Rare Computed Tomography Findings of Multiple Unihemispheric Brain Stones in A Patient Presenting Following Her First Seizure
Article Information
Raees Lunat*, Rahul Khamar, Jonathon Kyriakides
Emergency Department, Barnet Hospital, Royal Free London NHS Foundation Trust, England, UK
*Corresponding Author: Dr. Raees Lunat, Emergency Department, Barnet Hospital, Royal Free London NHS Foundation Trust, England, UK
Received: 07 May 2020; Accepted: 19 May 2020; Published: 01 July 2020
Citation: Raees Lunat, Rahul Khamar, Jonathon Kyriakides. Rare Computed Tomography Findings of Multiple Unihemispheric Brain Stones in A Patient Presenting Following Her First Seizure. Journal of Radiology and Clinical Imaging 3 (2020): 069-073
Share at FacebookAbstract
Brain stones are a rare form of intracranial calcification. They are defined as large, well-circumscribed foci of pathological calcification and can be classified according to location and aetiopathology. Clinical history and imaging are principally used to narrow the differential in the absence of a tissue diagnosis. We report the highly unique case of a 47-year-old female patient who presented following a witnessed tonic-clonic seizure, preceded by worsening neurological symptoms. Blood tests were unremarkable however imaging demonstrated multiple, large, discrete areas of bony hard calcifications that were distributed exclusively within the left cerebral hemisphere - a localisation characteristic that is unreported in literature to date.
Keywords
Intracranial; Calcification; Brain stones; Computed tomography; Magnetic resonance imaging; Seizure; First seizure
Intracranial articles, Calcification articles, Brain stones articles, Computed tomography articles, Magnetic resonance imaging articles, Seizure articles, First seizure articles
Intracranial articles Intracranial Research articles Intracranial review articles Intracranial PubMed articles Intracranial PubMed Central articles Intracranial 2023 articles Intracranial 2024 articles Intracranial Scopus articles Intracranial impact factor journals Intracranial Scopus journals Intracranial PubMed journals Intracranial medical journals Intracranial free journals Intracranial best journals Intracranial top journals Intracranial free medical journals Intracranial famous journals Intracranial Google Scholar indexed journals Calcification articles Calcification Research articles Calcification review articles Calcification PubMed articles Calcification PubMed Central articles Calcification 2023 articles Calcification 2024 articles Calcification Scopus articles Calcification impact factor journals Calcification Scopus journals Calcification PubMed journals Calcification medical journals Calcification free journals Calcification best journals Calcification top journals Calcification free medical journals Calcification famous journals Calcification Google Scholar indexed journals Brain stones articles Brain stones Research articles Brain stones review articles Brain stones PubMed articles Brain stones PubMed Central articles Brain stones 2023 articles Brain stones 2024 articles Brain stones Scopus articles Brain stones impact factor journals Brain stones Scopus journals Brain stones PubMed journals Brain stones medical journals Brain stones free journals Brain stones best journals Brain stones top journals Brain stones free medical journals Brain stones famous journals Brain stones Google Scholar indexed journals Computed tomography articles Computed tomography Research articles Computed tomography review articles Computed tomography PubMed articles Computed tomography PubMed Central articles Computed tomography 2023 articles Computed tomography 2024 articles Computed tomography Scopus articles Computed tomography impact factor journals Computed tomography Scopus journals Computed tomography PubMed journals Computed tomography medical journals Computed tomography free journals Computed tomography best journals Computed tomography top journals Computed tomography free medical journals Computed tomography famous journals Computed tomography Google Scholar indexed journals Magnetic resonance imaging articles Magnetic resonance imaging Research articles Magnetic resonance imaging review articles Magnetic resonance imaging PubMed articles Magnetic resonance imaging PubMed Central articles Magnetic resonance imaging 2023 articles Magnetic resonance imaging 2024 articles Magnetic resonance imaging Scopus articles Magnetic resonance imaging impact factor journals Magnetic resonance imaging Scopus journals Magnetic resonance imaging PubMed journals Magnetic resonance imaging medical journals Magnetic resonance imaging free journals Magnetic resonance imaging best journals Magnetic resonance imaging top journals Magnetic resonance imaging free medical journals Magnetic resonance imaging famous journals Magnetic resonance imaging Google Scholar indexed journals Seizure; First seizure articles Seizure; First seizure Research articles Seizure; First seizure review articles Seizure; First seizure PubMed articles Seizure; First seizure PubMed Central articles Seizure; First seizure 2023 articles Seizure; First seizure 2024 articles Seizure; First seizure Scopus articles Seizure; First seizure impact factor journals Seizure; First seizure Scopus journals Seizure; First seizure PubMed journals Seizure; First seizure medical journals Seizure; First seizure free journals Seizure; First seizure best journals Seizure; First seizure top journals Seizure; First seizure free medical journals Seizure; First seizure famous journals Seizure; First seizure Google Scholar indexed journals haemorrhage articles haemorrhage Research articles haemorrhage review articles haemorrhage PubMed articles haemorrhage PubMed Central articles haemorrhage 2023 articles haemorrhage 2024 articles haemorrhage Scopus articles haemorrhage impact factor journals haemorrhage Scopus journals haemorrhage PubMed journals haemorrhage medical journals haemorrhage free journals haemorrhage best journals haemorrhage top journals haemorrhage free medical journals haemorrhage famous journals haemorrhage Google Scholar indexed journals London Ambulance System articles London Ambulance System Research articles London Ambulance System review articles London Ambulance System PubMed articles London Ambulance System PubMed Central articles London Ambulance System 2023 articles London Ambulance System 2024 articles London Ambulance System Scopus articles London Ambulance System impact factor journals London Ambulance System Scopus journals London Ambulance System PubMed journals London Ambulance System medical journals London Ambulance System free journals London Ambulance System best journals London Ambulance System top journals London Ambulance System free medical journals London Ambulance System famous journals London Ambulance System Google Scholar indexed journals Fundoscopy articles Fundoscopy Research articles Fundoscopy review articles Fundoscopy PubMed articles Fundoscopy PubMed Central articles Fundoscopy 2023 articles Fundoscopy 2024 articles Fundoscopy Scopus articles Fundoscopy impact factor journals Fundoscopy Scopus journals Fundoscopy PubMed journals Fundoscopy medical journals Fundoscopy free journals Fundoscopy best journals Fundoscopy top journals Fundoscopy free medical journals Fundoscopy famous journals Fundoscopy Google Scholar indexed journals CT scanner articles CT scanner Research articles CT scanner review articles CT scanner PubMed articles CT scanner PubMed Central articles CT scanner 2023 articles CT scanner 2024 articles CT scanner Scopus articles CT scanner impact factor journals CT scanner Scopus journals CT scanner PubMed journals CT scanner medical journals CT scanner free journals CT scanner best journals CT scanner top journals CT scanner free medical journals CT scanner famous journals CT scanner Google Scholar indexed journals
Article Details
1. Introduction
In the initial clinical work-up of a patient presenting following a first seizure, computed tomography (CT) and magnetic resonance imaging (MRI) of the brain play a pivotal role. Differentials that can be evaluated on neuroimaging imaging include: stroke, post-traumatic sequelae, haemorrhage, neoplastic, mesial temporal sclerosis, malformation of cortical development, cavernoma and perinatal insult [1]. Several reviews have also demonstrated the value of MRI, beyond that of CT in identifying epileptogenic lesions with a greater sensitivity [2]. The numerous causes of intracranial calcifications (both physiological and pathological) are also well documented in the literature [3] however little is known regarding the rare finding of brain stones and the determinants of their development.
2. Case Description
A 47-year-old Portugese female patient initially presented to our Emergency Department in February 2020 after experiencing her first seizure. The London Ambulance System (LAS) conveyed this patient to our department after the seizure self-terminated where she underwent a thorough clinical assessment. The patient revealed a two-week history of a predominantly frontal “band like” headache which she had never experienced before. This headache was persistent and would intermittently worsen in severity over the course of the two-week period. It would often start upon waking in the morning and at its worst, last up to four hours. Simple analgesics including paracetamol did not provide any symptomatic relief. There were no other pathognomonic features that would suggest the aetiology of this headache was related to migraine, raised intracranial pressure, or meningism. This patient denied any history of foreign travel or fever. Of note, she revealed a 3-month history of blurred vision. No recent eye tests were reported and she did not wear glasses. There was no notable past medical or surgical history.
The generalised tonic-clonic seizure was witnessed by her husband who observed the patient lose consciousness before noting rhythmic jerking movements of the upper and lower limbs. He also reported associated tongue biting and urinary incontinence. The seizure lasted approximately five minutes before self-terminating. The patient, who was described as being in a post-ictal phase following the seizure, was then placed into recovery position before an ambulance was called. On assessment by paramedics, the patient had no memory of these events, remembering only the moment at which she was asked to open her mouth (which revealed blood from having bitten her own tongue).
On examination, her observations were all within normal range, with a normal cardiac, respiratory and abdominal examination. She also had a normal central nervous system examination, peripheral nervous system examination (including both upper and lower limbs) as well as a normal cerebellar examination. Fundoscopy was also unrevealing. Initial blood tests were largely unremarkable with a normal full blood count, renal function and bone profile. Notably, the serum sodium, adjusted calcium and magnesium levels (significant derangements of which can potentially precipitate seizure activity) were all normal at 139 mmol/L, 2.47 mmol/L and 0.80 mmol/L, respectively. Curiously, there was no elevation in lactate on the venous blood gas.
An unenhanced CT examination of the brain by a 64-slice CT scanner was performed. The protocol included a non-contrast CT scan with a 1mm slice thickness. As demonstrated in Figure 1, multiple extra-axial solid calcifications were found to be scattered throughout the subarachnoid space of the left cerebral hemisphere. The largest, measuring 2.4 cm in length and 0.8 × 0.9 cm in cross-section, was noted to be occupying the large part of the left sylvian fissure. A gadolinum-enhanced MRI was also performed for further evaluation of aetiology. Figure 2 illustrates the diffusion-weighted imaging sequence of the MRI which illustrates signal dropout at the cortical areas corresponding to the site of the brain stones. There was no abnormalities detected in the post-contrast images, in-keeping with a diagnosis of ‘benign brain stones’.
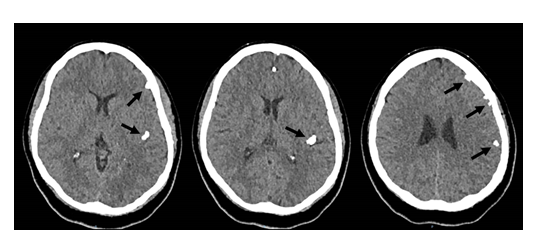
Figure 1: Unenhanced CT scan of the brain from Febraury 2020 illustrating multiple extra-axial calcific densities (‘brain stones’) in various of the L cerebral hemisphere; the largest occupying the posterior part of the left sylvian fissure and others distrubted peripherally.
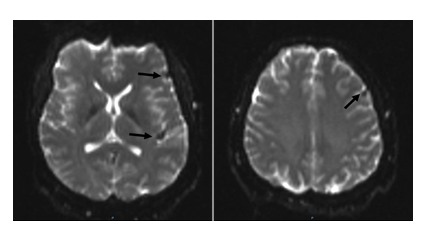
Figure 2: Diffusion weighted images from an MRI scan of the brain from Febraury 2020 illustrating signal ‘drop-out’ in the corresponding areas of the L cerebral hemisphere where brain stones were detected on CT imaging.
Following review by the in-patient neurology team, this patient was initiated on levetiracetam 250 mg BD, to be up-titrated following two weeks to 500 mg BD.
3. Discussion
Brain stones, also known as cerebral calculi, are a rare phenomenon. They can be classified according to their aetiology and distribution. Brain stones is the general term used to refer to “large, solitary or multiple, well circumscribed bony hard areas of pathological calcification” [4]. Intracranial calcifications are commonly reported in the literature however the finding of brain stones is less frequently encountered. Both phenomena are commonly detected incidentally or following either sudden neurological disturbance (e.g. a seizure) or progressive neurological symptoms (persistent worsening headaches or visual changes) [5].
Primarily, brain stones are classified on the basis of their location, i.e. whether they are intra-axial (within the parenchyma of the brain) or extra-axial (external to brain parenchyma). Whilst extra-axial stones typically arise from tumours or exaggeration of physiological calcification, the differential for intra-axial stones is vast and can be further classified according to aetiogenesis: neoplastic, vascular, infectious, congenital, endocrine or metabolic [6]. Meningiomas are an important cause of extra-axial brain stones with one study citing up to 60% of cases demonstrating some degree of macroscopic calcification [7]. Other pathological causes include dural osteomas (thought to be arising secondary to ossification of the fibrous dural coverings) and calcifying tumours such as craniopharyngeomas. Physiological calcifications that can affect numerous cortical areas including the pineal gland, habenula, basal ganglia and the dural coverings can, if accentuated, can give the appearance of brain stones [6].
Typically, brain stones are undetectable on plain skull x-rays due to the amount and configuration of calcium salts they contain. The superiority of CT in detecting intracranial calcification as compared to plain film imaging has resulted in CT being commonly used to quantify calcification. CT is also considered to be better than MRI in identifying and characterising intracranial calcification. However, T2-weighted MRI imaging has shown to correlate better with clinical symptoms than with CT identified calcifications. Hence, evaluation with both imaging modalities is recommended [8].
This particular case is of significant interest due to the finding of multiple, discrete brain stones that were distributed solely across a single cerebral hemisphere. All cases identified in the literature to date have reported either a singular focus of dense calcification or multiple scattered foci that are not restricted to a single cerebral hemisphere [3]. Furthermore, whilst it’s uncommon for brain stones to manifest with a seizure; their location in such circumstances is almost always intra-axial as opposed to extra-axial. In addition to this, the majority of patients with brain stones are asymptomatic and as a result, often go undiagnosed. The median age of symptomatic patients who do present is 70, with the finding rarely reported in patients under the age of 50 [9].
Treatment for brain stones is often limited to anti-seizure medication in the majority of cases (as in our patient). In highly symptomatic individuals, surgical resection is a potential alternative however total resection is rare due to the potential for complications and so the symptomatic mass is often removed with close follow-up in case of need for further neuro- or radiosurgery [10].
References
- Ho K, Lawn N, Bynevelt M, et al. Neuroimaging of first-ever seizure: Contribution of MRI if CT is normal. Neurology: Clinical Practice 3 (2013): 398-403.
- So E. Role of Neuroimaging in the Management of Seizure Disorders. Mayo Clinic Proceedings 77 (2002): 1251-1264.
- Kiroglu Y, Calli C, Karabulut N, et al. Intracranial calcifications on computed tomography: pictorial essay. Diagnostic and Interventional Radiology 16 (2009): 263-269.
- Tiberin P, Beller A. Observations on so-called brain stones or cerebral calculi. Neurology 13 (1963): 464-464.
- Gezercan Y, Acik V, Çavu? G, et al. Six different extremely calcified lesions of the brain: brain stones. SpringerPlus 5 (2016).
- Celzo F, Venstermans C, De Belder F, et al. Brain stones revisited—between a rock and a hard place. Insights into Imaging 4 (2013): 625-635.
- Grech R, Grech S, Mizzi A. Intracranial Calcifications. The Neuroradiology Journal 25 (2012): 427-451.
- Holland B, Kucharczyk W, Brant-Zawadzki M, et al. MR imaging of calcified intracranial lesions. Radiology 157 (1985): 353-356.
- Watts J, Singh J, Schoppe C, Johnson A. Calcified intracranial masses. Clin Neuroradiol 22 (2012): 253-256.
- Chaturvedi M, Janu V, Kumari R, et al. Congenital Skull Anomaly with Multiple Brain Stones and Symptomatic Meningioma of Medial Sphenoid Wing. Asian Journal of Neurosurgery 13 (2018): 822-825.
