Psychosis and Cannabis: Could a Hasty Diagnosis and Treatment of Schizophrenia be Harmful?
Article Information
Zoé Boulot1, Franck Gabayet F1, Mathieu Besnard1, Nathalie Coulon1,2,3*
1Schizophrenia Expert Center with Psychosocial Rehabilitation Reference Center, Alpes Isère Hospital (Saint-Egrève Psychiatric Hospital, 38 120 Saint-Egrève), 38 000 Grenoble, France
2Fondation FondaMental, 94 000 Créteil, France
3INSERM U955, Translational Psychiatry laboratory, AP-HP, DHU Pe-PSY, Schizophrenia Expert Center, Henry Mondor University Hospitals, Pole of Psychiatry and Addictology, Paris Est Créteil University, 40 rue de Mesly, 94 000 Créteil, France
*Corresponding Author: Nathalie Coulon, MD PhD, Psychiatrist and Child Psychiatrist, Schizophrenia Expert Center with Psychosocial Rehabilitation Reference Center, Alpes Isère Hospital (Saint-Egrève Psychiatric Hospital, 38 120 Saint-Egrève), 38 000 Grenoble, France, https://orcid.org/0000-0001-7765-1117
Received: 13 July 2021; Accepted: 10 August 2021; Published: 31 August 2021
Citation: Zoé Boulot, Franck Gabayet F, Mathieu Besnard, Nathalie Coulon. Psychosis and Cannabis: Could a Hasty Diagnosis and Treatment of Schizophrenia be Harmful?. Archives of Clinical and Medical Case Reports 5 (2021): 610-617.
Share at FacebookAbstract
We describe a young male patient who questions his diagnosis of schizophrenia made 10 years ago, and whose clinical presentation and history seem in favour of cannabisinduced psychotic episodes. This case questions the risk of a hasty diagnosis when it comes to concomitant psychosis and cannabis use. This presentation raises medical, therapeutical, and ethical questions. With cannabis use rising globally, cases like this are bound to multiply. There are no evident clinical distinctions between psychosis such as schizophrenia, and cannabis-induced psychosis described in literature, nor evidence-based guidelines on the care patients should benefit from. Further research is therefore needed.
Keywords
Cannabis-induced psychosis; Schizophrenia; Cannabis; Cannabis use disorder; Substance-induced psychosis
Cannabis-induced psychosis articles; Schizophrenia articles; Cannabis articles; Cannabis use disorder articles; Substance-induced psychosis articles
Article Details
Abbreviations:
PANSS- Positive and Negative Syndrome Scale; CGI- Clinical Global Impressions; THC- TetraHydroCannabinol; CBD- CannaBiDiol
1. Introduction
The drug market has been remarkably resilient despite the disruption caused by the COVID-19 pandemic and, in Europe, the most commonly tried drug is still cannabis (47.6 million males and 30.9 million females) [1]. The prevalence of European cannabis use is about five times that of other substances [1-2]. For public health however, it is now clear that the most psychoactive part of the cannabis (tetrahydrocannabinol=THC) can induce psychotic-like symptoms in healthy individuals [3]. In a meta-analysis, Marconi et al. [4] showed there was an association between the level of consumption of cannabis and psychosis; authors calculated an OR of 3.90 (95% CI 2.84 to 5.34) for the risk of schizophrenia and other psychosis-related outcomes among heavy cannabis users compared to nonusers. Thus, many studies consider cannabis use as a risk factor for the development of schizophrenia [4].
To be more precise on the side of semiology and terminology, cannabis-induced psychosis is a clinical entity both in ICD-10 [5] and in DSM-5 [6]. The difference between schizophrenia associated with the use of cannabis and cannabis-induced psychosis could therefore be slim. Some studies suggest there could even be shared genetic vulnerabilities [7-8]. Moreover, clinical characteristics during acute phases seem similar in cannabis-induced psychosis and schizophrenia (with or without cannabis abuse or dependence) [9]. In rentero et al. [9], the few differences concern the age of the patients (lower for cannabis-induced psychosis), lower means on the PANSS negative subscale, fewer auditory hallucinations, and greater presence of mania. Amotivational syndrome is also commonly associated with cannabis use, which could be mistaken for negative symptoms of schizophrenia. Petrucci et al. [10] have indeed shown there is a statistically significant relationship between cannabis and apathy.
Nevertheless, although cannabis-induced psychosis is a clinical entity of its own, Starzer et al. [11] revealed that 41.2 % (95 % CI=36.6-46.2) of patients who received a diagnosis of cannabis-induced psychosis between 1994 and 2014 in Denmark converted to schizophrenia. The risk of schizophrenia after a cannabis-induced psychotic episode therefore seems high. Starzer et al.’s study also identified predictors for conversion: younger age at which the cannabis-induced psychosis occurred, substance use disorder, eating disorders.
Current guidelines emphasized the importance of prompt treatment in psychotic episodes to reduce the duration of untreated psychosis [12]. Recommendations on duration of maintenance treatment vary from a minimum of one year, to at least two years for first-episode patients, and between two to five years for multi-episode patients. However, few recommendations exist on treatment of cannabis-induced psychosis.
2. Case Presentation
A 32-year-old man consulted in our Schizophrenia Expert Center to reconsider his diagnostic of schizophrenia received ten years ago. Our team belongs to a French national network, set up by a scientific cooperation foundation in France, the FondaMental Foundation (www.fondation-fondamental.org). We use standardized and extensive clinical and neuropsychological batteries, with ethical principles for medical research involving humans (WMA, Declaration of Helsinki). All data were collected anonymously. A non-opposition form was signed.
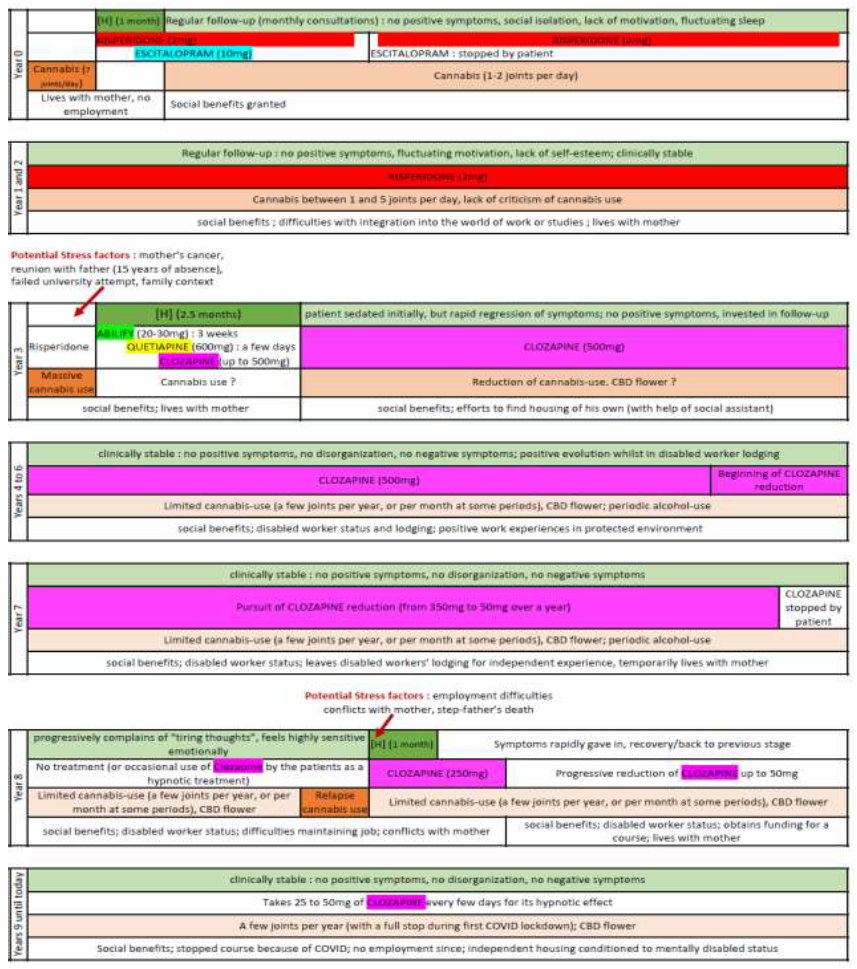
The man was cooperating, and his current medical and social team supported him in this process. During the first consultation, he described three hospitalisations that occurred following psychotic episodes in year 0, year 3 and year 5 (See please figure 1). Each time, the subject presented delusions of persecution, ideas of reference and was agitated, but he has never expressed hallucinations. These episodes coincided with cannabis use. Symptoms were not mood congruent. The subject also described he started cannabis use at age 15 with friends, and never really stopped. His first memory of cannabis was of the smell, when he was 6 years old; the smell still had a very strong effect on him (the craving was still strong). Currently, he smoked a few joints of cannabis per year, and used CBD flower regularly. Finally, he detailed various treatments he benefitted from during the last ten years: risperidone, escitalopram, ariprazole, quetiapine, zuclopenthixol and clozapine. At the time of the consultation, he had a prescription for 50 mg of clozapine per day but explained he took 25 to 50 mg every few days, for its hypnotic effect. Exploring his childhood found no evidence of physical abuse, but emotional deprivation seemed obvious. His mother also had several drug addictions (heroine, alcohol), which probably explained his placement for a few years after his parents separated.
During clinical evaluation, the subject had a neat appearance; his speech volume, rhythm and tone were normal; he answered precisely and informatively. Emotional expression was appropriate to content. His thoughts were logical with no evidence of flight of ideas, nor loosening of associations. There was no evidence for delusional thoughts or mistrust, nor perceptual or sensory abnormalities. He did not show any difficulty concentrating or memorizing. Abstract reasoning seemed functional. So, even though the subject took clozapine at an ineffective dosage, the patient’s presentation would seem inappropriate with a diagnosis of schizophrenia, often associated with cognitive impairment, residual negative symptoms, and disorganisation.
Furthermore, the depth analysis of the subject’s clinical records revealed the hospitalisations always occurred in a context of cannabis use (Figure 1). Stress factors preceding these psychotic episodes were also identified (Figure1). Psychotic symptoms diminished rapidly during his first and third hospitalisation. The second hospitalisation was the longest, symptoms lasted longer, and several treatments were tried, resulting in a prescription of clozapine. In between hospitalisations, no positive symptoms or disorganisation were observed; absence of motivation and a form of apathy were occasionally described. The subject benefited from psychiatric follow-up, social assistance and protected employment and housing. In years 6-7, the diagnosis was first questioned, and clozapine was progressively diminished, and stopped (year 8) with no symptomatic recurrence until the third and last hospitalisation at the end of the year, following stressful life events and recurrence of cannabis use. Since then, despite the ineffective use of clozapine (25-50 mg of clozapine every few days) the subject has not presented positive or negative symptoms, nor signs of disorganization. The clinical history was therefore also inappropriate with the diagnosis of schizophrenia.
Complementary clinical explorations found no present symptoms of schizophrenia. Indeed, the score of the Positive and Negative Syndrome Scale (PANSS) [13] was not in favour of schizophrenic symptoms: positive PANSS subscale was of 10, negative PANSS subscale was of 7 and total score was of 37. According to Leucht et al [14], being considered “mildly ill” according to the CGI corresponds to a PANSS’ score of 58. Furthermore, Calgary Depression Scale for Schizophrenia [15] was in favour of absence of depressive symptoms (score=2).
About neuropsychological assessment, no cognitive impairment was detected. The estimated intellectual quotient (according to Denney) was of 114. Executive functions, abstract thinking, memory functions, social cognition and intellectual abilities were within the range of normal, if not, slightly higher than standard. Only planning and organising capacities were slightly lower than standard. In the same way, initial brain imagery and biology provided no arguments in favour of a neurological, metabolic, infectious or any other explanation for the observed symptoms.
Consequently, the clinical presentation and history therefore seemed to be in favour of several cannabis-induced psychotic episodes.
3. Discussion
This clinical case highlights the importance of a cautious diagnosis of schizophrenia when there is a cannabis use in the story of a subject. Questions are closely intertwined concerning diagnoses and medical treatment, but also several ethical problems. The existence of a link between cannabis and psychosis is common knowledge, but the nature of this link remains unclear. Some studies have suggested there could be a common genetic baggage [7-8], while others insist on a correlation between the level of cannabis use and the risk of psychosis [3], or still others suggest cannabis use is a risk factor for psychosis [9], and even a risk for early onset of schizophrenia [16]. Moreover, schizophrenia is frequently associated with cannabis-use and there seems to be a high risk of conversion to schizophrenia after a cannabis-induced psychosis. However, this case-report showed that cannabis-induces psychotic episodes could also probably occur repetitively, without necessarily converting to schizophrenia. The distinction between schizophrenia and cannabis-induced disorders is not always so obvious, and our experience is an invitation to precautious diagnosis of schizophrenia when cannabis use is associated.
This clinical experience also highlights the interest of a multidisciplinary approach, in particular around psychosis and addictions. In our case, the importance of diagnosing and treating addiction was put in the background because the patient defeated it and had found illegal income, which he was hiding, through the drug environment.
Furthermore, the case report underlines the semiological overlap between clinical characteristics of psychotic episodes in schizophrenia, with cannabis abuse or dependence, and cannabis-induced psychosis. In-depth analysis and close attention to clinical symptoms could be necessary to pinpoint the exact diagnosis. In addition, to distinguish schizophrenia associated with cannabis use, and cannabis-induced psychosis, further explorations seem necessary. Indeed, clinical characteristics are currently described as very similar, further research could be helpful to identify discriminating factors.
Specifying the diagnosis could facilitate the therapeutic line. So, better distinguishing between these entities, schizophrenia with/ without cannabis use, and cannabis-induced psychosis, could be particularly significant when it comes to treating a patient. Indeed, there seems to be no current precise guidelines on treatment of cannabis-induced psychosis. This suggests further explorations on treatment of cannabis-induces psychosis are needed. In the meantime, when treated with antipsychotics, as in this case, treatment probably follows guidelines established for psychotic episodes. Are those guidelines adequate? Do many patients benefit from a maintenance treatment? And if so, is that what is best for them? Are these treatments harmful if the patient suffers from a cannabis-induced psychosis and not schizophrenia? Many questions that further research could maybe answer.
Finally, this case also raises many ethical questions. Firstly, concerning the subject, consequences of invalidating the diagnosis of schizophrenia would have many repercussions for him in his identity as a patient and in his whole life. The subject could lose his income from social benefits, and his housing which is granted to him thanks to the recognition of mental illness. This questions a hasty diagnosis, a risk of “over-medicalisation”, which seems to have locked the patient in a system with much assistance he is struggling to get rid of.
Secondly, for doctors, this case calls for caution with the need to take time for diagnosing and to try to perform a detailed clinical analysis. Indeed in the case, it seems that the subject’s symptoms were often interpreted to contribute to the diagnosis of schizophrenia. The advanced evaluation gave the time for detailed investigation, and fine analysis of the described symptoms. This is a reminder of the necessary watchfulness when evaluating patients and the interest of questioning diagnoses that have been established.
Lastly for society in France, this case leads to thinking in such a diagnosis opens rights to social benefits. Doctors therefore have a delicate responsibility towards society. To some extent, a wrongful diagnosis could be considered a prejudice for society. In this current case, the patient even suggested that during a certain period, the benefits he received financed his cannabis use. Doctors therefore have a responsibility towards society to make cautious diagnoses.
4. Conclusion
This case-report shows the importance of a cautious diagnosis when it comes to concomitant psychosis and cannabis use. The need for further research in this area is evident. Cannabis use seems to be rising all around the world. In many countries, its use is trivialized, in some, it is even, though sometimes controversially, legalised. Cases like this one are thus likely to become more frequent. The need for better distinction between cannabis-induced psychosis and schizophrenia is important to avoid misdiagnosis and provide the best care possible for patients. Guidelines for cannabis-induced psychosis need to see the light of day to provide suitable care in these cases and help medical decisions. Indeed, these diagnoses have significant consequences, which affect patients’ lives, but also impact society. Medical, ethical, and societal issues are at stake, which reinforces the need for further research.
Acknowledgments
The authors wish to thank their whole team for their input on this case, particularly Mr Sylvain Leignier, MD; Mrs Julie Monnais, resident in psychiatry with Mrs Zoé Boulot; Mrs Marie Abbes, Mrs Megane Faraldo, neuropsychologists, Msc, like Mr Franck Gabayet; Mrs Ingrid Arnaud and Mrs Delphine Hernandez, state-registered nurses like Mr Mathieu Besnard; Mr Raphaël Froger, health executive; Mr Thomas Cohen, clinical research associate; Mrs Joan Glorennec and Mrs Leïla Lemaire, medical assistants.
The authors also wish to thank the Direction of the hospital in the dynamics of research of the unit, in particular Mrs Véronique Bourrachot, Director of the psychiatric establishment, Mrs Giovanna Venturi-Maestri, President of the Medical Community and Mr Mustapha Bensaadi, Head of the Medical Pole. Finally, the authors wish to thank the patient, for his efforts and his sincerity, throughout the evaluation.
Funding
No special funding was received.
Disclosure and Conflict of Interests
None of the authors have any disclosures to make. The authors have no conflict of interests to declare.
References
- European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2021: Trends and Developments, Publications Office of the European Union, Luxembourg (2021).
- Hjorthøj C, Larsen M, Starzer M, et al. Annual incidence of cannabis-induced psychosis, other substance-induced psychoses and dually diagnosed schizophrenia and cannabis use disorder in Denmark from 1994 to 2016. Psychological Medicine 51 (2021): 617-622.
- Morrison P, Zois V, McKeown D, et al. The acute effects of synthetic intravenous Δ9-tetrahydrocannabinol on psychosis, mood and cognitive functioning. Psychological Medicine 39 (2009): 1607-1616.
- Marconi A, Di Forti M, Lewis CM, et al. Meta-analysis of the Association Between the Level of Cannabis Use and Risk of Psychosis. Schizophrenia Bulletin 42 (2016): 1262-1269.
- World Health Organization (WHO). International Classification of Diseases (ICD-10). Geneve (1993).
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders (DSM 5). Fifth Edition, American Psychiatric Association, Washington, D.C (2013).
- Power RA, Verweij KJH, Zuhair M, et al. Genetic predisposition to schizophrenia associated with increased use of cannabis. Molecular Psychiatry. 19 (2014): 1201-1204.
- Carey CE, Agrawal A, Bucholz KK, et al. Associations between Polygenic Risk for Psychiatric Disorders and Substance Involvement. Frontiers in Genetics 7 (2016): 149.
- Rentero D, Arias F, Sánchez-Romero S, et al. Cannabis-induced psychosis: clinical characteristics and its differentiation from schizophrenia with and without cannabis use. Adicciones 33 (2021): 95-108.
- Petrucci AS, LaFrance EM, Cuttler C. A Comprehensive Examination of the Links between Cannabis Use and Motivation. Subst Use Misuse 55 (2020): 1155-1164.
- Starzer MSK, Nordentoft M, Hjorthøj C. Rates and Predictors of Conversion to Schizophrenia or Bipolar Disorder Following Substance-Induced Psychosis. Am J Psychiatry 175 (2018): 343-350.
- Hui CLM, Lam BST, Lee EHM, et al. A systematic review of clinical guidelines on choice, dose, and duration of antipsychotics treatment in first- and multi-episode schizophrenia. International Review of Psychiatry 31 (2019): 441-459.
- Kay SR, Fiszbein A, Opfer LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia bulletin13 (1987): 261-276.
- Leucht S, Kane JM, Kissling W, et al. What does the PANSS mean? Schizophrenia Research 79 (2005): 231-238.
- Addington D, Addington J, Maticka-Tyndale E, et al. Reliability and validity of a depression rating scale for schizophrenics. Schizophrenia Research 6 (1992): 201-208.
- Large M, Sharma S, Compton MT, et al. Cannabis use and earlier onset of psychosis: a systematic meta-analysis. Archives of General Psychiatry 68 (2011): 555-561.