Presumed Giant Cell Arteritis presenting as Sequential Bilateral 6th Nerve Palsies: Case Report and Review of Literature
Article Information
Mustafa Al-Chalabi1*, Meghana Ranabothu2, Nameer Aladamat1, Khaled Gharaibeh1, Ajaz Sheikh1,2
1Department of Neurology, University of Toledo, Toledo, OH, USA
2College of Medicine and Life Sciences, University of Toledo, OH, USA
*Corresponding Author: Mustafa Al-Chalabi, DO, Department of Neurology, University of Toledo, 2130 W Central Ave, Toledo, Ohio, USA.
Received: 15 August 2022; Accepted: 29 August 2022; Published: 07 September 2022
Citation: Mustafa Al-Chalabi, Meghana Ranabothu, Nameer Aladamat, Khaled Gharaibeh, Ajaz Sheikh. Presumed Giant Cell Arteritis presenting as Sequential Bilateral 6th Nerve Palsies: Case Report and Review of Literature. Fortune Journal of Rheumatology 4 (2022): 14-16.
Share at FacebookAbstract
Giant CELL ARTERITIS (GCA) is a systemic autoimmune disease that classically presents with jaw claudication, temporal headache and transient visual loss, affecting mostly people above the age of 50 years. However, diplopia due to cranial nerve 6 palsy (CN VI) has been rarely reported in GCA. Moreover, bilateral CN VI palsies, occurring in a sequential fashion in GCA is exceedingly rare. We report a case of a 70-year-old man who was admitted to our hospital twice within the span of one month with persistent binocular diplopia due to sequential, bilateral, CN VI palsies (right followed by left CN VI palsy) with associated eye pain, temporal headache, malaise and joint pain. The inflammatory markers including Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) were elevated at both admissions. He was treated with intravenous steroids with a complete resolution of his binocular diplopia, eye pain and temporal headache. Despite a negative biopsy of the temporal artery for evidence of inflammation, he was diagnosed with GCA by rheumatology, considering the fact that GCA pathology may have a patchy distribution, and a negative biopsy does not rule it out absolutely. This case underscores the importance of recognizing GCA as a differential diagnosis in patients presenting with binocular diplopia.
Keywords
Arteritis; Vessels; Steroids; Rheumatology; Neuropathy
Arteritis articles; Vessels articles; Steroids articles; Rheumatology articles; Neuropathy articles
Arteritis articles Arteritis Research articles Arteritis review articles Arteritis PubMed articles Arteritis PubMed Central articles Arteritis 2023 articles Arteritis 2024 articles Arteritis Scopus articles Arteritis impact factor journals Arteritis Scopus journals Arteritis PubMed journals Arteritis medical journals Arteritis free journals Arteritis best journals Arteritis top journals Arteritis free medical journals Arteritis famous journals Arteritis Google Scholar indexed journals Vessels articles Vessels Research articles Vessels review articles Vessels PubMed articles Vessels PubMed Central articles Vessels 2023 articles Vessels 2024 articles Vessels Scopus articles Vessels impact factor journals Vessels Scopus journals Vessels PubMed journals Vessels medical journals Vessels free journals Vessels best journals Vessels top journals Vessels free medical journals Vessels famous journals Vessels Google Scholar indexed journals Steroids articles Steroids Research articles Steroids review articles Steroids PubMed articles Steroids PubMed Central articles Steroids 2023 articles Steroids 2024 articles Steroids Scopus articles Steroids impact factor journals Steroids Scopus journals Steroids PubMed journals Steroids medical journals Steroids free journals Steroids best journals Steroids top journals Steroids free medical journals Steroids famous journals Steroids Google Scholar indexed journals Rheumatology articles Rheumatology Research articles Rheumatology review articles Rheumatology PubMed articles Rheumatology PubMed Central articles Rheumatology 2023 articles Rheumatology 2024 articles Rheumatology Scopus articles Rheumatology impact factor journals Rheumatology Scopus journals Rheumatology PubMed journals Rheumatology medical journals Rheumatology free journals Rheumatology best journals Rheumatology top journals Rheumatology free medical journals Rheumatology famous journals Rheumatology Google Scholar indexed journals Neuropathy articles Neuropathy Research articles Neuropathy review articles Neuropathy PubMed articles Neuropathy PubMed Central articles Neuropathy 2023 articles Neuropathy 2024 articles Neuropathy Scopus articles Neuropathy impact factor journals Neuropathy Scopus journals Neuropathy PubMed journals Neuropathy medical journals Neuropathy free journals Neuropathy best journals Neuropathy top journals Neuropathy free medical journals Neuropathy famous journals Neuropathy Google Scholar indexed journals vasculitis articles vasculitis Research articles vasculitis review articles vasculitis PubMed articles vasculitis PubMed Central articles vasculitis 2023 articles vasculitis 2024 articles vasculitis Scopus articles vasculitis impact factor journals vasculitis Scopus journals vasculitis PubMed journals vasculitis medical journals vasculitis free journals vasculitis best journals vasculitis top journals vasculitis free medical journals vasculitis famous journals vasculitis Google Scholar indexed journals jaw claudication articles jaw claudication Research articles jaw claudication review articles jaw claudication PubMed articles jaw claudication PubMed Central articles jaw claudication 2023 articles jaw claudication 2024 articles jaw claudication Scopus articles jaw claudication impact factor journals jaw claudication Scopus journals jaw claudication PubMed journals jaw claudication medical journals jaw claudication free journals jaw claudication best journals jaw claudication top journals jaw claudication free medical journals jaw claudication famous journals jaw claudication Google Scholar indexed journals Erythrocyte Sedimentation Rate articles Erythrocyte Sedimentation Rate Research articles Erythrocyte Sedimentation Rate review articles Erythrocyte Sedimentation Rate PubMed articles Erythrocyte Sedimentation Rate PubMed Central articles Erythrocyte Sedimentation Rate 2023 articles Erythrocyte Sedimentation Rate 2024 articles Erythrocyte Sedimentation Rate Scopus articles Erythrocyte Sedimentation Rate impact factor journals Erythrocyte Sedimentation Rate Scopus journals Erythrocyte Sedimentation Rate PubMed journals Erythrocyte Sedimentation Rate medical journals Erythrocyte Sedimentation Rate free journals Erythrocyte Sedimentation Rate best journals Erythrocyte Sedimentation Rate top journals Erythrocyte Sedimentation Rate free medical journals Erythrocyte Sedimentation Rate famous journals Erythrocyte Sedimentation Rate Google Scholar indexed journals binocular diplopia articles binocular diplopia Research articles binocular diplopia review articles binocular diplopia PubMed articles binocular diplopia PubMed Central articles binocular diplopia 2023 articles binocular diplopia 2024 articles binocular diplopia Scopus articles binocular diplopia impact factor journals binocular diplopia Scopus journals binocular diplopia PubMed journals binocular diplopia medical journals binocular diplopia free journals binocular diplopia best journals binocular diplopia top journals binocular diplopia free medical journals binocular diplopia famous journals binocular diplopia Google Scholar indexed journals intravenous steroids articles intravenous steroids Research articles intravenous steroids review articles intravenous steroids PubMed articles intravenous steroids PubMed Central articles intravenous steroids 2023 articles intravenous steroids 2024 articles intravenous steroids Scopus articles intravenous steroids impact factor journals intravenous steroids Scopus journals intravenous steroids PubMed journals intravenous steroids medical journals intravenous steroids free journals intravenous steroids best journals intravenous steroids top journals intravenous steroids free medical journals intravenous steroids famous journals intravenous steroids Google Scholar indexed journals
Article Details
1. Introduction
Giant Cell Arteritis (GCA) is the most common type of vasculitis in large sized vessels. It primarily targets the tunica adventitia and media of arteries, such as branches of the ophthalmic artery [1]. If GCA is not identified and treated promptly, adverse effects such as ischemia of the visual pathways can occur, causing monocular or bilateral vision loss [2]. Other ophthalmic symptoms that can occur include ptosis, proptosis, eye pain, and diplopia. Sixth nerve palsy is one of the most common causes of diplopia [3]. However, CN VI palsy as a presenting manifestation of GCA is rare. There is growing data regarding the involvement of multiple cranial nerves in GCA, and CN VI palsies is one of them. Herein, we report a rare case of a patient, who presented with binocular diplopia due to sequential bilateral CN VI palsies and was eventually diagnosed by rheumatology with presumed GCA, based on his clinical picture, raised inflammatory markers and resolution of symptoms after receiving steroids.
2. Case Description
Our patient is a 70-year-old man, who presented with a five-day history of binocular diplopia. Diplopia was horizontal, and worse in right. He also had associated right periorbital and temporal pain. He further gave a history of malaise and joint pain mostly in the neck, knees and wrists for a month prior to his presentation. His past medical history was significant for type 1 diabetes (last A1C 8.1 mg/dL and presenting blood glucose 115 mg/dL), hypertension, hyperlipidemia, and deep vein thrombosis. Neurological examination showed complete right CN VI palsy, with restriction of right eye abduction on horizontal gaze testing. Rest of the neurological exam, including fundoscopy was normal. Computer Tomography (CT) of the brain was unremarkable. Magnetic resonance imaging (MRI) of the brain showed non-specific tortuosity of the optic nerves bilaterally raising suspicion for idiopathic intracranial hypertension. There were no areas of restricted diffusion on MRI. Magnetic resonance angiogram and venogram of head were normal. ESR was 79 mm/h (normal <20) and CRP was 7.7 mg/l (normal <0.8). The impression at this point was right CN VI palsy, likely secondary to a microvascular ischemic infract, given his elevated hemoglobin A1C, and hence a full stroke workup was instituted. The workup revealed a normal Low-Density Lipoprotein (LDL) of 56 mg/dl, and normal transthoracic echocardiogram (including ejection fraction and the left atrial size). He had a complete resolution of diplopia, along with total resolution of horizontal gaze restriction, 2 days after admission, and was therefore discharged home. The final impression at that time was transient right CN VI palsy due to microvascular ischemia, given his stroke risk factors. However, this did not explain the spontaneous resolution of the diplopia, nor the elevated inflammatory markers.
Three weeks later, he presented again with binocular diplopia with associated bitemporal headache and left eye pain and conjunctival injection. This time, however, the examination demonstrated bilateral CN VI palsies, left worse than right. Again, there were no other neurological findings on examination except for mild bilateral temporal tenderness. Repeat brain MRI continued to show nonspecific bilateral optic nerve tortuosity. ESR and CRP were persistently elevated at 92 mm/h and 12.2 mg/l respectively. Due to the MRI findings, lumbar puncture was performed and showed opening pressure of 16 cm H2O. He was evaluated by rheumatology, who strongly suspected giant cell arteritis. Therefore, he was started on a three-day course of methylprednisolone 1000mg daily. His diplopia, headache and eye pain resolved completely by the third dose of steroid. He underwent a bilateral temporal artery biopsy, which was negative for signs of active inflammation, including giant cell formation, but pathology report noted that healed arteritis could not be excluded. He was followed by rheumatology throughout his hospital course and their final impression was biopsy-negative giant cell arteritis. The negative biopsy was supposed to be due to patchy nature of the disease, and administration of steroids prior to biopsy, which could have potentially altered the biopsy results. The patient was then discharged on oral prednisone and continued to be free of diplopia and headache at his 2 months follow-up.
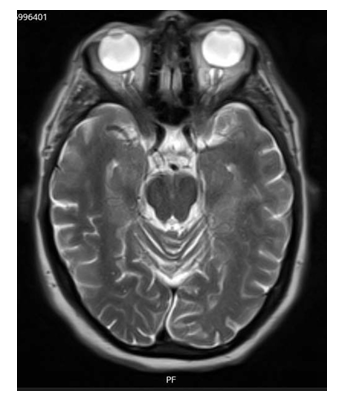
Figure 1: A T2 sequence of brain MRI demonstrates bilateral optic nerves tortuosity with no features of optic or preoptic sheath enhancement or flattening of the globes.
3. Discussion
Although a temporal artery biopsy was negative for giant cell formation in this case, we cannot completely rule out GCA, as steroids were used before the biopsy, and diplopia caused by cranial nerve palsies has been noted in this condition. ESR, the most important test to indicate inflammation, and CRP can be both elevated in GCA [7]. The fact that our patient was over 50 years of age, and had a new-onset headache, in presence of elevated ESR and CRP, were all strongly suggestive of diagnosis of GCA. In addition, 19% of patients whose temporal artery biopsy is negative for giant cell formation develop GCA later on [13]. Our case emphasizes the fact that diplopia due to bilateral CN VI palsies may occur in GCA. GCA mainly affects large arteries, including intracranial vasculature, and multiple cranial nerve palsies, although rare, have been and reported. In a case report two patients were described presenting with multiple cranial neuropathies due to GCA. One patient with cranial neuropathies involving CN III, IV & VI demonstrated active arteritis on temporal artery biopsy, while the other patient had involvement of CN III, V and VI, with temporal artery biopsy showing thickening and multinucleated giant cells [4]. In another case report, a patient with GCA had CN III, VIII and X palsies without the presence of typical giant cells [5]. All the patients showed resolution of some of their symptoms after receiving intravenous steroids followed by oral prednisone, potentially suggesting cranial nerve palsies in GCA can improve with the use of steroids. In addition, when multiple cranial nerves are affected in GCA, CN III commonly affected [4, 5, 9]. However, in our case, although more than one cranial nerve was affected, the pattern was bilateral, sequential CN VI involvement, with sparing of CN III, and symptoms completely resolved with the use of steroids.
GCA has many ophthalmic and neurologic manifestations, including headache, pain in the eye, jaw or temporal region, and myalgias [9]. Patients with GCA can present with vision loss that is serious, sudden, or sequential, where the other eye gets affected days to weeks after the initial eye [10]. It is usually the first manifestation of the condition, often permanent, and unlike diplopia, may not improve with the use of steroids [8, 12]. Diplopia secondary to CN VI palsy should always be considered as a clinical possibility in patients with GCA. In a retrospective and multicenter analysis, 10 of the 19 GCA patients who had constant diplopia had CN VI palsy [6]. Moreover, in two case reports, patients with CN VI palsy had diplopia [7,9], suggesting that there is a likely association. Our patient was atypical in that he developed horizontal-gaze diplopia to either side, after sequential bilateral CN VI palsy. Therefore, atypical manifestations of GCA, such as binocular diplopia, are important considerations for diagnosis of this disease. GCA due to specifically CN VI palsy is rare, as it usually occurs due to ocular ischemic manifestations, such as Anterior Ischemic Optic Neuropathy (AION), Posterior Ischemic Optic Neuropathy (PION), and central retinal artery occlusion (CRAO) [12]. In a case series study, out of the 36 patients who had systemic GCA, only 1 had isolated CN VI palsy and no ocular ischemic manifestations, whereas 17 patients had AION, 2 patients had CRAO, and 1 patient had PION. Moreover, in patients with occult GCA, similar findings were present. Out of the 6 patients with occult GCA, only 1 had isolated CN VI palsy and 5 had AION [11]. In conclusion, this case reinforces the importance of considering the diagnosis of GCA when evaluating patients with diplopia and unexplained isolated cranial nerve findings, such as CN VI palsy.
References
- Iyza FB, Alexis RP, Ashwini K, et al. Giant cell arteritis: early diagnosis is key. Eye and Brain 11 (2019): 1.
- Winkler A, David T. Giant cell arteritis: 2018 review. Missouri medicine 115.5 (2018): 468.
- Vodopivec I, Joseph FR. Ophthalmic manifestations of giant cell arteritis. Rheumatology 57 (2018): 63-72.
- Ross M, Lulu B, Rosanne S, et al. Multiple cranial nerve palsies in giant cell arteritis. Journal of Neuro-Ophthalmology 37 (2017): 398-400.
- Fytili C, Bournia VK, Korkou C, et al. Multiple cranial nerve palsies in giant cell arteritis and response to cyclophosphamide: a case report and review of the literature. Rheumatology International 35 (2015): 773-776.
- Ross AG, Imran J, Maxwell P, et al. Retrospective, multicenter comparison of the clinical presentation of patients presenting with diplopia from giant cell arteritis vs other causes. Journal of Neuro-Ophthalmology 39 (2019): 8-13.
- Wilson CM, PD'Ath. A Case of Sixth Cranial Nerve Palsy and Suspected Giant Cell Arteritis. BAOJ Ophthalmology 2 (2017): 007.
- Ghanchi FD, Gordon ND. Current concepts in giant cell (temporal) arteritis. Survey of ophthalmology 42 (1997): 99-123.
- Freitag, Frederick G, Seymour Diamond,. Solomon. Reversible multiple cranial nerve palsies in temporal (giant cell) arteritis with normal sedimentation rate: report of a case. The Journal of the American Osteopathic Association 88 (1988): 381-383.
- Freitag FG, Seymour D, Glen DS. Reversible multiple cranial nerve palsies in temporal (giant cell) arteritis with normal sedimentation rate: report of a case. The Journal of the American Osteopathic Association 88 (1988): 381-383.
- Issa M, Lura D, Trishal JP, et al. Ischemic ocular manifestations of giant cell arteritis: A Canadian case series. Journal of the Neurological Sciences 436 (2022): 120222.
- Mehler MF, Lydia R. The clinical neuro-ophthalmologic spectrum of temporal arteritis. The American journal of medicine 85 (1988): 839-844.
