Prevalence of Major Amputation in COVID-19 Era Compared to Non-COVID-19 Era- A Descriptive Retrospective Single Centre Study
Article Information
Ahmed J1, Saha H2,*, Rouf MA3, Wadud MA4, Islam S5, Russel SMGS6
1Assistant Professor and Associate Consultant, Department of Vascular Surgery, Ibrahim Cardiac Hospital and Research Institute, Shahbag, Dhaka, Bangladesh
2Assistant Professor, Thoracic Surgery, Bangabandhu Sheikh Mujib Medical University, Shahbag, Dhaka, Bangladesh
3Associate Professor, Department of Surgery, Khwaja Yunus Ali Medical College and Hospital, Sirajgong, Bangladesh
4Associate Professor and Consultant, Department of Cardiac Surgery, Ibrahim Cardiac Hospital and Research Institute, Shahbag, Dhaka, Bangladesh
5Resident Medical Officer, Department of Vascular Surgery, Ibrahim Cardiac Hospital and Research Institute, Shahbag, Dhaka, Bangladsesh
6Associate Professor and HOD, Department of Vascular Surgery, Ibrahim Cardiac Hospital and Research Institute, Shahbag, Dhaka, Bangladesh
*Corresponding author: Jubayer Ahmed, Assistant Professor and Associate Consultant, Department of Vascular Surgery, Ibrahim Cardiac Hospital and Research Institute, Shahbag, Dhaka, Bangladesh
Received: 29 December 2021; Accepted: 11 January 2022; Published: 13 January 2022
Citation: Ahmed J, Saha H, Rouf MA, Wadud MA, Islam S, Russel SMGS. Prevalence of Major Amputation in COVID-19 Era Compared to Non-COVID-19 Era- A Descriptive Retrospective Single Centre Study. Fortune Journal of Health Sciences 5 (2022): 29-36
Share at FacebookAbstract
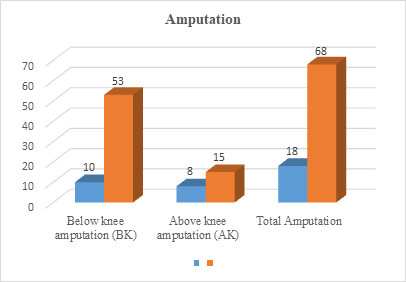
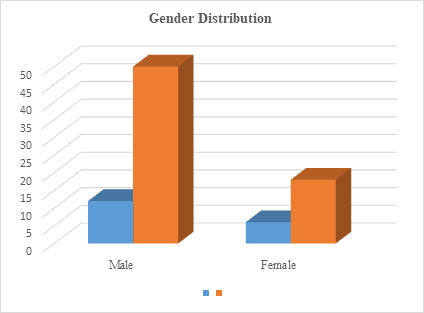
Introduction Amputation is the loss or removal of a body part such as a finger, toe, hand, foot, arm or leg. It can be a life changing experience affecting your ability to move, work, interact with others and maintain your independence. Continuing pain, phantom limb phenomena and emotional trauma can complicate recovery. Objective To assess the Prevalence of major amputation in covid-19 era compared to non-covid-19 era. Materials and Methods A descriptive Retrospective single Centre study was contacted in the Department Of Vascular Surgery, Ibrahim Cardiac Hospital And Research Institute, Shahbag, Dhaka, Bangladesh from Pre-pandemic era- 1st March 2018 to 3th August 2019: 18 months Group A and Pre-pandemic era- 1st March 2020 to 31th August 2021: 18 months Group B. We used the admission registers of all the hospital’s departments. We carried out a data collection sheet which allowed us to study the following parameters: the demographic aspects (age: according to WHO age groups and the sex of the patients), the type of amputation, the level of amputation and the causes. Results In the prepandemic phase, 18 major amputations were done (BK, 10 and AK, 8, and in the pandemic phase, 68 major amputations (BK, 53 and AK, 15) (P =.527) were undergone (fig-1). The age of the study participants in the prepandemic and pandemic period who had undergone a major amputation was 60.2 ± 13.4 and 62.88 ± 11.08 years (p=.241), respectively. The majority of the study participants were male in both the periods (prepandemic, M: F = 12:6; pandemic, M: F = 50:18) (P = .705). The mean duration of ulcer in the prepandemic period was 9 days and the same during the pandemic period was 10.8 days (P = .269). Co morbidities DM was present in 12(66.66%) study participants in the prepandemic and 40(58.82%) participants in the pandemic period (p=1.000). Diabetes Mellitus (DM) was present in 16 (88.88%) study participants in the prepandemic and 42(61.76%) participants in the pa
Keywords
Amputation, Gangrene, Lower Limb Amputation, Peripheral Arterial Occlusive Disease, Diabetes Mellitus
Article Details
1. Introduction
Amputation is the loss or removal of a body part such as a finger, toe, hand, foot, arm or leg. It can be a life changing experience affecting your ability to move, work, interact with others and maintain your independence. Continuing pain, phantom limb phenomena and emotional trauma can complicate recovery. Above-the-knee amputations are performed in patients of all ages for a variety of reasons. The amputation is performed through the femur and allows patients to use prosthesis for ambulation. This activity reviews the indications and techniques for above-the-knee amputations and highlights the role of the inter professional team in caring for patients who undergo this procedure [1]. A person can experience a traumatic amputation from a motor vehicle, occupational or industrial accident or combat injury. Traumatic injury accounts for about 45% of all amputations. A body part can be cut off or torn away in a severe accident, or it can be so badly damaged from a crush injury or severe burns that it cannot be saved. Above-the-knee amputations (AKA) involve removing the leg from the body by cutting through both the thigh tissue and femoral bone.
This procedure may be necessary for a wide variety of reasons, such as trauma, infection, tumor, and vascular compromise. There are several known physiologic and psychologic complications that are associated with this procedure. However, an inter professional approach to caring for these patients may decrease the rate of these complications. A below the knee amputation (BKA) is a transtibial amputation that involves removing the foot, ankle joint, distal tibia, fibula, and corresponding soft tissue structures. In general, below the knee amputations are associated with better functional outcomes than above the knee amputations. This activity describes the indications and technique for performing below the knee amputations and highlights the role of the inter professional team in the pre and post-operative management of patients undergoing this procedure [2]. A below-knee amputation (“BKA”) is a transtibial amputation that involves removing the foot, ankle joint, and distal tibia and fibula with related soft tissue structures. In general, a BKA is preferred over an above-knee amputation (AKA), as the former has better rehabilitation and functional outcomes.[3] The rates of lower extremity amputation have declined in recent years, but 3500 trauma-related amputations are still performed in the United States each year.[4] This surgical operation carries significant morbidity, yet it remains a treatment modality with vital clinical and often life-saving significance given appropriate indications [5, 6]. If tissue destruction, infection or disease affects a body part in a way that makes it impossible to repair or endangers the person’s life, that part may be removed by surgical amputation. Amputation of the extremity is one of the oldest surgical interventions that date back to the time of Hippocrates [7].
Amputation is not a failure of treatment rather it constitutes part of treatment when limb is not salvageable. It is indicated when the limb is not salvageable, it is dying or dead, it poses a threat to patients life, or it is viable but functionless [7, 8]. Lower limbs have loco motor function and functionless lower limb will interfere with employment of the patient. Dismemberment of the lower extremity has considerable economical, social and psychological impact on the patient and his family, but at the same time is a rehabilitative measure to improve patients’ quality of life [8, 9]. Lower limb amputation (LLA) can be major or minor. Major LLA is the one, which is performed at the level of the ankle or above [10]. The most common indication for LLA varies in different parts of the globe, however, trauma and peripheral vascular disease (PVD) including diabetic foot constitutes the major burden [11, 12].
2. Materials and Methods
A descriptive Retrospective single Centre study was contacted in the Department Of Vascular Surgery, Ibrahim Cardiac Hospital And Research Institute, Shahbag, Dhaka, Bangladesh from Pre-pandemic era- 1st March 2018 to 3th August 2019: 18 months Group A and Pre-pandemic era- 1st March 2020 to 31th August 2021: 18 months Group B. We used the admission registers of all the hospital’s departments. We also consulted the registers of the operating theatre and the staff of the Orthopaedic-Traumatology department (the only department that performs amputations). Thus, we were able to include all patients who had a major amputation (amputation site above the foot or hand) regardless of age or sex. We then consulted the patients’ files. We carried out a data collection sheet which allowed us to study the following parameters: the demographic aspects (age: according to WHO age groups and the sex of the patients), the type of amputation, the level of amputation and the causes.
2.1 Statistical Analysis
Collected data were entered in Microsoft Excel and the variables were coded. It was exported to IBM SPSS. Descriptive analysis was used to represent the data. Mean and standard deviation were used to represent the hospital stay, age of the study participants, duration of diabetes of the study participants, duration of ulcer, blood pressure (systolic and diastolic), estimated glomerular filtration rate (eGFR), glycosylated hemoglobin, and hemoglobin levels at the time of admission. Frequencies and percentages were used to represent the other parameters including number of BK amputations, AK amputations, gender, presence of complications, and history of previous surgeries. Wilcoxon signed-rank test was used as the data was non normal. IBM SPSS Version 20 was used.
3. Results
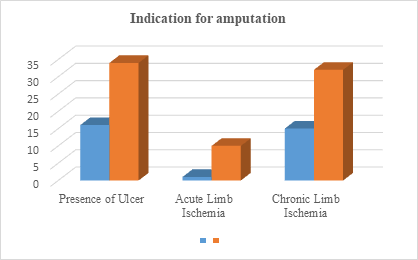
In the prepandemic phase, 18 major amputations were done (BK, 10 and AK, 8, and in the pandemic phase, 68 major amputations (BK, 53 and AK, 15) (P = .527) were undergone (fig-1). The age of the study participants in the prepandemic and pandemic period who had undergone a major amputation was 60.2 ± 13.4 and 62.88 ± 11.08 years (p=.241), respectively. The majority of the study participants were male in both the periods (prepandemic, M: F = 12:6; pandemic, M: F = 50:18) (P = .705) (Fig-2). There were no significant changes in the hospital stay during the prepandemic (9.3 ± 2.9) period and pandemic period admissions (9.1 ± 4) (P = .851). The mean duration of ulcer in the prepandemic period was 9 days and the same during the pandemic period was 10.8 days (P = .269). Co morbidities DM was present in 12(66.66%) study participants in the prepandemic and 40(58.82%) participants in the pandemic period (P = 1.000). Diabetes Mellitus (DM) was present in 16 (88.88%) study participants in the prepandemic and 42(61.76%) participants in the pandemic period (p= 1.000). HTN was noted in 8 (44.44%) study participants in the prepandemic and 32(47.05%) participants in the pandemic group (p=.705). CVD was present in 4(22.22%) study participants in the prepandemic and 10 (14.70%) in the pandemic group (p= 1.000). PAD was present in 16 (88.88%) and 38 (55.85%) study participants in the prepandemic and pandemic groups, respectively (p= .248). CKD was present in 4 (44.44%) and 12 (17.47%) study participants in the prepandemic and pandemic groups, respectively (p=1.000). The amputation rate in the prepandemic and pandemic phases was 4.48 per 1000 and 10.30 per 1000, respectively (Table-1). The above chart shows distribution of complications after amputation. Presence of Ulcer was present in 16 study participants in the prepandemic and 34 participants in the pandemic period (p=0.006*). Acute Limb Ischemia was present in 1 study participants in the prepandemic and 10 participants in the pandemic period (p = 1.000). Chronic Limb Ischemia was present in 15 study participants in the prepandemic and 32 participants in the pandemic period (p =1.000) (fig-3).
Table-1: Co-Morbidities prepandemic and pandemic period (N=86)
|
Group A |
Group B |
|
|
Smoker |
12 (66.66%) |
40 (58.82%) |
|
DM |
16 (88.88%) |
42 (61.76%) |
|
HTN |
8 (44.44%) |
32 (47.05%) |
|
CVD (Cerebrovascular disease) |
4 (22.22%) |
10 (14.70%) |
|
PAD (Peripheral vascular disease) |
16 (88.88%) |
38 (55.85%) |
|
CKD |
4 (44.44%) |
12 (17.47%) |
4. Discussion
In amputations, the indications are many and the pattern varies from place to place. The majority of the study participants were male. Males are at risk of trauma, especially in developing countries where male population work outside exposed to accidental hazards [13]. This resembles the study conducted by Caruso et al [13] which indicated increased diabetic foot problems during the pandemic in tertiary care settings. Among major amputations, BK amputations were higher in number than AK in both the pandemic and prepandemic groups. The overall prevalence of major amputations was higher during the pandemic lockdown compared to the prepandemic period. There was a 54.1% increase in major amputations noted. This might be due to the increased severity of diabetic foot infection in the pandemic period [14].
The reason might be the outcome of postponing the routine visit, improper diet, nonadherence to medications, and physical inactivity. Missed hospital visits or postponing the routine visit in this contest is defined as not visiting the physician as per the schedule, which is usually discussed in their previous visits as per the need/risk of the patient. High-risk patients are usually advised to visit their diabetologist and foot care specialists every 3 months. Improper diet can be defined as inconstant dietary habits in opposition to the advice of their physician/dietitian. In an online pilot survey, 20% of the study participants recorded they were not following the diet as before the lockdown [15]. No adherence to medications is not to take medicines as prescribed by the doctor. This no adherence can be intentional or no intentional. People with diabetes are advised to do minimal physical activity (30 min per day) in any form including walking, exercises, and yoga. Not doing the minimal physical activity to control the glycemic index is considered as physical inactivity. In terms of risk factors for diabetes-related amputations, glycemic control, peripheral neuropathy, and PAD are generally considered to play a vital role [16, 17]. A higher prevalence of PAD and peripheral neuropathy prevalence was noted in the study participants in the pandemic group than the prepandemic group. Practices like telemedicine were also practiced in this pandemic globally [18]. In addition to the teleconsultation, home visits by the podiatrists and/or the other paramedical staff were practiced.7 This combination of treatment in treating the wound can save the limbs and avoid the patients’ rush to emergency care at the 11th hour. Even though these services were available, they might not be affordable for all the patients who seek these services due to their socioeconomic status, especially in a developing country like India. During this pandemic, the low socioeconomic groups’ routine income was affected [19]. This might have worsened the condition. The presence of complications of diabetes, history of previous minor surgeries, eGFR, and presence of PAD were considered as risk factors for the major amputations [20]. Rate of amputation had increased twice in the pandemic period than in the prepandemic period. The number of major amputations decreased in the early pandemic period and progressed during the late pandemic period.
5. Conclusion
Number of major amputations increased a lot in COVID-19 era compared to non COVID-19 era due to lack of regular follow-up for this panic COVID situation. The prevalence of diabetes-related major amputations during the COVID-19 pandemic. From the results of this study, we observed there was a delay in seeking health care during the pandemic period when compared to the prepandemic period. And there was a notable increase in the number of major amputations. This study shows the indirect effect of the COVID-19 pandemic on people with diabetes, resulting in the increased prevalence of major amputations (BK and AK amputations) which might cause a drastic impact on their quality of life. Furthermore, these emphasize the need for easy and routine access to foot-care specialists to prevent avoidable amputations.
References
- Myers M, Chauvin BJ. Above the Knee Amputations. In: StatPearls [Internet]. Treasure Island (FL): Stat Pearls Publishing (2021).
- Adams CT, Lakra A. Below Knee Amputation. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2021).
- Pedersen HE. The problem of the geriatric amputee. Artif Limbs 1 (1968): 1-3
- Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J 95 (2002): 875-83.
- Penn-Barwell JG. Outcomes in lower limb amputation following trauma: a systematic review and meta-analysis. Injury 42 (2011): 1474-9.
- Narula N, Dannenberg AJ, Olin JW, Bhatt DL, Johnson KW, Nadkarni G, Min J, Torii S, Poojary P, Anand SS, Bax JJ, Yusuf S, Virmani R, Narula J. Pathology of Peripheral Artery Disease in Patients With Critical Limb Ischemia. J Am Coll Cardiol 72 (2018): 2152-2163.
- Atri A, Kocherlakota CM, Dasgupta R. Managing diabetic foot in times of COVID-19: time to put the best ‘foot’ forward. Int J Diabetes Dev Ctries 40 (2020): 321-328.
- Caruso P, Longo M, Signoriello S, et al. Diabetic foot problems during the COVID-19 pandemic in a tertiary care center: the emergency among the emergencies. Diabetes Care 43 (2020): e123-e124.
- Lancaster EM, Wu B, Iannuzzi J, et al. Impact of the COVID-19 pandemic on an academic vascular practice and a multi-disciplinary limb preservation program. J Vasc Surg 72 (2020): 1850-1855.
- Nachimuthu S, Vijayalakshmi R, Sudha M, Viswanathan V. Coping with diabetes during the COVID-19 lockdown in India: results of an online pilot survey. Diabetes Metab Syndr: Clin Res Rev 14 (2020): 579-582.
- Quilici M, Fiol F, Vieira A, Toledo M. Risk factors for foot amputation in patients hospitalized for diabetic foot infection. J Diabetes Res 2016 (2016): 1-8.
- Sadriwala Q, Gedam B, Akhtar M. Risk factors of amputation in diabetic foot infections. Int Surg J 5 (2018): 1399-1402.
- Caruso P, Longo M, Signoriello S, et al. Diabetic foot problems during the COVID-19 pandemic in a tertiary care center: the emergency among the emergencies. Diabetes Care 43 (2020): e123-e124.
- Lancaster EM, Wu B, Iannuzzi J, et al. Impact of the COVID-19 pandemic on an academic vascular practice and a multi-disciplinary limb preservation program. J Vasc Surg 72 (2020): 1850-1855.
- Nachimuthu S, Vijayalakshmi R, Sudha M, Viswanathan V. Coping with diabetes during the COVID-19 lockdown I India: results of an online pilot survey. Diabetes MetabSyndr: Clin Res Rev 14 (2020): 579-582.
- Quilici M, Fiol F, Vieira A, Toledo M. Risk factors for foot amputation in patients hospitalized for diabetic foot infection. J Diabetes Res 2016 (2016): 1-8.
- Sadriwala Q, Gedam B, Akhtar M. Risk factors of amputation in diabetic foot infections. Int Surg J 5 (2018): 1399-1402.
- Shin L, Bowling FL, Armstrong DG, Boulton AJM. Saving the diabetic foot during the COVID-19 pandemic: a tale of two cities. Diabetes Care 43 (2020): 1704-1709.
- Gopalan HS, Misra A. COVID-19 pandemic and challenges for socio-economic issues, healthcare and national health programs in India. Diabetes Metab Syndr: Clin Res Rev 14 (2020): 757-759.
- Shojaiefard A, Khorgami Z, Larijani B. Independent risk factors for amputation in diabetic foot. Int J Diabetes Dev Ctries 28 (2008): 32-37.