Restorative Direct Management of Cavitated Proximal Carious Lesions of Permanent Molars using Elastic Separators in Children and Adolescents
Article Information
Berdouses ED1*, Agouropoulos A2, Sifakaki M3, Lagouvardos P4, Oulis CJ5
1Paediatric Dentist, Athens, Greece
2Assistant Professor, Department of Paediatric Dentistry, National and Kapodistrian University of Athens, Greece
3Paediatric Dentist, Clinical Instructor, Department of Paediatric Dentistry, National and Kapodistrian University of Athens, Greece
4Professor Emeritus, Department of Operative Dentistry, National and Kapodistrian University of Athens, Greece
5Professor Emeritus, Department of Paediatric Dentistry, National and Kapodistrian University of Athens, Greece
*Corresponding Author: Berdouses Elias, Paediatric Dentist, 22 Kodrou str, Halandri, Athens 152 31, Greece/p>
Received: 02 October 2020; Accepted: 09 October 2020; Published: 28 October 2020
Citation: Berdouses ED, Agouropoulos A, Sifakaki M, Lagouvardos P, Oulis CJ. Restorative Direct Management of Cavitated Proximal Carious Lesions of Permanent Molars using Elastic Separators in Children and Adolescents. Dental Research and Oral Health 3 (2020): 190-201.
Share at FacebookAbstract
Purpose: The purpose of this study was to assess the longevity of direct amalgam and composite restorations placed on the mesial surface of permanent molars after separation with elastic separators.
Design: One hundred and seventy seven (177) restorations placed on the mesial surfaces of first and second permanent molars in 140 patients aged 10-25 years-old (median age 12.2 years) were followed for a period of 1 to 12 years (median time 4.3 years). Eighty four (84) amalgam and 93 composite resin restorations were placed randomly on carious lesions that were detected by bite-wing x-rays at the dentino-enamel junction and verified as cavitated after tooth separation. Restorations were evaluated clinically according to the modified Ryge criteria. Flexible parametric proportional-hazards and proportional-odds models for censored survival data was used to analyze the data, with application to prognostic modelling and estimation of treatment effects at 95% CI.
Results: Of the 177 restorations, 13 (7.2%) failed in a median time to failure of 8.8 years. There was no statistically significant difference on the cumulative median time to failures between amalgam and composite while statistically significant difference was found between patients that were using fluoride mouthrinse or not (p<0.048) and if there was bleeding detected at the interproximal area of the restoration or not (p<0.001).
Conclusions: Restorative management of cavitated proximal carious surfaces of permanent teeth with amalgam or composite resin, using elastic separators, seems to be a very good and promising alternative technique in the context of the minimal invasive dentistry in children and adolescents.
Keywords
Minimal Invasive Dentistry, Interproximal Restorations, Teeth Separation
Minimal Invasive Dentistry articles; Interproximal Restorations articles; Teeth Separation articles
Minimal Invasive Dentistry articles Minimal Invasive Dentistry Research articles Minimal Invasive Dentistry review articles Minimal Invasive Dentistry PubMed articles Minimal Invasive Dentistry PubMed Central articles Minimal Invasive Dentistry 2023 articles Minimal Invasive Dentistry 2024 articles Minimal Invasive Dentistry Scopus articles Minimal Invasive Dentistry impact factor journals Minimal Invasive Dentistry Scopus journals Minimal Invasive Dentistry PubMed journals Minimal Invasive Dentistry medical journals Minimal Invasive Dentistry free journals Minimal Invasive Dentistry best journals Minimal Invasive Dentistry top journals Minimal Invasive Dentistry free medical journals Minimal Invasive Dentistry famous journals Minimal Invasive Dentistry Google Scholar indexed journals Interproximal Restorations articles Interproximal Restorations Research articles Interproximal Restorations review articles Interproximal Restorations PubMed articles Interproximal Restorations PubMed Central articles Interproximal Restorations 2023 articles Interproximal Restorations 2024 articles Interproximal Restorations Scopus articles Interproximal Restorations impact factor journals Interproximal Restorations Scopus journals Interproximal Restorations PubMed journals Interproximal Restorations medical journals Interproximal Restorations free journals Interproximal Restorations best journals Interproximal Restorations top journals Interproximal Restorations free medical journals Interproximal Restorations famous journals Interproximal Restorations Google Scholar indexed journals Teeth Separation articles Teeth Separation Research articles Teeth Separation review articles Teeth Separation PubMed articles Teeth Separation PubMed Central articles Teeth Separation 2023 articles Teeth Separation 2024 articles Teeth Separation Scopus articles Teeth Separation impact factor journals Teeth Separation Scopus journals Teeth Separation PubMed journals Teeth Separation medical journals Teeth Separation free journals Teeth Separation best journals Teeth Separation top journals Teeth Separation free medical journals Teeth Separation famous journals Teeth Separation Google Scholar indexed journals Secondary caries articles Secondary caries Research articles Secondary caries review articles Secondary caries PubMed articles Secondary caries PubMed Central articles Secondary caries 2023 articles Secondary caries 2024 articles Secondary caries Scopus articles Secondary caries impact factor journals Secondary caries Scopus journals Secondary caries PubMed journals Secondary caries medical journals Secondary caries free journals Secondary caries best journals Secondary caries top journals Secondary caries free medical journals Secondary caries famous journals Secondary caries Google Scholar indexed journals molars articles molars Research articles molars review articles molars PubMed articles molars PubMed Central articles molars 2023 articles molars 2024 articles molars Scopus articles molars impact factor journals molars Scopus journals molars PubMed journals molars medical journals molars free journals molars best journals molars top journals molars free medical journals molars famous journals molars Google Scholar indexed journals
Article Details
1.Introduction
Dental caries is still a problem in many industrialized countries and the global burden of the disease is still significant [1]. For many years, dentistry was influenced by the approach “extension for prevention”. This included radical removal of diseased tooth structure, along with material-driven geometric extensions to areas that were assumed to be caries-resistant. Today a different paradigm of operative conservatism, sometimes referred to as “minimally invasive dentistry,” has gained popularity. It is designed to promote maximum preservation of healthy dental structures over a lifetime [2]. Proximal caries of the first permanent molar account for a significant proportion of the carious lesions of this tooth and the mesial surface has been reported to be more susceptible to dental caries compared to the rest smooth surfaces [3-5]. Early diagnosis can prevent incipient lesions form evolving to the cavitation level. Radiographic examination is the most frequently used diagnostic method for the detection of interproximal lesions [6]. The limitation of the radiographs is that they have low accuracy in the detection of incipient carious lesions and cannot distinguish between cavitated/non-cavitated surfaces [7]. The management of the proximal cavitated carious lesions in permanent molars has been a challenge for the clinician in terms of integrity of the tooth, aesthetics and longevity of the restoration. The survival rate of posterior restorations that include interproximal surfaces, range from 92.5% to 92.8 % for amalgam and 86.2% to 85.8% for composite resins [8, 9]. Main reasons of failure are secondary caries and fractures of the restorations and/or the tooth. Secondary caries have been found significantly higher in composite restorations [8-10].
Minimal invasive techniques for restoration of proximal carious lesions are the tunnel and the saucer shaped (only box) techniques [2, 11-13] introduced in an attempt to preserve sound tooth structure and overcome the problem of durability of the restoration. Results regarding the failure rates of these types of restorations show that they present inferior longevity compared to conventional class II composite resin restorations. Main reasons of failure are marginal ridge fracture for the tunnel and recurrent or progressive caries for both configurations [11, 14]. Temporary separation of the teeth with orthodontic elastic separators gives direct visual access to the proximal tooth surface and answers the question “cavitation or not”. At the same time, the method gives the possibility for a direct restoration of the cavitated carious lesion [15]. In light of minimal-invasive dentistry, this new approach promotes a more conservative cavity design [16]. The purpose of this study was to assess the longevity of direct amalgam and composite restorations placed in the mesial surface of first and second permanent molars after separation with elastic bands.
2. Methods and Materials
The sample of this study was selected from the files of children, having one or more proximal carious lesion detected during the visual or radiographic initial examination and restored with the abovementioned method in a private dental clinic in Athens, Greece. One trained and experienced dentist performed all clinical procedures, while a different clinician made the final recall of the patients and did the clinical evaluation of the restoration. Parents or guardians signed the consent form to allow children to participate in the study after they were informed of the benefits of the study to evaluate the performance of this type of restoration. The study was also approved by the Ethics and Research Committee of the National and Kapodistrian University of Athens, School of Health Sciences, Department of Dentistry (Ref. 57a/30.10.2006). The inclusion criteria to perform a direct restoration on a mesial surface of 1st or 2nd permanent molar were: a) to present with proximal caries lesions that was detected visually at the interproximal surface, or b) radiographically the lesion to extend between the outer and middle third of the thickness of the dentin (D1-D2), (Table 1), c) absence of spontaneous pain and d) the restorations had at least 1 year of follow up time. Exclusion criteria: a) broken marginal ridge and visually open cavitation before restoration, b) caries extending into the inner 1/3 of the thickness of the dentin (D3), or in close proximity to the pulp, c) presence of radiographic signs of periapical lesions.
|
Class |
Description |
|
E0 |
No lesion |
|
E1 |
lesion in the outer half of enamel |
|
E2 |
lesion in the inner half of enamel |
|
D1 |
lesion in the outer third of dentin |
|
D2 |
lesion in the middle third of dentin |
|
D3 |
Lesion in the inner third of dentin |
Table 1: Classification of the depth of interproximal caries lesion [27].
2.1 Treatment procedures
The performed technique followed a standard procedure and consisted of stage I:
- Visual detection of a mesial carious lesion which was always followed by a radiographic evaluation or there was only radiographic detection of the lesion. In any case the lesion should not exceed radiographically the middle 1/3 of dentin,
- A double thickness elastic separator (DynaFlex® Reseps separators, DynaFlex, Missouri, USA) was inserted between the contacting surfaces of the affected and the adjacent tooth with the use of the appropriate forceps, for 4-5 days. It was reminded to the patient the possibility of temporary discomfort and guidance of proper hygiene was given.
- Schedule the second visit after 4 to 6 days
At the second appointment stage II was performed:
- Removal of the elastic separator and a 2-3 mm interproximal space was usually observed
- Assessment of the surface of the lesion visually to determine if it was a cavitated or not and if the created space was adequate to facilitate direct restoration of the mesial surface
- Local anaesthesia was performed and rubber dam was placed
- Use of a #330 carbide bur in a horizontal direction buccolingually to remove caries. Further caries removal was performed by a slow speed hand piece and a small round bur
- Provided that the thickness of the remaining marginal ridge was at least 2 mm, a direct restoration was placed using amalgam or composite resin. Otherwise, a class II restoration was performed.
All restorations in this clinical study were performed by a single trained and experienced dentist and all materials were handled according to the manufacturer recommendations. Amalgam restorations were performed using Dispersalloy® (Dentsply, USA). The material was condensed in the cavity using a thin amalgam condenser and the help of the gutta-percha instrument. Composite resin restorations were performed using Spectum® (Dentsply, USA). The cavity was treated with 37% phosphoric acid etch, Eco-Etch (Ivoclar-Vivadent, Liechtenstein) for 30’ sec and then rinsed thoroughly at least for 10 sec. A layer of Prime & Bond NT® (Dentsply, USA) was applied with a disposable brush for 20 seconds. Then the surface was gently air dried for at least 5 seconds so the surface had a glossy uniform appearance. Then the Prime & Bond NT® was light cured for 20 sec and the composite material was placed in one layer and light cured for 40 seconds. The patient’s records were also used to extract information on previous caries experience. Based on the previous caries experience patients were classified as high or low caries risk (low risk dmft or DMFT 0 or 1 and high risk dmft or DMFT >1).
2.2 Outcome evaluation
Primary outcome was failure of the restoration because of the development of secondary caries. Secondary outcome was broken marginal ridge. The restorations were evaluated at the recalls of the patients. All patients, even patients that the restorations were marked as failed at a previous recall, had the final examination performed by a second experienced paediatric dentist. During this examination the patients were asked to provide information on tooth brushing frequency, daily fluoride use and use of floss.
Based on the frequency of the recall examinations patients were classified in 3 groups: patients that had recalls every 6 months, once a year or occasionally. Patients were divided into 3 groups based on the reason causing their visit: pain, need for restoration or check up/prevention. Patient were also identified as using daily fluoride mouth rinse or not while they were divided in 3 groups based on the use of floss: daily, sporadically or not at all. The restorations were evaluated from 1-12 years clinically as successful or failed according to the modified Ryge criteria [17].
2.3 Statistical analysis
Descriptive statistics are given by absolute (N) and relative (%) frequencies for categorical variables and median and Interquartile Range (IQR) for continuous ones. Flexible parametric proportional-hazards and proportional-odds models for censored survival data were used to analyze the data, with application to prognostic modelling and estimation of treatment effects at 95% CI. Time-to-failure analyses took into account the uncertainty regarding the exact time of failure. When failure had not occurred at the recall date, time to failure has been considered as right censored as in the usual survival analysis case. When failure had occurred at the recall date, time of failure has been considered as lying in an interval between a prior date and the recall date.
More specifically the prior date was considered to be one year before the recall date for those with yearly visits and 3 months after placement date for those with sporadic visits. All estimates and tests have been based on flexible parametric proportional hazards models allowing for interval censored data. Clustering of restorations within patients has been ignored since it does not affect mean estimates and its effect on standard errors was negligible [18, 19]. Statistical analysis was performed using the software STATA 12 (Stata Corp LLC, Texas, USA).
3. Results
One hundred and seventy seven restorations (177) were included in the sample from 139 patients. Eighty four (84) were amalgam and 93 were composite restorations (Table 2). The range of the age of the sample was between 10 and 15 years-old (median age 12.4 years) while the follow up period extended from 1 to 12 years (median time 4.3 years). There were two reasons for a restoration to fail, one was secondary caries and the other was marginal ridge failure. Most of the times both reasons were observed (10 restorations) without being possible to identify which one was the primary cause of the failure. There was one case where only caries were observed and 2 cases where only marginal ridge failure was detected. Overall, out of the 177 restorations 11 (6.2%) developed caries during the period of study and 12 (6.8%) had marginal ridge fracture while the total number of failures were 13 restorations (7.3%). The median age of the placement of the restorations was 12.4 years and the time lapsed until the failure either because of caries or because of marginal ridge failure was 8.9 years (Table 2). Figure 1 presents the estimated cumulative probability of failure. The median time to failure was calculated to 20.2 years while the cumulative probability failure at 2, 5 and 10 years was 1.17, 5.75 and 18.20%. Of the different factors that were evaluated on their effect on the failures of the restorations only gum bleeding, frequency of brushing and use of mouthrinse have a statistically significant preventive effect on the restorations. While caries risk group, restorative material, reason and frequency of examinations was not found to have any statistically significant effect (Table 3).
Figure 2 presents the cumulative probability of failure based on the material of the restoration. Both materials show similar performance with estimated median time to failure being 17.8 years for amalgam restorations and 21.7 years for the composite resin ones. While the cumulative probability failure for 5 and 10 years were 6.71%, 4.75% and 21.59%, 15.69% for the amalgam and composite restorations respectively. No statistical difference was found in the performance between the two materials. Similar picture appears in figure 3 where the estimated cumulative probability of failure by dmft experience is presented. There is no statistically significant difference found between the two groups. The estimated median time to failure was 18.0 and 30.0 for the low and high experience group while the cumulative probability failure for 5 and 10 years were 7.72%, 3.36% and 22.72%, 10.37% for the low and high experience group, respectively. In figure 4 is presented the estimated cumulative probability of failure by gum bleeding. The estimated median time to failure was 8.5 and 31.1 years for the bleeding and the no bleeding group while the estimated cumulative probability of failure for 5 and 10 years were 25.90%, 3.73% and 59.41%, 10.81 for the bleeding and the no bleeding group.
|
Study sample |
Patients |
Surfaces |
Amalgam |
Resin |
|
|
139 |
177 |
84 |
93 |
||
|
Total restorations |
Reason for failure |
Total restorat-ions failed |
|||
|
Caries |
Marginal ridge |
||||
|
Sample by surface |
177 |
11 (6.2%) |
12 (6.8%) |
13 (7.3%) |
|
|
Age of placement (years) Median (IQR) |
12.4 (10.7 15.4) |
13.1 (10.3 15.7) |
14.9 (11.8 15.5) |
14.0 (10.3 15.7) |
|
|
Follow Up time (years) Median (IQR) |
4.3 (2.1, 8.4) |
8.9 (8.4, 9.5) |
8.9 (8.4, 9.4) |
8.8 (8.4, 9.4) |
|
|
dmft – Median (IQR) |
1.0 (0.0, 5.0) |
0.0 (0.0, 0.5) |
0.0 (0.0, 1.0) |
0.0 (0.0, 1.0) |
|
|
DMFT - Median (IQR) |
4.0 (2.0, 5.0) |
5.0 (2.5, 8.5) |
4.0 (2.0, 7.0) |
4.0 (2.0, 7.0) |
|
Table 2: Descriptive statistics of the sample.
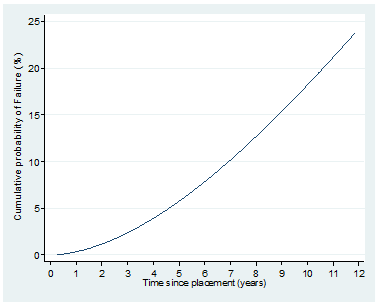
Figure 1: Estimated cumulative probability of Failure.
Estimated (95%CI) median time to Failure: 20.2 (9.9, 41.3) years
Estimated (95%CI) cumulative Failure (%) at 2 years: 1.17 (0.22, 5.99)
Estimated (95%CI) cumulative Failure (%) at 5 years: 5.75 (2.80, 11.61)
Estimated (95%CI) cumulative Failure (%) at 10 years: 18.20 (10.15, 31.41)
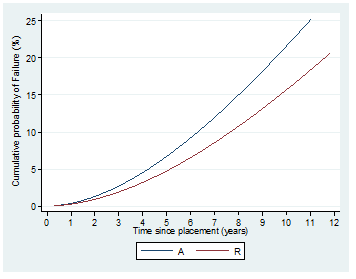
Figure 2: Cumulative probability of failure due to caries based on the material of the restoration.
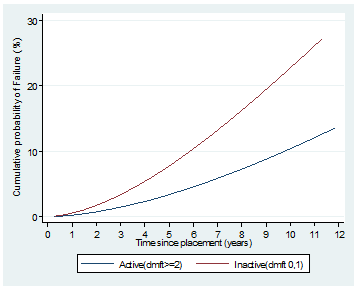
Figure 3: Estimated cumulative probability of failure by dmft experience.
|
Intact N (%) |
Failed N (%) |
Overall N (%) |
p-value |
|
|
Total sample (teeth) |
164 (100) |
13 (100) |
177 (100) |
|
|
Total sample (patients) |
127 (100) |
12(100) |
139 (100) |
|
|
Caries risk group |
0.104 |
|||
|
Low (dmft or DMFT ≤ 1) |
88 (53.7) |
10 (76.9) |
98 (55.4) |
|
|
High (dmft or DMFT >1) |
76 (46.3) |
3 (23.1) |
79 (44.6) |
|
|
Material |
0.632 |
|||
|
Amalgam |
77 (47.0) |
7 (53.8) |
84 (47.5) |
|
|
Resin |
87 (53.0) |
6 (46.2) |
93 (52.5) |
|
|
Visit frequency |
0.293 |
|||
|
Every 6 months |
22 (13.4) |
0 (0.0) |
22 (12.4) |
|
|
Every year |
45 (27.4) |
3 (23.1) |
48 (27.1) |
|
|
Occasionally |
97 (59.1) |
10 (76.9) |
107 (60.5) |
|
|
Gum bleeding |
<0.001 |
|||
|
Yes |
156 (95.1) |
7 (53.8) |
163 (92.1) |
|
|
No |
8 (4.9) |
6 (46.2) |
14 (7.9) |
|
|
Tooth brushing |
0.028 |
|||
|
No Brushing |
1 (0.6) |
0 (0.0) |
1 (0.6) |
|
|
Sporadically |
11 (6.7) |
4 (30.8) |
15 (8.5) |
|
|
Once a day |
95 (57.9) |
6 (46.2) |
101 (57.1) |
|
|
More than twice a day |
57 (34.8) |
3 (23.1) |
60 (33.9) |
|
|
Use of fluoride mouthrinse |
0.048 |
|||
|
No |
19 (11.6) |
4 (30.8) |
23 (13.0) |
|
|
Yes |
145 (88.4) |
9 (69.2) |
154 (87.0) |
|
|
Use of floss |
0.188 |
|||
|
No flossing |
92 (56.1) |
10 (76.9) |
102 (57.6) |
|
|
Sporadically |
66 (40.2) |
2 (15.4) |
68 (38.4) |
|
|
Once a day |
6 (3.7) |
1 (7.7) |
7 (4.0) |
|
Table 3: Descriptive Statistics for the restorations that failed (either because of caries or marginal ridge fracture).
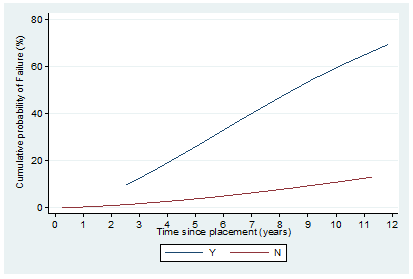
Figure 4: Estimated cumulative probability of failure by gum bleeding.
4. Discussion
In this clinical study, a rather new approach was evaluated regarding the definite diagnosis and conservative restoration of incipient proximal carious lesions that are detected on bitewing radiographs but are not seen clinically before separation with elastic separators. Results showed that the procedure besides its use on diagnosing whether a proximal radiographically detected carious lesion is “cavitated or not”, can be used as an alternative technique for the preparation and restoration of proximal carious lesion with good results. The major problem with proximal carious lesions is the definite diagnosis of the cavitation. Radiographs have good accuracy on detecting early carious lesions but they cannot differentiate if they are cavitated or not. In this study, elastic separators were used as they are suggested in the literature [20]. Separation of the teeth allows for a definite diagnosis and acknowledgment of the cavitation while also facilitates the decision whether a preventive or restorative approach should be implemented for the lesion. Visual examination has a great range of sensitivity and specificity when it comes to the diagnosis of incipient carious lesions [21]. This depends on the surface under examination and the accuracy of the method improves with the use of specific indexes [22]. The experience from this study suggests that the use of elastic separators was very well accepted by the patients and their parents. A minimal discomfort was reported mainly in older children probably because of the tighter contacts due to the eruption of the second molars. This has been reported as a side effect of elastic separator placement during orthodontic treatment, but with no severe consequences [23]. Care must be taken when placing the separator not to injure the periodontal tissues because this will increase the discomfort of the patient. Another disadvantage of the technique is the need for a second appointment after placement of the separator.
In the context of minimal invasive dentistry, conservative cavity preparation designs have been suggested. For proximal surfaces the designs used so far include saucer and tunnel shape preparations. A study on the direct comparison of survival rates of these designs has shown, for a 4 year time period, 76% survival for saucer compared to 46% for tunnel [14]. These findings for both techniques are similar with other studies [11] and much lower success rates than the approach presented here (92.3%). The main reason of failure of these conservative designs is marginal ridge fracture for the tunnel and secondary caries for the saucer shape. In the technique presented here the advantage is that by having a direct approach to the lesion and the cavity preparation it is possible to have a better estimation of the remaining tooth structure at the marginal ridge and also remove caries more accurately and design a more appropriate cavity for the material used. This might be the reason leading to only 12 (6.8%) restorations exhibiting marginal ridge failure while 13 (7.3%) failed regardless of the reason of failure. To our knowledge this is the first paper that evaluates the survival rate of this restorative method of interproximal caries. When it comes to conventional interproximal cavity design for class II restorations, the survival rate of posterior restorations ranges from 92.5% to 92.8 % for amalgam and 86.2% to 85.8% for composite resins. The results from this study showed very similar success with the literature for the amalgam restorations (91.6%) and better performance (93.5%) for the composite resin restorations. This difference in the performance of the two materials was not found to be statistically significant while literature suggests that amalgam restorations usually exhibit better performance than composites. Composite placement is a highly sensitive and operator depended technique, while newest materials present better properties than the older ones. In our study all restorations were place by one very skilled dentist and this minimized the failures due to variability of operator skills as far as cavity preparation and material handling.
Skudutyte-Rysstad et al., [24] showed that intact tooth surfaces adjacent to newly placed composites have a higher possibility to develop caries and this is mainly attributed to iatrogenic damage, which is a frequent side-effect of operative treatment of approximal carious lesions. Using the separation method, this side effect is minimized, since there is a small distance between the tooth that is prepared and the adjacent tooth. This could be a further advantage of this technique, but further research is needed to verify it. Today, a more conservative approach has been suggested for restoration of initial interproximal lesions using resin infiltration. The systematic review of Doméjean et al., [25] indicates that “this is an effective method to arrest the progression of non-cavitated caries lesions”. The resin infiltration technique was consider invasive since a layer of 100 nm of enamel must be removed as a prerequisite of the technique and was compared to none invasive procedures (flossing, diet control, fluoride varnish application). The lesions in all studies were detected on radiographs, without knowing on whether they are cavitated or not. Considering all these factors it is difficult to compare the infiltration technique with the technique presented here, since different principles have been used for the diagnosis and management of the lesion.
Regarding caries risk, the patients were divided in low and high caries risk groups. Usually caries risk systems categorize in low, medium and high the risk [26]. Since guidelines on the prevention and management of patients are the same for low and medium risk, we collapsed the two categories in one defined by having up to one carious lesion. An interesting finding is that there was no difference in the survival rate of the restorations in low and high caries risk patients in this study. This could be attributed to the fact that the population of the study originated from a private dental practice, where patients usually follow better oral health habits and more regular recall dental visits. Interestingly enough the factors that improved the performance of the technique was the use of mouthrinse, the absence of bleeding and the frequency of brushing. The use of mouthrinse and the frequent brushing is directly associated with the presence of fluoride in the mouth but the abscess of bleeding also suggests frequent brushing and again presence of fluoride through the toothpaste. In the literature, it is very well established the protective effect that fluoride has on the smooth surfaces of the teeth. The main advantage of this technique is the minimal tooth loos since there is no extension to occlusal surface and the marginal ridge of the tooth is preserved. Careful selection of the cases combined for this new approach, can reduce the use of the typical class II restorations and give more long term survival rates and better aesthetics to the restorations for the benefit of the patients. Limitations of the study might be considered that it requires two appointments, one for the placement of the separators and a second one for restoring the lesion. In some instances the elastic is lost and there is a need of one more appointment to reinsert them.
5. Conclusions
Temporary separation of the proximal surfaces of teeth with orthodontic elastic separators, besides its use on differentiating a proximal radiographically detected carious lesion is “cavitated or not”, can be used effectively as an alternative technique for preparing and restoring class II cavitated carious lesions as class I, preserving the marginal ridge of the tooth and fulfilling the principles of minimal invasion dentistry.
Competing Interests
The authors declare that they have no competing
interests.
References
- Kassebaum NJ, Bernabé E, Dahiya M, et al. Global burden of untreated caries: a systematic review and metaregression. J Dent Res 94 (2015): 650-658.
- Peters MC, McLean ME. Minimally invasive operative care. J Adhes Dent 3 (2001): 7-16.
- Dummer PMH, Addy M, Oliver SJ, et al. Changes in the distribution of decayed and filled tooth surfaces and the progression of approximalcaries in children between the ages of 11-12 years and 15-16 years. Br Dent J 164 (1988): 277-282.
- Mejare I, Kallestal C, Stenlund H, et al. Caries development from 11 to 22 years of age: a prospective radiographic study. Prevalence and distribution Caries Res 32 (1998): 10-16.
- Flink A, Kallestal C, Holm A, et al. Distribution of caries in 12-year-old children in Sweden. Social and oral health-related behavioural patterns. Comm Dent Oral Epidemiol 16 (1999).
- Llena-Puy C, Forner L. A clinical and radiographic comparison of caries diagnosed in approximal surfaces of posterior teeth in a low-risk population of 14-year-old children. Oral Heal. Prev Dent 3 (2005): 47-52.
- Ritter AV, Ramos M Da, Astorga F, et al. Visual-tactile versus radiographic caries detection agreement in caries-active adults. J Pub Heal. Dent 73 (2013): 252-260.
- Moraschini V, Fai CK, Alto RM, et al. Amalgam and resin composite longevity of posterior restorations: A systematic review and meta-analysis. J Dent 43 (2015): 1043-1050.
- Hurst D. Amalgam or composite fillings--which material lasts longer?. Evid. Based. Dent 15 (2014): 50-51.
- Forss H, Widström E. The post-amalgam era: a selection of materials and their longevity in the primary and young permanent dentitions. Inter J Paediatr Dent 13 (2003): 158-164.
- Kopperud SE, Tveit AB, Gaarden T, et al. Longevity of posterior dental restorations and reasons for failure. Eur J Oral Sci 120 (2012): 539-548.
- McComb D. Systematic review of conservative operative caries management strategies. J Dent Educ 65 (2001): 1154-1161.
- Mount GJ. Minimal intervention dentistry: rationale of cavity design. Oper Dent 28 (2003): 92-99.
- Hörsted-Bindslev P, Heyde-Petersen B, Simonsen P, et al. Tunnel or saucer-shaped restorations: a survival analysis. Clin Oral Invest 9 (2005): 233-238.
- Baelum V, Hintze H, Wenzel A, et al. Implications of caries diagnostic strategies for clinical management decisions. Commun Dent Oral Epidemiol 40 (2012): 257-266.
- Leggat PA, Smith DR. Musculoskeletal disorders self-reported by dentists in Queensland, Australia, Aust. Dent. J 51 (2006): 324-327.
- Ryge G, Jendresen M Da, Glantz PO, et al. Standardization of clinical investigators for studies of restorative materials. Swed Dent J 5 (1981): 235-239.
- Royston P. Flexible parametric alternatives to the Cox model, and more. Stata J 1 (2001): 1-28.
- Royston P, Parmar MKB. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat. Med 21 (2002): 2175-2197.
- Seddon RP. The detection of cavitation in carious approximal surfaces in vivo by tooth separation, impression and scanning electron microscopy. J Dent 17 (1989): 117-120.
- Gomez J, Tellez M, Pretty IA, et al. Non-cavitated carious lesions detection methods: a systematic review. Comm Dent Oral Epidemiol 41 (2013): 55-73.
- Gimenez T, Piovesan C, Braga MM, et al. Visual Inspection for Caries Detection: A Systematic Review and Meta-analysis. J Dent Res 94 (2015): 895-904.
- Farronato G, Giannini L, Galbiati G, et al. Oral tissues and orthodontic treatment: common side effects. Minerva Stomatol 62 (2013): 431-446.
- Skudutyte-Rysstad R, Tveit AB, Espelid I, et al. Posterior composites and new caries on adjacent surfaces - any association? Longitudinal study with a split-mouth design. BMC Oral Health 16 (2016): 11.
- Doméjean S, Ducamp R, Léger S, et al. Resin infiltration of non-cavitated caries lesions: a systematic review. Med Princ Pr 24 (2015): 216-221.
- Tellez M, Gomez J, Pretty I, et al. Evidence on existing caries risk assessment systems: are they predictive of future caries?. Commun Dent Oral Epidemiol 41 (2013): 67-78.
- Anusavice KJ. Present and Future Approaches for the Control of Caries. J Dent Educ 69 (2005): 538-554.
