Prevalence of HIV in Different High-Risk Groups and Associated Risk Factors in Pakistan. A Systematic Review from 2010 to 2020
Article Information
Aswa Gondal1*, Mahrukh Rasheed2, Sana Ali3, Zain Ul Abdin4, Omar Rahim5, Shristee Ghimire6, Mohamed A Suleiman7, Relfa Dellanira Proano8, Ahmad Mashlah9, Olasumbo Elizabeth Fagbenle10, Jennifer Okon11, Sidra Shahid Mubasher12, Nabeel Hussain13, Asma Nasir14, Firas Kadurei15
1Rawal Institute of Health Sciences, Islamabad, Pakistan
2Dow University of Health and Sciences, Karachi, Pakistan
3Sheikh Zayed Medical College Rahim Yaar Khan, Rahim Yar Khan, Pakistan
4Punjab Medical College, Faisalabad, Pakistan
5Kabir Medical College, Peshawar, Pakistan
6University of Science and Technology Chittagong, Chittagong, Bangladesh
7IC laser Eye Care Ophthalmology, Philadelphia, USA
8Universidad de Guayaquil, Guayaquil, Ecuador
9Alfaisal University, Riyadh, Saudi Arabia
10Windsor University School of Medicine, Cayon, Saint Kitts and Nevis
11All Saints University College of Medicine, Arnos Vale, Saint Vincent and the Grenadines
12University Medical and Dental College, Faisalabad, Pakistan
13Saba University School of Medicine, Saba, Netherlands
14Dow University of Health Sciences, Karachi, Pakistan
15Mubarak Al-Kabeer Hospital, Jabriya, Kuwait
*Corresponding author: Aswa Gondal, Department of Internal Medicine, Rawal Institute of Health Sciences, Pakistan
Received: 06 September 2021; Accepted: 15 September 2021; Published: 27 September 2021
Citation:
Aswa Gondal, Mahrukh Rasheed, Sana Ali, Zain Ul Abdin, Omar Rahim, Shristee Ghimire, Mohamed A Suleiman, Relfa Dellanira Proano, Ahmad Mashlah, Olasumbo Elizabeth Fagbenle, Jennifer Okon, Sidra Shahid Mubasher, Nabeel Hussain, Asma Nasir, Firas Kadurei. Prevalence of HIV in Different High-Risk Groups and Associated Risk Factors in Pakistan. A Systematic Review from 2010 to 2020. Archives of Internal Medicine Research 4 (2021): 233-248.
Share at FacebookAbstract
Objective: HIV was diagnosed for the first time in Pakistan in 1987; since then, the prevalence has been gradually increasing and is expected to rise over the next decade. Although the epidemic has been predominantly concentrated in the high-risk groups, the concerning factors include spillover potential in the general population and multiple nosocomial infections. Therefore, we rooted the prevalence of HIV in the populations of Pakistan that were at higher risk and compared it with the prior estimates to guide future interventions.
Methods: We conducted a systematic review using keywords in PubMed, Google Scholar, and Pakimedinet.com to identify articles related to HIV frequency in Pakistan from January 1, 2010 to May 15, 2020. After reviewing the articles, 33 met the inclusion criteria for qualitative synthesis.
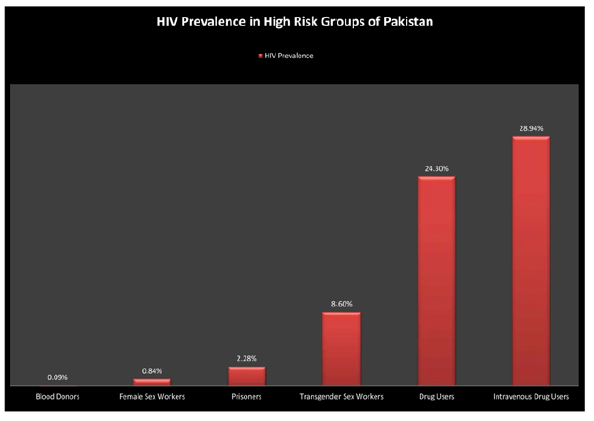
Results: Our results substantiated that the infection rate in blood donors was low yet on the rise with a numerical value of 0.09%. The analysis of high-risk groups estimated the highest infection rates of 28.94% in the intravenous drug users (IVDUs), followed by prisoners (2.28%) and sex workers (2.25%).
Conclusion: These estimates are considerably high compared to prior data on this topic and can cause devastating consequences for the population as a whole. Hence, urgent and effective interventions are required to reduce the frequency of HIV in high-risk groups and limit nosocomial epidemics.
Keywords
AIDS, Pakistan, Prevalence, Drug users, Sex workers
Article Details
1. Introduction
HIV has affected 36.7 million people globally and 2.1 million new cases are reported every year with a mortality rate of 1.1 million [1]. Pakistan has the fifth largest population in the world with over 200 million people [2] and reported its first case of HIV in 1987 [1]. According to the UNAIDS 2018 factsheet, 160,000 cases of HIV have been confirmed in Pakistan [3]. Historically, overall, HIV prevalence in Pakistan has remained low, and HIV cases have been predominantly concentrated in high-risk behavior groups, which include intravenous drug users (IVDUs), males who have sex with males (MSM), male, female, and transgender sex workers (TGSWs) and prisoners [4]. However, the incidence of HIV has been steadily rising over the last three decades and is projected to rise in the future as well [4]. The incidence of HIV is on the rise in Pakistan along with four other countries of Asia [4]. Pakistan experienced a 36.9% increase in deaths due to HIV in eight years from 2010 to 2018, while the incidence of new HIV infections also rose from 14000 to 22000 over the same period [5].
Another concerning factor is the escalating number of nosocomial HIV infections [6, 7]. In a recent outbreak in district Larkana of Sindh province between April and December 2019, Sindh AIDS Control Program identified 952 children with HIV [4]. In the last 20 years, there have been many flare-ups but this is the first outbreak that has predominantly affected children on such a large scale [6, 7]. It is thought that this outbreak was caused by poor transfusion practices and the reuse of needles by healthcare providers [8, 9]. Factors that are contributing to this rising trend of HIV include high levels of poverty, low literacy rate, lack of awareness among health care workers, and limited safety of blood transfusion [10-12]. An effective and efficient response is urgently required to downscale the number of new infections. In 2017, the Government of Pakistan coordinated the development of the AIDS epidemic model for Pakistan with the Global Fund's support to fight AIDS, tuberculosis (TB), and malaria (GFATM), the UNAIDS Country team, and the UNAIDS Regional Support team, Asia Pacific [13].
However, many more such efforts are required to curb the HIV epidemic. In the last three decades in Pakistan, multiple studies have reported HIV prevalence in different population cohorts. However, most of these studies had small patient population samples. Therefore, the purpose of this study was the assessment of HIV prevalence in Pakistan in critical populations and comparison with previous estimates. This will help us see the direction in which Pakistan is heading and help us make informed decisions about the future.
2. Material/Subjects/Patients and Methods
2.1 Search strategy and terms used
Our research team structured a comprehensive search strategy consisting of Mesh and keywords for a systematic review, to identify potential articles from January 2010 to May 2020 on HIV prevalence in Pakistan. The review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA guidelines). The search strategy was a combination of many different MeSH and key terms and included "Acquired Immunodeficiency Syndrome," "Pakistan," and different versions of the terms “HIV”, “HTLV-III Infection”, “Blood donors”, “sex workers” and “drug users”. Different online databases and sources like PubMed, Google Scholar and Pakmedinet.com were used during the search.
2.2 Inclusion and exclusion criteria
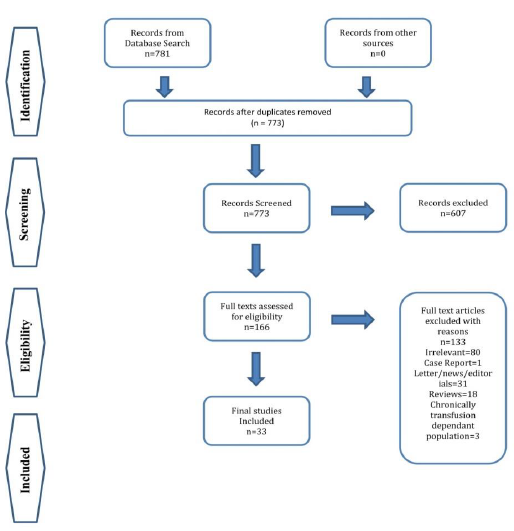
We identified a total of 781 articles initially and the number was reduced to 773 after the removal of duplicates. During the screening process of titles and abstracts by two independent reviewers, the articles fulfilling the inclusion criteria were included (between the assigned time frame of January 2010-May 2020, studies having more than 100 participants, reporting the prevalence of HIV in different high-risk cohorts of Pakistan, age≥18 years and original peer-reviewed articles in English language (Cross-sectional studies, case-control, prospective and retrospective cohorts). Articles were excluded if they were non-English, non-peer-reviewed, having less than 100 participants, population<18 years of age, and outside the assigned time frame. Reviews, editorial letters, case reports, correspondence, book chapters, and abstracts without full length were also excluded. Any conflict between the two reviewers was resolved either by discussion till a consensus or by an independent third reviewer.
2.3 Eligible studies
We imported a total of 781 studies in Bibliographic software (Endnote 8) and were left with 773 results after the duplicates were removed. After the review process, 166 studies were screened for full-length articles. We excluded 133 studies, as reported in the PRISMA diagram (Figure 1). A total of 33 studies were included in our review with 22 studies for the blood donors group, 3 for drug users, 5 for sex workers, and 3 for prisoners.
2.4 Data extraction
2 independent reviewers extracted the data from the full-lengths in an electronic spreadsheet for all the included articles. Different categories included study characteristics (lead author, year published, title of the article, DOI, database name, type of study), patient demographics (age, sex, sample size), high-risk group (IVDU, sex worker, prisoners), overall prevalence of HIV in the group and their associated risk factors. The extracted data was counter-checked by a third reviewer and discrepancies (if any) were resolved.
2.5 Data synthesis
Taking into account different risk factors and high-risk
groups, the diversity and cross-sectional nature of most of our included primary studies, a meta-analysis could not be performed to stay away from potentially deceptive conclusions.
3. Results
3.1 Overall HIV prevalence in pakistan
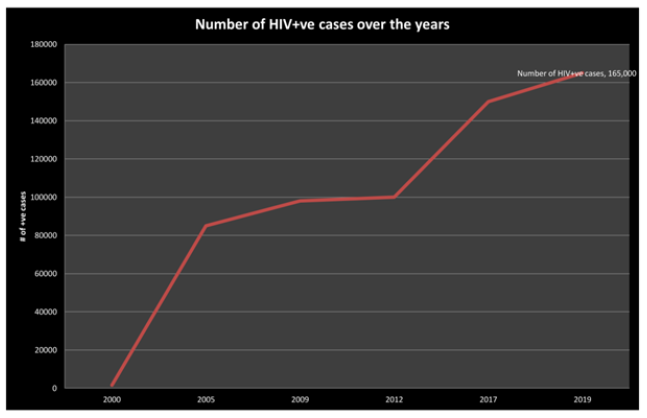
We reviewed a total of 33 studies and reported the prevalence of HIV in various high risk groups in Pakistan (Tables 1-4). These groups include blood donors, intravenous drug users, prisoners, and sex workers including male, female and transgender sex workers. Our analysis documents that cumulative prevalence of HIV in the country has steadily increased over the last two decades (Figure 2). In addition to cumulative prevalence, we also calculated the prevalence of HIV in different high-risk cohorts.
3.2 Blood donors
A total of 22 studies (6 studies from Islamabad, 7 from Punjab, 8 from Sindh and 2 from KP province) were included from 2010 to 2020 (Table 1). The studies reported 100% data from urban areas and mostly from provincial capitals. Chemiluminescent microparticle immunoassay (CMIA) was the most commonly used technique for the diagnosis of HIV (45.45% cases) followed by ELISA (22.7%). These studies reported the prevalence of HIV in blood donors and showed that 949 patients (0.09%) were positive for HIV.
3.3 Intravenous drug users
Three studies reported the frequency/prevalence of HIV in 1,228 drug users in Pakistan from 2010 to 2020 (Table 2). All three of these studies were conducted in big cities (1 in the Federal capital and 2 from Punjab province) and included 98% males. The mean age was 31.2 ± 8.95 years. Most of these people could not afford sufficient daily/monthly earnings and were poor (56.6%). An alarming 95.6% had a lack of information about hazards of needle sharing according to Samo et al. and accordingly, the prevalence of HIV was shocking (28.94%) in IVDUs. One study pointed out that sharing syringes, being homeless and daily frequency of injecting drugs were significantly associated with high risks of getting HIV infection. (p values <0.0001, 0.009 and 0.04 respectively). This epidemic in IVDUs is caused by diverse risk factors, including needle sharing and high-risk sexual practices.
3.4 Sex workers and the transgender community
Five studies reported the frequency of HIV in the sex workers group. Three out of these five reported female sex workers (FSWs), one study reported all male, female and transgender sex workers, and one study by Akhtar et al [14]. reported the data of only transgender sex workers population in Pakistan from 2010 to 2020 (Table 3). These studies collectively screened 13,984 persons with a mean age of 27.7 years. More than half of them were illiterate; more than half of FSWs and 18.3% trans-genders were married while they continued the sex work. FSWs entertained 2-3 clients per day and less than half of them (42.63%) were “always” doing safe sex practices (use of condoms) during the act. The rate of condom use was highest among the brothel-based FSWs and low among TGSWs and male sex workers. The overall prevalence among the sex workers group was calculated to be 2.25 % (315 patients). The isolated rates for FSWs and transgender sex workers are given in Figure 3. Although the rate of using intravenous drugs was calculated to be about 4.02%, having sex with IVDUs was calculated to be as high as 12.88 % and it can act as a bridge between the two high-risk groups. Almost all (99%) FSWs blamed economic instability for continuing this practice according to Khan et al [15]. The transgender sex worker population had an 8.60% prevalence rate with HIV-1 subtype as the predominant one, which was alarmingly high as compared to FSWs and was directly associated with little use of condoms, frequency of having unsafe sex (p=0.012), lack of knowledge and education (p=0.047 ) and sharing of razor blades for body shaving (p=0.092).
3.5 Prisoners
A total of 3 studies reported the frequency of HIV in inmates of Pakistan published between 2010 to 2020 (Table 4). All these studies collectively screened 2804 prisoners with 99 % males and a mean age of 27.3 years (range of 13-81 years). The results show that 64 prisoners (2.28%) were positive for HIV. The extramarital heterosexual sex rate was 43.7% and homosexual sex unpaid and paid was 22.7% among prisoners according to 2 studies. Only 9-25% of prisoners used condoms during the last sexual act according to one study. Needle sharing (21.42%) for IVDUs and sharing razor blades (22.91%) were also common practices among prisoners. CD4 count<500 was present in 2.8% patients and co-infections with Hepatitis C (50%), Hepatitis B (4.1%) and Tuberculosis (4.1%) were also seen.
|
Author, year (reference) |
Number of blood donors (n) |
Males |
Diagnostic method |
HIV prevalence N (%) |
|
Waheed et al., 2012 [16] |
10,145 |
NA |
ELISA |
0% |
|
Tufail et al., 2013 [17] |
1,833 |
NA |
CMIA |
3 (0.16%) |
|
Ghafoor et al., 2016 [18] |
1,500 |
94.67% |
ICT |
2 (0.13%) |
|
Waheed et al., 2016 [19] |
65,376 |
NA |
ELISA |
45 (0.06%) |
|
Sial et al., 2016 [20] |
29,522 |
90.40% |
CMIA |
20 (0.07%) |
|
Raza et al., 2016 [21] |
33,595 |
100% |
CMIA |
34 (0.10%) |
|
Niazi et al., 2016 [22] |
160,552 |
98.5% |
HIV antigen-antibody combination assay |
26 (0.02%) |
|
Memon et al., 2017 [23] |
4,683 |
NA |
CMIA |
3 (0.06%) |
|
Zameer et al., 2017 [24] |
10,048 |
100% |
ICT |
12 (0.11%) |
|
Arshad et al., 2016 [25] |
16,602 |
99.73% |
ELISA |
7 (0.04%) |
|
Attaullah et al., 2012 [26] |
127,828 |
99.96% |
ELISA |
77 (0.06%) |
|
Saeed et al., 2017 [27] |
18,274 |
99.32% |
ICT |
4 (0.02%) |
|
Awan et al., 2018 [28] |
30,470 |
62.2% |
HIV antigen-antibody combination assay |
49 (0.16%). |
|
Rauf et al., 2019 [29] |
6,594 |
99.97% |
CMIA |
12 (0.18%) |
|
Raza et al., 2018 [30] |
16,660 |
NA |
CMIA |
12 (0.07%) |
|
Sultan et al., 2017 [31] |
16,957 |
99.5% |
HIV antigen-antibody combination assay |
14 (0.08%) |
|
Irfan et al., 2013 [32] |
108,598 |
99.85% |
CMIA |
111 (0.10%) |
|
Sultan et al., 2016 [33] |
148,628 |
99.8% |
CMIA |
163 (0.11%) |
|
Azhar et al., 2018 [34] |
2,400 |
100% |
CMIA |
300 (12.5%) |
|
Batool et al., 2017 [35] |
41,033 |
98.3% |
CMIA |
28 (0.07%) |
|
Amin et al., 2017 [36] |
190 |
NA |
HIV antigen-antibody combination assay |
0% |
|
Zaheer et al., 2014 [37] |
160,376 |
99.62% |
ELISA |
27 (0.017%) |
|
Total: 1,011,864 |
Total: 949 (0.09%) |
Abbreviations: CMIA: chemiluminescent microparticle immunoassay, ELISA: enzyme-linked immunosorbent assay, ICT: immunochromatographic test
Table 1: Prevalence of HIV in blood donors.
|
Asif et al., 2019 [38] |
Samo et al., 2013 [39] |
Mansoor et al., 2014 [40] |
|
|
Total Drug users
|
Total: n= 402 IVDUs n=162 |
IVDUs: n=474 |
IVDUs: n=352 |
|
Mean age(years) |
32.2 ± 8.9 |
30.0 ± 9.0 |
NA |
|
Low socio- economic status |
n=343 -85.30% |
n=277 -58.40% |
n=75 -72% |
|
HIV prevalence |
Total=85/402 (21.1%) IVDUs n=72/162 (44.44%) |
n=118/474 (24.9%) |
n=96/352 -27.27% |
|
Currently sharing needles |
NA |
n=101 -21.30% |
NA |
|
Frequency of daily injection use(#/day) |
NA |
3.7 ± 1.4 |
NA |
|
Imprisonment History |
n=143 35.60% |
53.20% |
NA |
|
HIV Prevalence in Total drug users=24.3% |
HIV Prevalence in IVDUs=28.94% |
||
IVDUs= Intravenous Drug Users, NA=Not Available
Table 2: Prevalence of HIV in intravenous drug users.
|
Altaf et al., 2012 [41] |
Khan et al., 2011 [15] |
Mishra et al., 2012 [42] |
Akhtar et al.* 2012 [14] |
Melesse et al. 2016[43] |
|
|
Total Population |
FSWs n=1125 |
FSWs n=730 |
FSWs n=3340 |
TGSWs n=306 |
Total n=8483 FSWs=34.5% TGSWs=32.4% MSWs=33.1% |
|
Mean age(years) |
27.4 ± 6.7 |
30 |
26 |
29 |
26.3 ± 6.5 |
|
Clients or sex per unit time (day/ week/month) |
2.1 ± 1.2 clients/day |
3 clients/day |
50 clients/month |
1-40 times sex /week |
NA |
|
“Always” use condom |
n=31/50 (62%) Karachi n=22/40 (55%) Hyderabad |
n=471 (65%) |
n=1002 30.0% (26.6 to33.6) |
NA |
Overall n=3864 -45.55% FSWs= 53.47% TGSWs=31.87% MSWs=22.87% |
|
IVDUs among FSWs or TGSW |
n=zero |
n=3(0.4%) |
n=180 (5.4%) CI=(4.6 to 6.3) p<0.001 |
zero |
n=380 -4.48% |
|
Sex with IVDUs |
NA |
NA |
n=534/3332 (16.0%) p<0.001 |
NA |
n=988 -11.65% |
|
HIV prevalence |
Karachi n=3/400 (0.75%) 95 % CI 0.2-2.2%) Overall n=3/1125 -0.26% |
n=5/730 (0.7%) |
n=25/3340 (0.63%) 95% CI 0.43 to 0.92%) |
n=66 -21.60% (CI 0.17-0.26) |
Overall n=216(2.55%) (95% CI= 2.08–3.00) TGSWs =8.14% MSWs= 3.57% FSWs= 0.97% (P<0.01) |
*the included population is transgender community
FSWs=Female sex workers, TGSWs= Transgender sex workers, MSWs=Male sex workers
CI=confidence interval
Table 3: Prevalence of HIV in sex workers & trans genders.
|
Kazi et al., 2010 [44] |
Khan et al., 2018 [45] |
Wali et al., 2019 [46] |
|
|
Total population of inmates |
n=364 |
n=2084 |
Total participants=567 Inmates=356 |
|
Mean Age(years) |
27 (range 18–81) |
25 (range 13–80) |
30 (IQR: 21–37) |
|
Extramarital/paid sex |
n=166/362 (45.9%) |
n=38/104 (36.53%) 11 out of these 38 were HIV +ve (OR = 4.48) (95% CI 1.41–14.2) |
NA |
|
Homosexual/paid sex |
n= 77/362 -21.30% |
n=29/104 (27.88%) 7 out of these 29 were HIV +ve (OR= 2.09) (95% CI 0.69–6.28) |
NA |
|
Injection drug users (% from total drug users) |
n=50 /215 (23.3%) 95% CI 8.5–15.0 |
n=11/57 (19.29%) (OR=13) 95% CI 2.82–60.01) |
NA |
|
Needle sharing |
n=23/50 (46%) |
HIV+ve n= 08/16 (50%) HIV -ve n= 2/88 (2.3%) Overall n=10/104 (9.61%) OR=43 95% CI=7.77–237.87 |
NA |
|
Tattoos |
n= 91/364 -25% |
n= 7/104 (6.7%) 2 out of these 7 were HIV +ve |
NA |
|
Sharing/using of old razor blades |
n= 97/363 -26.70% |
n= 10/104 (9.61%) 3 out of these 10 were HIV +ve (OR=2.67) (95% CI=0.61–11.66) |
NA |
|
History of any surgical procedure |
n=143/363 -39.40% |
n= 13/104 (12.5%) OR=01 (95% CI=0.2–5.01) |
NA |
|
HIV prevalence |
n=7/364 (2.0%) (CI=0.6–3.4%) |
n=33/2084 (1.6%) |
n=24/356 (6.74%) |
OR=Odds Ratio, CI=confidence interval, IQR= Interquartile range
Table 4: Prevalence of HIV in prisoners.
4. Discussion
4.1 Overall HIV frequency in pakistan
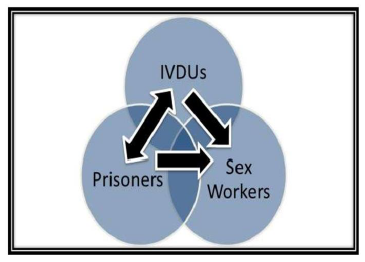
Altogether, we reviewed 33 studies and reported the prevalence of HIV in Pakistan (Figure 3). Previous data showed that Pakistan has low general population rates of HIV (<1/100,000); however, few populations have an increasingly concentrated epidemic. These cohorts include intravenous drug users, prisoners, and sex workers. Although these cohorts account for <2% of the general population (NACP 2008), they contribute to the rising overall prevalence of HIV. Only four countries in Asia have seen an increase in the incidence of HIV over the last decade, Pakistan is one of them (others are Afghanistan, Bangladesh, Philippines) [47]. Appro-ximately, 160,000 patients were positive for HIV in Pakistan in 2018 [5]. Most of these patients belong to high-risk groups such as IVDUs, prisoners, MSM, transgender people, and sex workers [47]. Our data shows an overall pooled HIV frequency of 0.157% in our study population. Prior work on this topic has reported a relatively low frequency. Ali, Nadeem, Numan, et al. [48] reported a frequency of 0.041% in their meta-analysis published in 2017 [48]. Possible reasons for this increase include the gradually increasing frequency of HIV among key populations in Pakistan, as documented by successive HIV surveillance surveys [49-52]. Moreover, evidence shows that these high-risk groups are interacting with each other and have the potential to cause HIV epidemic bridging [53]. Intravenous drug users mostly have criminal record/imprisonment history and sexual relations with both FSWs and TGSWs making them the cornerstone of bridging among the high-risk groups (Figure 4).
Furthermore, there have been multiple outbreaks in the general population in the last few years [6, 7, 54]. However, the large outbreak in 2019 in Larkana, Sindh, is the first outbreak that predominantly affected children [55, 56 ]. WHO identified a few potential means of HIV transmission such as risky blood donation and reuse of medical needles. Male circumcision with unhygienic blades, and ear and nose piercing with unsafe needles are also the potential causes of this outbreak [57]. It is also thought that the overall frequency of HIV is underreported in Pakistan [58].
4.2 Blood donors
Most of the papers in our analysis documented an overall HIV seroprevalence of < 0.1% [22, 23, 25-27, 59]. Other studies reported a seropre-valence of 0.1%-0.2% [18, 28, 31, 60] while a few studies reported no cases of HIV [4, 16, 36]. We compared cumulative percent HIV frequency in the healthy population (i.e., healthy blood donors) with high-risk groups. Our data documents that the frequency of HIV in healthy blood donors is 0.09%. Although this is low as compared to high-risk groups, it is gradually increasing. Ali et al. and colleagues performed a systematic review of HIV data of 30 years in Pakistan (1987–2017) and reported an HIV frequency of 0.012% in blood donors [48], which is relatively low compared with estimates in the current study. Furthermore, a few of the recent articles (2012–2017) reported relatively higher rates of HIV frequency in healthy blood donors [37, 59, 60]. This is an indication that the HIV frequency is gradually increasing in the country. A possible reason for this gradually increasing trend of HIV frequency in healthy donors includes an overall increase in HIV frequency in the general population secondary to the bridging of healthy populations with high-risk populations. Further-more, the blood transfusion system in Pakistan relies mainly on weakly regulated transfusion practices. This is especially true for small cities and remote rural areas and contributes to a steadily rising HIV prevalence in blood donors.
4.3 Drug users
0.7% of the total population (about 628,000) use opiates in Pakistan. Among them, 77% of individuals are heroin users, and 19% are IVDUs [28]. IVDUs account for the highest rate of HIV infections for any population group in Pakistan [49]. Pakistan has low general population rates of HIV, yet the frequency among IVDUs in Pakistan has remained persistently high. Our data documented an even higher frequency of HIV in IVDUs (28.94%) than in the previous studies. Ali, Nadeem, Numan, et al. [48] documented a frequency of 16.51% in IVDUs in their study published in 2017, which is considerably low compared to our data [48]. Similarly, UNAIDS reported a frequency of 21% in IVDUs in Pakistan in 2018 [5]. This upward trend is not only due to needle sharing but also because of high-risk sexual practices performed under the influence of these drugs and can lead to a high frequency in the general population through bridging contacts (Figure 4). As a large number of IVDUs have criminal records and previous imprisonment history, it can serve as a bridge between IVDUs and prisoners. Effective infection control measures like limiting reuse of needles and syringes, the introduction of auto-disable syringes in hospitals, opiate substitution therapy, testing, and availability of antiretroviral therapy, should be implemented to decrease the burden of HIV in this group.
4.4 Sex workers and the transgender community
Our data documented an overall frequency of 2.25% in sex workers in Pakistan. Ali, Nadeem, Numan, et al. [48] documented a frequency of 2.21% in sex workers in their analysis published in 2017 [48]. Although overall frequency among sex workers is not that high, our data documented extremely high frequency in the transgender population (8.60%). This is also considerably high compared to previous data, e.g., NACP (National AIDS Control Program) reported a frequency of 7.1% among the transgender population in 2016 [47]. Possible reasons for this high frequency in the transgender population could be attributed to low condom use, higher-risk sexual practices [47], sharing of razors for body shaving, and lack of access to proper knowledge. Furthermore, due to psychological and social stress, they are also at increased risk of developing drug dependence [48]. They are also involved in intravenous drug addiction and sex with IVDUs that also contribute to the cause.
Historically HIV rates among female sex workers have remained low in the country. All the studies in our data report a frequency of <1% in female sex workers. This low risk can be attributed to the fact that the majority of clients of these female sex workers do not belong to any of the high-risk groups and hence have a low HIV frequency [61]. Our data does not include any studies about HIV frequency exclusively for MSM. Limited data on this topic is the result of the limited acceptance of MSM in Pakistani society. Hence these people do not come forward and are reported as either heterosexual or transgender men [62]. Our data shows a considerable difference in HIV frequency rate among the transgender population and female sex workers. However, this is not conclusive and needs more elaborate research.
4.5 Prisoners
Prisons in developing countries are ideal incubators of
infectious diseases. Pakistan has about 90 prison cells, and Punjab Province has the highest number of prisoners [63]. The judicial system in Pakistan is poorly regulated, leading to lengthy trials and delays in convictions. This leads to overcrowded prisons with poor accommodation and medical facilities [64]. Most of the prisoners interact with the high-risk population (especially IVDUs), and most of them are drug users and/or sex workers, which could lead to high HIV frequency [65, 66]. Our data documented HIV frequency of 2.28% in prisoners. This is relatively high as compared to the previously reported data. Ali, Nadeem, Numan, et al. [48] documented a frequency of 1.32% in prisoners in their meta-analysis [48], which is considerably low compared to our data. This upward trend in HIV frequency in prisoners warrants immediate reforms in the judicial and prison system with the availability of better screening and medical services.
4.6 Recommendations
Our society as a whole needs to play a decisive role in uprooting this menace along with government and non-government organizations (NGOs). Adequate knowledge should be provided on HIV, its prevalence, risk factors, mode of transmission, and severity to the masses through proper media platforms (including social, print and electronic media). Transfusion practices should be properly regulated and auto-disable syringes be introduced in private and public health institutions all over the country. Proper medical waste management is also warranted in all healthcare centers to help curb this evil. Substitution therapy and rehabili-tation centers for drug users should be introduced in different regions throughout the country. Moreover, easy and cost-effective methods for diagnosis and management like anti-retroviral therapy should also be introduced along with special awareness programs aimed at every high-risk group. Special instructions regarding the role of sharing razor blades and HIV should be provided in prisons and among transgender communities. Job opportunities should be enhanced for the transgender and female population to substitute the sex work.
4.7 Limitations
Limitations of our study include lack of information/ studies from all over the country, especially avail-ability of data from rural areas. Many of the included studies were from a single-center and predominantly included males. The sample size was not significantly large enough in many studies. Further-more, we cannot estimate the prevalence definitively as people are reluctant to talk about sexual relationships due to social barriers. A large number of new prospective studies are required to fully assess how deep-rooted the menace of HIV is in the country and to inquire about the associated risk factors.
5. Conclusion
HIV frequency in Pakistan has gradually increased over the last two decades. Our data documents alarmingly uptrend HIV frequency in IVDUs, transgender populations, and prisoners. These high-risk groups and localized nosocomial epidemics can cause devastating consequences for the population as a whole. A national strategy must be adapted to implement an effective response to control the HIV epidemic in high-risk groups.
References
- Global HIV & AIDS statistics — Fact sheet. Unaids.org (2021).
- Population Census. Pakistan Bureau of Statistics (2021).
- Country Factsheet UNAIDS. Pakistan 2020. Unaids.org (2021).
- Mir F, Mahmood F, Siddiqui A, et al. HIV infection predominantly affecting children in Sindh, Pakistan, 2019: a cross-sectional study of an outbreak. The Lancet Infectious Diseases 20 (2020): 362-370.
- Country Fact sheets. Pakistan, Geneva, Switzerland: UNAIDS (2018).
- Wahid B. An update on the severe outbreak of HIV in Kot Imrana, Pakistan. Lancet Infect Dis 19 (2019): 241.
- Shah SA, Altaf A, Mujeeb SA, et al. An outbreak of HIV infection among injection drug users in a small town in Pakistan: potential for national implications. Int J STD AIDS 15 (2004): 209.
- Arif F. HIV crisis in Sindh, Pakistan: the tip of the iceberg. Lancet Infect Dis 19 (2019): 695-696.
- Altaf A, Iqbal S, Shah SA. A third major human immunodeficiency viruses (HIV) outbreak in Larkana, Pakistan: caused by unsafe injection practices. J Pak Med Assoc 69 (2019): 1068-1069.
- UNAIDS Country Profile (2005).
- WHO Epidemiological Fact Sheet (2005).
- HIV and AIDS in Pakistan, HIV in Pakistan, AIDS in Pakistan, Indicators, Estimates, Figures, HIV situation (2005).
- National AIDS Control Programme, Ministry of National Health Services, Regulations & Coordination (2017).
- Akhtar H, Badshah Y, Akhtar S, et al. Prevalence of human immunodeficiency virus infection among transgender men in Rawalp-indi (Pakistan). Virology journal 9 (2012): 1-9.
- Khan MS, Unemo M, Zaman S, et al. HIV, STI prevalence and risk behaviours among women selling sex in Lahore, Pakistan. BMC infectious diseases 11 (2011): 119.
- Waheed U, Khan H, Satti HS, et al. Prevalence of transfusion transmitted infections among blood donors of a teaching hospital in Islama-bad. Ann Pak Inst Med Sci 8 (2012): 236-239.
- Tufail S. Blood donors deferral-Causes. Journal of Rawalpindi Medical College 17 (2013): 119-121.
- Ghafoor Muhammad, Hussain M, Leghari AR, et al. Major Transfusion-Transmissible Infections Among Blood Donors In Rahim Yar Khan, A District Of Southern Punjab, Pakistan. Isra Medical Journal 8 (2016): 246-248.
- Waheed U, Hasan SI, Wazeer A, et al. The status of blood safety in Islamabad, Pakistan. Ann. Pak. Inst. Med. Sci 12 (2016): 209-214.
- Sial GR, Khan S, Shahid SU, et al. Prevalence Of Transfusion Transmitted Infections In Asymptomatic Blood Donors: Is Syphilis Alarming?. Biomedica 32 (2016).
- Raza N. Revisiting Reactive Blood Donor Demographics - A Single Center Experience. J Liaquat Uni Med Health Sci 15 (2016): 208-212.
- Niazi SK, Mahmood A, Alam M, et al. Seroprevalence of transfusion transmissible infections in blood donors: A three year experience. Pakistan Armed Forces Medical Journal 66 (2016): 190-193.
- Memon FA, Ujjan ID, Memon AI, et al. Seroprevalence of transfusion transmitted infections among different blood group donors at Blood Bank LUMHS, Hyderabad. Pak J Med Sci 33 (2017): 443-446.
- Zameer M, Shahzad F, Khan FS, et al. Transfusion transmissible infections among healthy blood donors at blood bank from children's hospital & institute of child health Lahore. Pakistan Armed Forces Medical Journal 1 (2017): 131.
- Arshad A, Borhany M, Anwar N, et al. Prevalence of transfusion transmissible infections in blood donors of Pakistan. BMC hematology 16 (2016): 27.
- Attaullah S, Khan S, Khan J. Trend of transfusion transmitted infections prevalence in blood donors: provide a road map for its prevention and control. Journal of translational medicine 10 (2012): 1-5.
- Saeed M, Hussain S, Rasheed F, et al. Silent killers: Transfusion transmissible infections-TTI, among asymptomatic population of Pakistan. J Pak Med Assoc 67 (2017): 369-374.
- Awan S A, Junaid A, Sheikh S. Transfusion Transmissible Infections: Maximizing Donor Surveillance. Cureus 10 (2018): e3787.
- Rauf R, Cheema A. Potential risk of transfusion-transmissible infections among blood donors in district Faisalabad of Pakistan. Clin Med 19 (2019): s27.
- Raza N, Qureshi H, Qureshi A. Reactive blood donor notification; their responses and perceptions: Experience from southern Pakistan. J Ayub Med Coll Abbottabad 30 (2018): 351-355.
- Sultan S, Nasir MI, Rafiq S, et al. Multiplex real-time RT-PCR assay for transfusion transmitted viruses in sero-negative allogeneic blood donors: an experience from Southern Pakistan. The Malaysian Journal of Pathology 39 (2017): 149-154.
- Irfan SM, Uddin J, Zaheer HA, et al. Trends in transfusion transmitted infections among replacement blood donors in Karachi, Pakistan. Turkish Journal of Hematology 30 (2013): 163-167.
- Sultan S, Murad S, Irfan SM, et al. Trends of venereal infections among healthy blood donors at Karachi. Arch Iran Med 19 (2016): 192-196.
- Azhar S, Iftikhar M, Usman M, et al. Epidemiological Study of Seropositive Infection HBV, HCV and HIV in Male healthy blood donors of Gadap Town, Karachi. P J M H S 12 (2018).
- Batool Z, Durrani SH, Tariq S. Association of ABO and Rh blood group types to hepatitis B, hepatitis C, HIV and Syphillis infection, a five year’experience in healthy blood donors in a tertiary care hospital. Journal of Ayub Medical College Abbottabad 29 (2017): 90-92.
- Amin F, Zafar A, Chattha HA. Prevalence of Hepatitis B, C & HIV among Blood Donors in Blood Bank of Lahore General Hospital, Lahore. PJMHS 11 (2017): 878-880.
- Zaheer H, Saeed U, Waheed Y, et al. Prevalence and trends of Hepatitis B, Hepatitis C and human immunodeficiency viruses among blood donors in Islamabad, Pakistan 2005–2013. J. Blood Disorders Transf 5 (2014): 1000217.
- Asif A, Ayub S, Komal A, et al. Prevalence of human immunodeficiency virus and Hepatitis (B & C) among drug users in a tertiary care public hospital. Pak J Med Sci 35 (2019): 459-463.
- Samo RN, Altaf A, Agha A, et al. High HIV Incidence among Persons Who Inject Drugs in Pakistan: Greater Risk with Needle Sharing and Injecting Frequently among the Homeless. PLoS ONE 8 (2013): e81715.
- Mansoor SA, Muazzam M, Imam HSH. HIV infection; prevalence among intravenous drug users. Professional Med J 21 (2014): 975-979.
- Altaf A, Agha A, McKinzie MH, et al. Size estimation, HIV prevalence and risk behaviours of female sex workers in Pakistan. JPMA-Journal of the Pakistan Medical Association 62 (2012): 551.
- Mishra S, Thompson LH, Sonia A, et al. Sexual behaviour, structural vulnerabilities and HIV prevalence among female sex workers in Pakistan. Sexually transmitted infections 89 (2013): 34-42.
- Melesse D, Shafer L, Shaw S, et al. Heterogeneity Among Sex Workers in Overlapping HIV Risk Interactions With People Who Inject Drugs. Medicine 95 (2016): e3085.
- Kazi AM, Shah SA, Jenkins CA, et al. Risk factors and prevalence of tuberculosis, human immunodeficiency virus, syphilis, hepatitis B virus, and hepatitis C virus among prisoners in Pakistan. International Journal of Infectious Diseases 14 (2010): e60-e66.
- Khan MD, Wali A, Fatima R et al. Prevalence and associated risk factors of HIV in prisons in Balochistan, Pakistan: a cross-sectional study. F1000Research 7 (2018): 1821.
- Wali A, Khan D, Safdar N, et al. Prevalence of tuberculosis, HIV/AIDS, and hepatitis; in a prison of Balochistan: a cross-sectional survey. BMC public health 19 (2019): 1-8.
- National AIDS Control Program Pakistan. Integrated biological and behavioral surveillance in Pakistan 2016-2017 (2018).
- Ali M, Nadeem M, Numan M, et al. Thirty years of HIV in Pakistan: a systematic review of prevalence and current scenario. Future Virol 12 (2017): 609-623.
- National AIDS Control Program. HIV second generation surveillance in Pakistan: national report round II 2006-2007. Islamabad, Pakistan (2007).
- National AIDS Control Program. HIV second generation surveillance in Pakistan: national report round III, 2008. Islamabad, Pakistan (2008).
- National AIDS Control Program. HIV second generation surveillance in Pakistan: national report round IV, 2013. Islamabad, Pakistan (2013).
- National AIDS Control Program. Progress report on the Declaration of commitment on HIV/AIDS for the United nations General assembly special session on HIV/AIDS. Islamabad, Pakistan (2010).
- Khanani MR, Somani M, Rehmani SS, et al. The spread of HIV in Pakistan: bridging of the epidemic between populations. PLoS One 6 (2011): e22449.
- Altaf A, Pasha S, Vermund SH, et al. A second major HIV outbreak in Larkana, Pakistan. J Pak Med Assoc 66 (2016): 1510-1511.
- Ansari JA, Salman M, Safdar RM, et al. HIV/AIDS outbreak investigation in Jalalpur Jattan (JPJ), Gujrat, Pakistan. J Epidemiol Glob Health 3 (2013): 261-268.
- Zaid M, Afzal MS. HIV outbreak in Pakistan. Lancet Infect Dis 18 (2018): 601.9
- Waqar Bhatti M. WHO declares HIV outbreak in Larkana as ‘Grade 2 Emergency’. The News International (2019).
- Altaf A. Delays and gaps in HIV programmes in Pakistan. Lancet HIV 5 (2018): e678-e679.
- Batool Z, Durrani SH, Tariq S. Association of Abo and Rh blood group types to hepatitis B, hepatitis C, HIV and syphilis infection, A five year’ experience in healthy blood donors in A tertiary care hospital. J Ayub Med Coll Abbottabad 29 (2017): 90-92.
- Irfan SM, Uddin J, Zaheer HA, et al. Trends in transfusion transmitted infections among replacement blood donors in Karachi, Pakistan. Turkish J. Hematol 30 (2013): 163-167.
- Singh S, Ambrosio M, Semini I, et al. Revitalizing the HIV response in Pakistan: A systematic review and policy implications. International Journal of Drug Policy 25 (2014): 26-33.
- Altaf A, Abbas S, Zaheer HA. Men who have sex with men: new emerging threat of HIV/AIDS spread in Pakistan. JPMA 58 (2008): 419-420.
- Malik M, Shirazi RA. An analytical review of juvenile delinquents in jails of Sindh province: some problems and suggestions to overcome. Indus J. Manage. Soc. Sci 4 (2010): 43-54.
- Safi SZ. Seroprevalence of hepatitis C and human immunodeficiency viruses in blood donors of northwestern Pakistan. Asian Biomed 5 (2011): 389.
- Khan Z, Raziq F, Aslam N. Prevalence of HIV in blood donors in NWFP. JPMI 16 (2011): 1-4.
- Shah S, Ehsan A. Seroprevalence of surrogate markers for hepatitis B, hepatitis C and HIV in healthy blood donors at Shaikh Zayed Medical Complex, Lahore. Annals KEMU 15 (2010): 5-10.