Retrospective evaluation of the impact of second-stage labor arrest on stress urine incontinence in postpartum women
Article Information
Georges Yared MD1,2, Jihad Al Hassan3,4,5, Charlotte Hajjar5,6, Kariman Ghazal MD5,6,7,*
1Associate Professor Obstetrics and Gynecology Department, American Lebanese University,Beirut, Lebanon
2Head of Obstetrics and Gynecology Department,Rafik Hariri Hospital University Medical Center, Beirut, Lebanon
3Head and Assistant Professor of Obstetrics and Gynaecology Department, Lebanese University, Beirut, Lebanon
4Head of Obstetrics and Gynaecology Department, Al Zahraa Hospital University Medical Centre, Beirut, Lebanon
5Obstetrics and Gynecology Department,Rafik Hariri Hospital University Medical Center, Beirut, Lebanon
6Obstetrics and Gynaecology Department, Al Zahraa Hospital University Medical Centre, Beirut, Lebanon
7Assistant Professor of Obstetrics and Gynaecology Department, Lebanese University, Beirut, Lebanon
*Corresponding Author: Kariman Ghazal, MD, Obstetrics and Gynaecology Department Lebanese University.
Received: 27 September 2022; Accepted: 04 October 2022; Published: 22 October 2022
Citation:
Georges Yared, Jihad Al Hassan, Charlotte Hajjar, Kariman Ghazal. Retrospective evaluation of the impact of second-stage labor arrest on stress urine incontinence in postpartum women. Obstetrics and Gynecology Research 5 (2022): 254-260.
Share at FacebookAbstract
Background: Stress Urinary Incontinence (SUI), has been always linked to normal vaginal delivery (NVD) or operative vaginal delivery (OVD). Many women get concerned about this issue before giving birth and tend to deliver by cesarean delivery. However, the increased frequency of cesarean deliveries poses health concerns especially in the absence of solid risk factors.
Methods: This is a retrospective observational cohort study conducted at Rafic Hariri University Hospital (RHUH) between 2011 and 2013. Forty primiparous women undergoing cesarean delivery were involved. They were evenly divided into 2 groups. The first involved those who underwent elective cesarean delivery and those with failure to progress. The second group involved women who underwent cesarean delivery for arrested second stage of labor. Statistical analysis was performed using the statistical program SPSS version 20.
Results: The prevalence of SUI in group 1 was 25% compared to 35% in group 2. Cesarean delivery was not found to have any protective role against SUI in group 1 patients and the frequency of SUI in selective cesarean patients was nearly the same as those performing cesarean for failure to progress. However, patients undergoing cesarean for arrested second stage of labor > 2hours had a significant higher frequency of SUI as compared to patients undergoing cesarean delivery for arrested second stage of labor < 2hours.
Conclusion: Cesarean delivery cannot be proposed to women who fear to suffer from SUI post-partum. However, it should be done if the cervix fully dilated for > 2hours in order to decrease the risk of SUI.
Keywords
Stress Urinary Incontinence normal delivery cesarien
Stress Urinary articles Stress Urinary Research articles Stress Urinary review articles Stress Urinary PubMed articles Stress Urinary PubMed Central articles Stress Urinary 2023 articles Stress Urinary 2024 articles Stress Urinary Scopus articles Stress Urinary impact factor journals Stress Urinary Scopus journals Stress Urinary PubMed journals Stress Urinary medical journals Stress Urinary free journals Stress Urinary best journals Stress Urinary top journals Stress Urinary free medical journals Stress Urinary famous journals Stress Urinary Google Scholar indexed journals Urinary Incontinence articles Urinary Incontinence Research articles Urinary Incontinence review articles Urinary Incontinence PubMed articles Urinary Incontinence PubMed Central articles Urinary Incontinence 2023 articles Urinary Incontinence 2024 articles Urinary Incontinence Scopus articles Urinary Incontinence impact factor journals Urinary Incontinence Scopus journals Urinary Incontinence PubMed journals Urinary Incontinence medical journals Urinary Incontinence free journals Urinary Incontinence best journals Urinary Incontinence top journals Urinary Incontinence free medical journals Urinary Incontinence famous journals Urinary Incontinence Google Scholar indexed journals normal delivery articles normal delivery Research articles normal delivery review articles normal delivery PubMed articles normal delivery PubMed Central articles normal delivery 2023 articles normal delivery 2024 articles normal delivery Scopus articles normal delivery impact factor journals normal delivery Scopus journals normal delivery PubMed journals normal delivery medical journals normal delivery free journals normal delivery best journals normal delivery top journals normal delivery free medical journals normal delivery famous journals normal delivery Google Scholar indexed journals cesarien articles cesarien Research articles cesarien review articles cesarien PubMed articles cesarien PubMed Central articles cesarien 2023 articles cesarien 2024 articles cesarien Scopus articles cesarien impact factor journals cesarien Scopus journals cesarien PubMed journals cesarien medical journals cesarien free journals cesarien best journals cesarien top journals cesarien free medical journals cesarien famous journals cesarien Google Scholar indexed journals Stress urine incontinence articles Stress urine incontinence Research articles Stress urine incontinence review articles Stress urine incontinence PubMed articles Stress urine incontinence PubMed Central articles Stress urine incontinence 2023 articles Stress urine incontinence 2024 articles Stress urine incontinence Scopus articles Stress urine incontinence impact factor journals Stress urine incontinence Scopus journals Stress urine incontinence PubMed journals Stress urine incontinence medical journals Stress urine incontinence free journals Stress urine incontinence best journals Stress urine incontinence top journals Stress urine incontinence free medical journals Stress urine incontinence famous journals Stress urine incontinence Google Scholar indexed journals physical health articles physical health Research articles physical health review articles physical health PubMed articles physical health PubMed Central articles physical health 2023 articles physical health 2024 articles physical health Scopus articles physical health impact factor journals physical health Scopus journals physical health PubMed journals physical health medical journals physical health free journals physical health best journals physical health top journals physical health free medical journals physical health famous journals physical health Google Scholar indexed journals vaginal delivery articles vaginal delivery Research articles vaginal delivery review articles vaginal delivery PubMed articles vaginal delivery PubMed Central articles vaginal delivery 2023 articles vaginal delivery 2024 articles vaginal delivery Scopus articles vaginal delivery impact factor journals vaginal delivery Scopus journals vaginal delivery PubMed journals vaginal delivery medical journals vaginal delivery free journals vaginal delivery best journals vaginal delivery top journals vaginal delivery free medical journals vaginal delivery famous journals vaginal delivery Google Scholar indexed journals urethra articles urethra Research articles urethra review articles urethra PubMed articles urethra PubMed Central articles urethra 2023 articles urethra 2024 articles urethra Scopus articles urethra impact factor journals urethra Scopus journals urethra PubMed journals urethra medical journals urethra free journals urethra best journals urethra top journals urethra free medical journals urethra famous journals urethra Google Scholar indexed journals bladder neck articles bladder neck Research articles bladder neck review articles bladder neck PubMed articles bladder neck PubMed Central articles bladder neck 2023 articles bladder neck 2024 articles bladder neck Scopus articles bladder neck impact factor journals bladder neck Scopus journals bladder neck PubMed journals bladder neck medical journals bladder neck free journals bladder neck best journals bladder neck top journals bladder neck free medical journals bladder neck famous journals bladder neck Google Scholar indexed journals anterior vaginal wall articles anterior vaginal wall Research articles anterior vaginal wall review articles anterior vaginal wall PubMed articles anterior vaginal wall PubMed Central articles anterior vaginal wall 2023 articles anterior vaginal wall 2024 articles anterior vaginal wall Scopus articles anterior vaginal wall impact factor journals anterior vaginal wall Scopus journals anterior vaginal wall PubMed journals anterior vaginal wall medical journals anterior vaginal wall free journals anterior vaginal wall best journals anterior vaginal wall top journals anterior vaginal wall free medical journals anterior vaginal wall famous journals anterior vaginal wall Google Scholar indexed journals
Article Details
Introduction:
Stress urine incontinence is seen as a serious issue and a serious health concern that can harm both mental and physical health. Limited physical activity and absenteeism have been linked to it, increasing the economic and financial burden on the community. Stress urine incontinence has traditionally been linked to vaginal birth. The continence mechanism seems to be most affected by the first vaginal delivery. It is widely established that parity may also have an impact on the pelvic floor, causing connective tissue and muscle disturbance and a rise in the prevalence of stress incontinence [13].
The pelvic visceral organs are supported by the pelvic floor muscles, especially the levator ani muscles, which are also crucial for maintaining urine continence [3]. These muscles can quickly contract to maintain continence during an acute intraabdominal pressure and then release after evacuation [4]. Physically, the absence of support for the urethra and bladder neck from the pelvic floor muscles and vaginal connective tissue results in urethral hypermobility. As a result, the urethra and bladder neck won't be able to close against the anterior vaginal wall [5].
The urethra may lose mechanical support as a result of trauma to the pelvic floor muscles and nerve damage during childbirth. It is yet unknown what biological processes cause injury to the pelvic floor during pregnancy and childbirth [6]. Pudendal nerve damage, which is typically brought on by surgical vaginal birth Among the explanations put up include OVD, a prolonged second stage of labor, and large birth weight [7]. According to some hypotheses, NVD regular vaginal birth and a drawn-out second stage of labor can harm the levator ani and coccygeus muscles [8]. For instance, alterations in collagen and elastin may play a part in the pathophysiology of SUI [9].
Between 15% and 55% of persons experience SUI. Pregnancy and childbirth account for 50% of the causes of stress urine incontinence in parous women, particularly premenopausal women; however, in postmenopausal women, age seems to balance out the effect of parity [10]. Risk factors for SUI include obesity [11], non-Hispanic ethnicity, and high-impact sports like jumping.
The prevalence of cesarean births has increased recently despite the creation of obstetric practice guidelines. The protective effects of elective cesarean delivery are being debated by both the medical and lay sectors.
Objective
It is important to understand whether failure to advance and a paused second stage of labor lasting longer than two hours are risk factors for SUI, as well as when the pregnancy was terminated by cesarean birth. In addition, the proportion of patients with an arrested second stage of labor who underwent a cesarean section in under two hours compared to those who underwent a cesarean section in excess of two hours.
Aim:
The primary objective of our study is to emphasize the value of C|S and NVD in identifying SUI during pregnancy.
Materials
40 primigravida women who needed cesarean deliveries between 2011 and 2013 were the subject of a retrospective cohort observational study at Rafic Hariri University Hospital. The participants were equally divided into two groups.
- a) Women who elect to have cesarean births or who experience complications
- b) Women who have cesarean sections because their second stage of labor has been halted.
Inclusion criteria:
Term cesarean deliveries by primiparous women between the ages of 18 and 30
Exclusion criteria:
- Women who become pregnant within the first two years of having a cesarean section are excluded from the study.
- We were unable to reach the women.
- Ladies who experienced incontinence while pregnant or before having their first cesarean section.
- Ladies who have had pelvic surgery before (ex dilation and curettage, myomectomy)
- Estimated fetal weight > 5 kg for mothers who are not diabetic, > 4.5 kg for women who are, and 2 kg.
- Epidural sedation.
METHODS
Data Collection:
After a two-year follow-up period, 40 primigravida women were contacted by phone, and only those who met the inclusion requirements were chosen. We gained oral consent prior to the study's commencement by outlining its objectives. A validated questionnaire was then given to the patients to complete. Tables with the data were created. The obstetric history of participants was gathered from the hospital's medical records after receiving IRB approval from RHUH.
Data analysis:
Retrospective data collection was done on 40 patients who met the aforementioned inclusion and exclusion criteria. A licensed statistician carried out the statistical analysis. He made use of SPSS version 20 for statistics. Categorical variables were subjected to the Chi-Square Square test. A p-value of less than 5% indicates the existence of a statistically significant relationship.
Results
We were able to review the medical records of primigravida women who underwent cesarean delivery between 2011 and 2013 after receiving permission from the RHUH Institutional Review Board.
121 ladies who fit the inclusion requirements were recruited. 37 of these 121 were dropped because their medical records didn't meet certain requirements (for example baby weight, exact delay in second stage of labor, and accurate measurement of cervical dilation). 84 women were left, 72 of whom qualified for group 1 (elective cesarean or cesarean for failure to progress), and 12 qualified for group 2. (cesarean for arrested second stage of labor).
Until we hit our target of 20 women responding, we randomly began contacting each of these 72 women and completed the survey. 34 people were contacted in all. Home relocation and phone number changes were the main causes of the lack of a response.
Table 1 shows prevalence of SUI in group 1 patients along other variables whose ratio of correlation with SUI incidence was calculated.
The prevalence of SUI was 5/20 (25%). Out of these 5 patients with SUI one of them has underwent elective cesarean while the others have underwent cesarean for failure to progress.
When age was studied as a potential risk factor, the correlation ratio was r=0.164. As such, age is a weak risk factor for SUI. Similarly, baby weight and gestational period were found to have r=0.088 and r=0.57 respectively which proves baby weight is a very weak risk factor while gestational age is a moderate risk factor.
As a conclusion, age and baby weight cannot be considered as risk factors for SUI, but increase in gestational age is associated with increased occurrence of SUI.
Table 1: SUI frequecy in women in patients performing c-section post failure to progress or elective c-section
|
Patient |
Age |
Gestation |
Cervical dilation |
Baby weight |
SUI |
|
1 |
19 |
40 |
elective |
2.5 |
yes |
|
2 |
21 |
36+4 |
4cm for 7hr |
3.9 |
yes |
|
3 |
30 |
36+5 |
4cm for 6hr |
4.2 |
yes |
|
4 |
29 |
38+2 |
1cm for 12hr |
2.7 |
yes |
|
5 |
29 |
38+5 |
2cm for 10hr |
2.9 |
yes |
|
6 |
18 |
40+4 |
1.5cm for 4hr |
3.2 |
No |
|
7 |
18 |
40+1 |
1cm for 5hr |
3.7 |
No |
|
8 |
18 |
42 |
4cm for 4hr |
3.7 |
No |
|
9 |
19 |
39+6 |
3cm for 5hr |
2.4 |
no |
|
10 |
19 |
39 |
1cm for 5hr |
3.2 |
no |
|
11 |
20 |
37+1 |
elective |
3 |
No |
|
12 |
21 |
40+3 |
4cm for 6hr |
3 |
no |
|
13 |
24 |
40+3 |
4cm for 4hr |
3.3 |
No |
|
14 |
25 |
40+4 |
elective |
4 |
No |
|
15 |
25 |
40 |
2cm for 5hr |
4.2 |
No |
|
16 |
26 |
37+4 |
elective |
2.8 |
No |
|
17 |
27 |
40+2 |
elective |
3.2 |
No |
|
18 |
27 |
39+4 |
3cm for 5hr |
3.3 |
No |
|
19 |
28 |
38+4 |
Elective |
2.9 |
No |
|
20 |
28 |
40+4 |
4cm for 9hr |
3.2 |
No |
Table 2: SUI frequency in women performing c-section for arrested 2nd stage of l
|
Patient |
Age |
Gestation |
Baby weight |
Indication for C-section |
SUI |
|
1 |
18 |
40+2 |
3.9 |
4hr |
yes |
|
2 |
19 |
40+4 |
2.8 |
4hr |
yes |
|
3 |
21 |
41+3 |
4 |
2hr |
yes |
|
4 |
24 |
38+4 |
2.9 |
4hr |
yes |
|
5 |
29 |
40+2 |
3.9 |
2.5hr |
yes |
|
6 |
30 |
36+2 |
2 |
3hr |
yes |
|
7 |
30 |
39+3 |
3.6 |
4hr |
yes |
|
8 |
18 |
40+3 |
3.5 |
3hr |
no |
|
9 |
18 |
42+2 |
3.8 |
2hr |
no |
|
10 |
19 |
40+5 |
3.2 |
2hr |
no |
|
11 |
21 |
39+2 |
3.2 |
2.5 |
no |
|
12 |
22 |
40+1 |
3.9 |
2hr |
no |
|
13 |
23 |
39+3 |
3.1 |
2hr |
no |
|
14 |
24 |
40+4 |
2.9 |
2.5hr |
no |
|
15 |
25 |
40+2 |
2.7 |
2hr |
no |
|
16 |
26 |
40+3 |
2.5 |
1hr |
no |
|
17 |
26 |
40+4 |
3 |
3hr |
no |
|
18 |
27 |
40+1 |
3.5 |
1.5hr |
no |
|
19 |
30 |
40 |
3 |
3hr |
no |
|
20 |
30 |
36+6 |
3.2 |
2hr |
no |
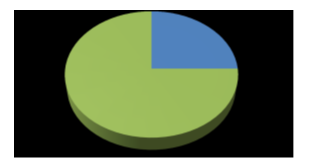
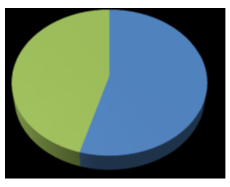
YES 25%, NO 75%
Fig. 1: Pie chart illustrating frequency of SUI in Group 1 patients.
Yes: presence of SUI, No: absence of SUI
This is a pie chart showing frequency of SUI in group 1 of 25% (n=5). It does not take into consideration the cause of cesarean delivery whether failure to progress or upon maternal request. We compared frequency of SUI in patients of group 1 undergoing cesarean delivery for failure to progress (n=14) to the frequency of SUI in all patients of group 1 (n=20). The goal of this comparison is to know if elective cesarean delivery had any protective role as compared to failure to progress and if failure to progress by itself is a risk factor for SUI. P value was also calculated.
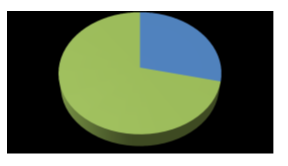
YES 29%, NO 71%
Fig. 2: Frequency of SUI in non-elective cesareans of Group 1 (4/14)
YES: presence of SUI in women undergoing cesarean delivery for failure to progress (4/14)
NO: absence of SUI in women undergoing cesarean for failure to progress (10/14)
We found that the frequency of SUI increased from 25% to 29%.
P value=0.5976
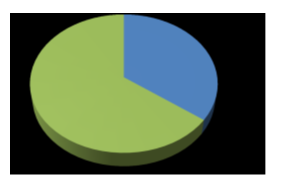
YES 35%, NO 65%
Fig. 3: pie chart illustrating frequency of SUI in Group 2
YES: presence of SUI. NO: absence of SUI
This is a pie chart showing frequency of SUI in group 2 of 35% (n=7).
The frequency of SUI in group 2 is higher by 10% than group 1.
group 2 was divided into 2 subgroups. Group a included patient who underwent cesarean within 2 hours of pushing post full dilation of the cervix. Group b included patients who underwent cesarean after 2 hours of pushing post full dilation of the cervix. Similarly, the frequency of SUI in both subgroups was calculated and p value was obtained
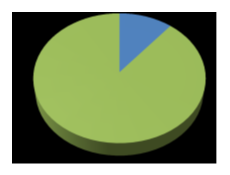
YES 11% NO 89%
Fig. 4: Frequency of SUI in subgroup A (1/9)
YES: presence of SUI in women with arrested 2nd stage of labor for less than or equal to 2 hours.
NO: absence of SUI in women with arrested 2nd stage of labor for less than or equal to 2 hours.
Out of 9 patients having arrested second stage of labor for less than or equal to 2 hours only 1 patient had SUI.
YES (54%), NO 46%
Fig. 5: Frequency of SUI in subgroup B (6/11)
YES: presence of SUI in patients with arrested second stage of labor for more than 2 hours
NO: absence of SUI in patients with arrested second stage of labor for more than 2 hours
Out of 11 patients having arrested second stage of labor for more than 2 hours, 6 of them had SUI (54%)
P value=0.01803
DISCUSSION
To summarize, in our retrospective cohort study 40 primiparous women undergoing cesarean delivery were recruited and divided equally into 2 subgroups. The 1st group included those undergoing cesarean delivery either electively or for failure to achieve full cervical dilation. The 2nd group included those undergoing cesarean delivery for failure of baby descent despite full cervical dilation. The frequency of SUI was 25% in group 1 and 35% in group 2. Other risk factors like maternal age, gestational age and baby weight were also studied to see if they are potential risk factors. They all proved to have weak correlation with the occurrence of SUI in both groups. Thus, the difference in frequency is insignificant. This means group 1 containing elective cesareans and cesareans for failure to progress, is statistically homogeneous. Hence, elective cesarean has no protective role against SUI as compared to cesarean for failure to progress. In addition, failure to progress is not a risk factor for SUI as well.
These findings agree with Hung-yen Chin et al and Thorp et al concerning the non-protective role of elective cesarean delivery [16, 17]. According to them maternal age (>30), smoking, and a high BMI before pregnancy are indicators of developing postpartum urine incontinence. However, this does not rule out the possibility of postpartum stress urine incontinence in women who are older at the time of delivery. Because pregnancy has been demonstrated to enhance the prevalence of stress incontinence relative to nulliparous women [18], a cesarean cannot provide total protection against postpartum stress urine incontinence [17]. There was no statistical difference between vaginal and C-sections performed for obstetric reasons.
In comparison to elective cesareans, they discovered that cesareans performed for protracted and halted labor were associated with a greater incidence of postpartum stress incontinence. Another thing to consider is if the push power plays a role in the style of birth, itself, be a risk factor for future stress incontinence.
According to Gartland et al.2012, cesarean sections performed before labor and before the onset of the second stage of labor were associated with lower rates of stress incontinence than spontaneous vaginal delivery, whereas cesarean sections performed after the second stage of labor were associated with a lower likelihood of reporting to prevent one of them from developing postpartum stress urinary stress incontinence, however there was no statistical difference between vaginal and cesarean birth [19].On the other hand, cesarean delivery was found to have a protective role when performed within the 1st 2 hours of full cervical dilation.
Similar results were found by Sultan et al When compared to the elective cesarean group, they found that women who underwent a cesarean after the commencement of labor were more likely to acquire pudendal nerve injury [20, 21]. He stated that pudendal nerve injury occurred mostly on the left side, with NVD and labor being the main risk factors. As a result, he advocated that cesarean births be done on a voluntary basis if the goal was to reduce the risk of SUI.
This was not the case with Donath et al. who found out that there is a minimal increase in the incidence of incontinence when duration of the second stage extends from 0 to 5 hours, but without having any major statistical difference [22].
When compared to vaginal delivery, Farrell et al. discovered that cesarean delivery at any stage of labor has a lower risk of developing SUI. As a result, the timing of a C-section during labor and delivery appears to be a significant modifiable risk factor for postpartum stress urine incontinence.
Nevertheless, Gimosky et al. concluded that prolonged second stage of labor beyond current guidelines decreased the incidence of cesarean delivery by 55% and did not have negative impact on maternal and neonatal risks [23].
So, how long should women be allowed to push before opting for caesarean section?
According to him delaying surgery beyond current guidelines in situations of extended second-stage labor, reduced the incidence of c - section by 55%. It had a deleterious impact on women, though. Postpartum hemorrhage, chorioamnionitis, and third and fourth-degree degree perineal lacerations were among the conditions. When the second stage in this process is prolonged, Sandstorm et al. 2016 found an increased relative risk of having many infant problems (ischemic hypoxic encephalopathy, meconium aspiration syndrome, seizures, and NICU admissions) [24] He, argued that in order to protect neonates, current standards for performing a timed cesarean birth in women with a long second stage of labor must be followed. we stated that we want to find out if frequency of SUI increases with increasing time post full cervical dilation The effect on babies, on the other hand, was limited.
One of the main limitations was that most if not all of our patients belonged to low socioeconomic status and all of them were of Syrian nationality with low educational background ,were refugees this made it difficult to contact them due to frequent house translocation and change in phone number. and the meaning of the questions in the questionnaire was hard to convey. This fact prevented us from scaling the severity of SUI in these patients and limited us with “yes or no” answers.
Several studies like sultan et al [24] relied on objective tests to assess SUI in addition to standardized questionnaires. These tests included pudendal nerve motor terminal latency test, cough stress test and cotton swab test. They were performed at regular intervals post-delivery. We were not able to conduct such tests due to lack of means and experience in addition to high possibility of loss of follow up throughout the study.
Conclusions
Stress Urinary incontinence (SUI) is a common clinical condition worldwide that affects women of all ages and across different cultures and races. It is associated with debilitating impact on quality of life and in certain cases can increase the risk of depression when it becomes so severe.. However, it is important to know if failure to achieve a full dilation during the first stage of labor, and the inability of the baby to descent through the birth canal during the second stage of labor, could be considered as major risk factors for the development of post-partum SUI if pregnancy was terminated by cesarean delivery.
Nevertheless, the fact that some studies proved opposite results while others confirmed our findings poses the challenge to conduct further studies with minimized bias and larger samples in order to build solid conclusions concerning this major health problem.
References
- Christopher M. Tarnay, M D. Urinary Incontinence & Pelvic Floor Disorders . In: Andrei Rebarber, MDAlan H. DeCherney, Lauren Nathan, Neri Laufer, Ashley S. Roman .CURRENT Diagnosis & Treatment: Obstetrics & Gynecology, 11e, New york :McGraw-Hill Companies; chapter 42, 2007.
- Luo R, Dai W, Tay L H, et al., Urinary incontinence in female outpatients in Singapore, Int Urogynecol J,28 (2017): 1-6
- Blueprints-Obstetrics-and-Gynecology-Blueprint-Series-P826.aspx
- Anne M Gilroy, Brian R MacPherson, Lawrence M Ross, et al.,, Atlas of Anatomy, 2nd edition, Thieme, 2012.
- Rahn D D, Wai C Y, Hoffman B L, et al., Urinary incontinence. In: William Gynecology, McGraw Hill Medical, New York p.609, 2012.
- Groutz A, Rimon E, Peled S, et al., Cesarean section: does it really prevent the development of postpartum stress urinary incontinence? A prospective study of 363 women one year after their first delivery. Neurourol Urodyn. 23 (1) (2004): 2-6.
- Snooks S J, Swash M, Henry M M, Setchell M. Risk factors in childbirth causing damage to the pelvic floor innervations. Int J Colorectal Dis. 1 (1) (1986): 20-24.
- Shek K L, Dietz H P. Intrapartum risk factors for levator trauma BJOG.117 (12) (2010): 1485-1492.
- Chen B, Wen Y, Zhang Z, et al., Microarray analysis of differentially expressed genes in vaginal tissues from women with stress urinary incontinence compared with asymptomatic women. Hum Reprod. 21(1) (2006): 22-29.
- Nygaard I.Urinary incontinence: is cesarean delivery protective? Semin Perinatol. 30 (5) (2006): 267-271.
- Subak L L, Richter H E, Hunskaar S. Obesity and urinary incontinence: epidemiology and clinical research update. J Urol. 182 (6 Suppl) (2009): 2-7.
- Lukacz E S, Lawrence J M, Contreras R, et al., Parity, mode of delivery, and pelvic floor disorders Obstet Gynecol. 107 (6) (2006): 1253-1260
- Dinç A 1. Prevalence of Urinary Incontinence During Pregnancy and Associated Risk Factors. Low Urin Tract Symptoms. Jul 4, 2017.
- Boyles S H, Li H, Mori T, et al., Effect of mode of delivery on the incidence of urinary incontinence in primiparous women. Obstet Gynecol. 113 (1) (2000): 134-141.
- Leijonhufvud A, Lundholm C, Cnattingius S, et al., Risks of stress urinary incontinence and pelvic organ prolapse surgery in relation to mode of childbirth. Am J Obstet Gynecol. 204 (1) (2011):1-7.
- Chin H Y, Chen M C, Liu Y H, Wang K H. Postpartum urinary incontinence: a comparison of vaginal delivery, elective, and emergent cesarean section. Int Urogynecol J Pelvic Floor Dysfunct. 17 (6) (2006): 631-635.
- Lal.M. Prevention of urinary and anal incontinence: role of elective cesarean delivery. Curr Opin Obstet Gynecol. 15(5) (2003): 439-448.
- Rogers R G, Ninivaggio C, Gallagher K, et al., Pelvic floor symptoms and quality of life changes during first pregnancy: a prospective cohort study. Int Urogynecol J. 28 (11) (2017):1701-1707.
- Brown S J, Gartland D, Donath S, MacArthur C. Effects of prolonged second stage, method of birth, timing of caesarean section and other obstetric risk factors on postnatal urinary incontinence: an Australian nulliparous cohort study. BJOG. 118 (8) (2011): 991-1000.
- Sultan A H, Kamm M A, Hudson C N. Pudendal nerve damage during labour: prospective study before and after childbirth. Br J Obstet Gynaecol. 101(1) (1994):22-28.
- Boyles S H, Li H, Mori T, et al., Effect of mode of delivery on the incidence of urinary incontinence in primiparous women. Obstet Gynecol. 113 (1) (2009): 134-141.
- Brown S J, Gartland D, Donath S, MacArthur C. Effects of prolonged second stage, method of birth, timing of caesarean section and other obstetric risk factors on postnatal urinary incontinence: an Australian nulliparous cohort study. BJOG. 118 (8) (2011): 991-1000.
- Gimovsky AC, Berghella V. Prolonged Second Stage: What Is the Optimal Length? Obstet Gynecol Surv. 71 (11) (2016): 667-674.
- Altman M, Sandström A, Petersson G, Frisell T, Cnattingius S, Stephansson O. Prolonged second stage of labor is associated with low Apgar score. Eur J Epidemiol. 30 (11) (2015): 1209-1215.
