institute (KEMRI), the National Institute for Communicable Diseases (NICD) and Center Pasteur du Cameroun have been established since the early 1900` but have been established to provide activities only for communicable disease [15-17]. This was a similar development to the United States Centers for Disease Control and Prevention (US CDC), which was initially established in 1946 to reduce the burden of malaria [18]. Second, there is also variation in the definition of what a fully established NPHI is. More than one NPHI in a country can be accepted as a member of the IANPHI, which implies that a country can have more than one institution responsible for leading and coordinating essential public health functions at the national level, while the African CDC promotes a single coordinating body or contact point at the national level. Moreover, membership in the IANPHI is not an automatic qualification to be a fully established NPHI for the African CDC unless it fulfills the minimum requirements. Only 72.5% of the African Union Member States have NPHIs that are either fully established or in a developing stage, which necessitates that the CDC and developing partners enhance their support to ensure that every Member State has a funded, sustainable NPHI with a full capacity and capability to respond to any public health emergencies in the country. Additional efforts are required from the African CDC and other partner organizations to encourage and support countries, especially those that do not have a plan to establish one through continuous engagement and advocacy with the countries’ leadership.
Success in building strong health systems in Africa requires countries to have strong public health institutions. NPHIs are science-based government institutions with clearly defined legal mandates that provide focused and centralized leadership and coordination for the specific public health functions detailed above. Among countries that responded to the survey, eight (20%) structured their NPHIs as a department under the Ministries of Health with limited freedom to make independent decisions. To carry out their responsibilities independently, make decisions or recommendations merely based on science and evidence, directly deal with external partners for health, and provide prompt responses to priority public health issues in their respective countries, NPHIs need to have full or some level of technical and operational autonomy. The fact that five (12.5%) of the countries that responded to our survey have no plan to establish an NPHI demands further investigation and active engagement with countries’ leadership to explore reasons and understand the resourcing requirements for advancement.
Limitations of the Study
The findings of this study are based on information collected through a self-administered questionnaire, which could be liable to information bias. As nine (09) countries from West Africa did not respond to the survey, it was difficult to have a full picture of the NPHI development status in the region. Moreover, the questionnaire was only in English, which might have contributed to the lower response rate among Francophone West African countries. The study took almost 10 months to complete. Acknowledging that the survey was conducted at the peak of the COVID response, the delay in response may not reflect that NPHI establishment could have advanced in the interim.
Conclusion
Success in building strong health systems in Africa requires countries to have strong public health institutions. The establishment and advancement of NPHI development is complex and not a static process. Our findings show that only 12 countries in Africa have fully established NPHIs. There is recognition that some of the smaller countries may establish collaborative networks in a region to have the national functions of a public health institute fulfilled. The gaps in responding to building surveillance capacity post COVID-19 is a core function of system strengthening and contributes to global health security. The African CDC, Member States, and partners will need to work intensely to advance NPHIs and to tap into existing resources of the established NPHIs on the continent for advocacy and peer support.
Declarations
Ethics approval and consent to participate
Ethical approval to conduct the survey was obtained from the Public Health Institutes and Research Division of the African CDC. Informed consent was obtained from the study participants, and all completed the online survey.
Consent for publication
Our manuscript does not include information or images that could lead to the identification of a study participant; therefore, consent for publication is not applicable.
Availability of data and Materials
The datasets generated and/or analysed during the current study are available from the corresponding author based on reasonable requests. Countries need to give their consent to make the data publicly available.
Competing interests
The authors declare that they have no competing interests.
Funding
We declare that we have not obtained any funding to conduct this study.
Authors' Contributions
H.T. Designed and planned the study, took the lead in analyzing the results and writing the manuscript. R. T. contributed to the design and implementation of the study, the analysis of the results and the writing of the manuscript. N.M. & A. contributed to the writing of the manuscript. All authors provided critical feedback and helped shape the manuscript.
Acknowledgements
My very great appreciation goes to all Directors and Focal persons of NPHIs in Africa for their participation in the survey and sharing data regarding their NPHI development status with the African CDC.
I would like to thank Mr Adam Terefe for his contribution during the design of the survey questionnaire.
I would also like to express my very great appreciation to Ms Farha Abdalla, Ms Addis Miraf, Dr Amadu CISSE, and Dr Marguerite Loembe and Mr Denis Phocus Bunyoga for sharing the survey questionnaire with NPHI Directors and Focal persons in their Respective Regional Collaborating Centers and for making follow up to get responses.
My appreciation also extends to Dr Shelly Bratton and Dr Carrie Carnevale for their contribution during the write up of the manuscript.
Authors' information
Haftom Taame Desta
Principal Technical Officer for NPHIs,
Africa Centers for Disease Control and Prevention (Africa CDC), African Union Commission,
Email: haftomt@africa-union.org
Natalie Mayet
Deputy Director, National Institute for Communicable Diseases (NICD), South Africa
Email: nataliem@nicd.ac.za
Alex Riolexus Ario
President, International Association of National Public Health Institutes -Africa region (IANPHI)
Email: riolexus@gmail.com
Raji Tajudeen,
Head, Public Health Institutes and Research,
Africa Centers for Disease Control and Prevention (Africa CDC), African Union Commission,
Email: Rtajudeen@africa-union.org
References
- Africa Union.Africa Centres for Disease Control and Prevention. Framework for development of national public health institutes in Africa (2022).
- Binder S, Adigun L, Dusenbury C, et al. National Public Health Institutes: contributing to the public good. J Public Health Policy 29 (2008): 3-21.
- Ellen W, Katherine S, Jessica B, et al. IANPHI and National Public Health Institutes.oboin Public Health (2020)
- Sonja L Myhre, Steve D. French & Anne Bergh(2022).National public health institutes: A scoping review, Global Public Health17 (2022): 1055-1072.
- Koplan JP, Puska P, Jousilahti P, et al. Improving the world's health through national public health institutes. Bull World Health Organ 83 (2005): 154-7.
- Frieden TR, Koplan JP. Stronger national public health institutes for global health. Lancet (London, England) 376 (2010): 1721-1722.
- Myhre S, Habtemariam MK, Heymann DL.et al.Bridging global health actors and agendas: the role of national public health institutes.J Public Health Pol(2022).
- Clemente J, Rhee S, Miller B, et al. Reading between the lines: A qualitative case study of national public health institute functions and attributes in the Joint External Evaluation. J Public Health Afr 11 (2020): 1329.
- Erondu NA, Rahman-Shepherd A, Khan MS, et al. Improving National Intelligence for Public Health Preparedness: a methodological approach to finding local multi-sector indicators for health security. BMJ Glob Health 6 (2021): e004227.
- Johns Hopkins Center for Health Security. Global Health Security Index (2022).
- Adigun L, Dusenbury C, Schoub BD. Public health in Africa-the role of national public health institutes. S Afr Med J 97 (2007): 1036-9.
- International Association of National Public Health Institutes. STAGED DEVELOPMENT TOOL (SDT) FOR NATIONAL PUBLIC HEALTH INSTITUTES (2022)
- Africa Union.Africa Centres for Disease Control and Prevention. Providing a Legal Framework for a National Public Health Institute (NPHI) (2022).
- Saqif Mustafa and Sohel Saikat. “The Role of Public Health Institutes and WHO CCs in health system strengthening and essential public health functions in Africa” (2015): 22.
- National Institute for Communicable Diseases (2022).
- Kenya Medical Research Institute (2022).
- Pasteur Network. Center Pasteur in Cameroon (2022).
- Centers for Disease Control and Prevention. Our History-Our Story (2022).