Preliminary Epidemiological Investigation of SARS-CoV-2 and Risk Factors Associated with Infection in Tarhouna, Libya
Article Information
Hanan M. Maetouq1, Abdulsalam S. Mahmoud2,*, Abdulati El Salem3, Khaled A. Aisawi5, Ashraf A Naass6, Abdulaziz M. Alkeelani4, Mahmud EL. Abushhewa4
1Burn and Plastic Surgery hospital, Tripoli, Libya
2Faculty of Veterinary Medicine, University of Tripoli, Libya
3Faculty of Medicine, Alasmarya Islamic University, Libya
4Faculty of Medicine, Azzaytuna University, Libya
5Faculty of Agriculture, Tripoli University, Libya
6Biotechnology Research Centre, Libya
*Corresponding author: Abdulsalam S. Mahmoud, Department of Preventive Medicine, Faculty of Veterinary Medicine, University of Tripoli, P.O. Box 13662, Tripoli, Libya;
Received: 06 June 2021; Accepted: 14 June 2021; Published: 09 July 2021
Citation: Hanan M. Maetouq, Abdulsalam S. Mahmoud, Abdulati El Salem, Khaled A. Aisawi, Ashraf A Naass, Abdulaziz M. Alkeelani, Mahmud EL. Abushhewa. Preliminary Epidemiological Investigation of SARS-CoV-2 and Risk Factors Associated with Infection in Tarhouna, Libya. Fortune Journal of Health Sciences 4 (2021): 373-382.
Share at FacebookAbstract
Background: During the last couple of years, the emerging and re-emerging viral diseases have been spilled over and were considered of great international concern, Severe Acute Respiratory Syndrome (SARS), Middle Eastern Respiratory Syndrome Corona virus (MERS-CoV), Ebola virus disease and Severe Acute Respiratory distress Syndrome (SARS-CoV-2). SARS-CoV-2, the virus that causes corona virus disease 2019 (COVID-19), has spread rapidly around the world since emerging in Wuhan, China, in late 2019.
Objectives: The study was conducted to investigate the epidemiological situation of COVID-19 and risk factors associated with SRAS-CoV-2 infection in Tarhouna city.
Materials and Methods: The cross-sectional study was conducted to investigate the epidemiological situation of COVID-19 and study the risk factors (age, gender, history of contact and comorbidity condition) associated with infection in the city of Tarhouna from December 2020 to Jan 2021. All data were entered into the Microsoft Excel spreadsheet and coded for analysis. Influence of variables like age, gender, comorbidity and history of contact on infection was calculated. A descriptive statistical analysis was performed to analyze the epidemiological characteristics of the confirmed cases of COVID-19 using SPSS version 22. For each proportion the percent and 95% confidence interval (CI) were calculated. Chi square test was used to investigate the level of association among variables at the significance level of p<0.05.
Results: The present study reported 540 confirmed cases of COVID-19 screened by RT.PCR. The result showed the statistical significant (.001) at p < 0.05 among four age categories (≤19 year 5.50%, 20-39 year 42.41%, 40-59 year 48.30% and ≥60 year 4.62%). Significantly (P=.04), the gender influence on infection rate of SARS-CoV-2 amongst target population. The infecti
Keywords
SARS-CoV-2; Infection
SARS-CoV-2 articles SARS-CoV-2 Research articles SARS-CoV-2 review articles SARS-CoV-2 PubMed articles SARS-CoV-2 PubMed Central articles SARS-CoV-2 2023 articles SARS-CoV-2 2024 articles SARS-CoV-2 Scopus articles SARS-CoV-2 impact factor journals SARS-CoV-2 Scopus journals SARS-CoV-2 PubMed journals SARS-CoV-2 medical journals SARS-CoV-2 free journals SARS-CoV-2 best journals SARS-CoV-2 top journals SARS-CoV-2 free medical journals SARS-CoV-2 famous journals SARS-CoV-2 Google Scholar indexed journals Infection articles Infection Research articles Infection review articles Infection PubMed articles Infection PubMed Central articles Infection 2023 articles Infection 2024 articles Infection Scopus articles Infection impact factor journals Infection Scopus journals Infection PubMed journals Infection medical journals Infection free journals Infection best journals Infection top journals Infection free medical journals Infection famous journals Infection Google Scholar indexed journals acute respiratory distress syndrome articles acute respiratory distress syndrome Research articles acute respiratory distress syndrome review articles acute respiratory distress syndrome PubMed articles acute respiratory distress syndrome PubMed Central articles acute respiratory distress syndrome 2023 articles acute respiratory distress syndrome 2024 articles acute respiratory distress syndrome Scopus articles acute respiratory distress syndrome impact factor journals acute respiratory distress syndrome Scopus journals acute respiratory distress syndrome PubMed journals acute respiratory distress syndrome medical journals acute respiratory distress syndrome free journals acute respiratory distress syndrome best journals acute respiratory distress syndrome top journals acute respiratory distress syndrome free medical journals acute respiratory distress syndrome famous journals acute respiratory distress syndrome Google Scholar indexed journals public health emergency of international concern articles public health emergency of international concern Research articles public health emergency of international concern review articles public health emergency of international concern PubMed articles public health emergency of international concern PubMed Central articles public health emergency of international concern 2023 articles public health emergency of international concern 2024 articles public health emergency of international concern Scopus articles public health emergency of international concern impact factor journals public health emergency of international concern Scopus journals public health emergency of international concern PubMed journals public health emergency of international concern medical journals public health emergency of international concern free journals public health emergency of international concern best journals public health emergency of international concern top journals public health emergency of international concern free medical journals public health emergency of international concern famous journals public health emergency of international concern Google Scholar indexed journals Human Diagnostic articles Human Diagnostic Research articles Human Diagnostic review articles Human Diagnostic PubMed articles Human Diagnostic PubMed Central articles Human Diagnostic 2023 articles Human Diagnostic 2024 articles Human Diagnostic Scopus articles Human Diagnostic impact factor journals Human Diagnostic Scopus journals Human Diagnostic PubMed journals Human Diagnostic medical journals Human Diagnostic free journals Human Diagnostic best journals Human Diagnostic top journals Human Diagnostic free medical journals Human Diagnostic famous journals Human Diagnostic Google Scholar indexed journals MERS-CoV articles MERS-CoV Research articles MERS-CoV review articles MERS-CoV PubMed articles MERS-CoV PubMed Central articles MERS-CoV 2023 articles MERS-CoV 2024 articles MERS-CoV Scopus articles MERS-CoV impact factor journals MERS-CoV Scopus journals MERS-CoV PubMed journals MERS-CoV medical journals MERS-CoV free journals MERS-CoV best journals MERS-CoV top journals MERS-CoV free medical journals MERS-CoV famous journals MERS-CoV Google Scholar indexed journals Physicians’ Age, Gender, and Ethnicity articles Physicians’ Age, Gender, and Ethnicity Research articles Physicians’ Age, Gender, and Ethnicity review articles Physicians’ Age, Gender, and Ethnicity PubMed articles Physicians’ Age, Gender, and Ethnicity PubMed Central articles Physicians’ Age, Gender, and Ethnicity 2023 articles Physicians’ Age, Gender, and Ethnicity 2024 articles Physicians’ Age, Gender, and Ethnicity Scopus articles Physicians’ Age, Gender, and Ethnicity impact factor journals Physicians’ Age, Gender, and Ethnicity Scopus journals Physicians’ Age, Gender, and Ethnicity PubMed journals Physicians’ Age, Gender, and Ethnicity medical journals Physicians’ Age, Gender, and Ethnicity free journals Physicians’ Age, Gender, and Ethnicity best journals Physicians’ Age, Gender, and Ethnicity top journals Physicians’ Age, Gender, and Ethnicity free medical journals Physicians’ Age, Gender, and Ethnicity famous journals Physicians’ Age, Gender, and Ethnicity Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals
Article Details
1. Introduction
Corona viruses (CoVs) have been well known since first identified many years ago as primarily zoonotic pathogens and causative of diverse animal illnesses. However, in the 1960s, CoVs were capable of causing human illness usually consistent with self-limiting respiratory infections in humans [1]. In recent years newly identified human pathogen CoVs have caused three significant global outbreaks since 2003. The first of these was Severe Acute Respiratory Syndrome (SARS) which was emerged in 2003 in Hong Kong and Toronto. The second was Middle Eastern Respiratory Syndrome Corona virus (MERS-CoV), and that was mostly localized in the Middle East, although cases well beyond that region were diagnosed. The third is Severe Acute Distress Respiratory Syndrome (SARS-CoV-2) in December 2019 and was named Corona virus Disease-19 (COVID-19), and still of great public health emergency of international concern (PHEIC) [2, 3]. COVID-19, emerged in China when several cases of acute respiratory distress syndrome (ARDS) were reported in Wuhan City, China with unknown etiology [4]. Early epidemiological investigation revealed that these cases were linked to a local wet market (seafood markets, live animal markets) a common commercial source of food in China [5, 4], and therefore, the results suggested that an unknown zoonotic transmission, and ultimately human to human propagation of infection with SARS have long been confirmed [6]. Further research identified the virus as a newly discovered human corona virus, SARS 2 known as COVID-19. Soon after, it became clear COVID-19 is transmitted person to person [6]. With a population of eleven million people, Wuhan City became the epicentre for the resulting COVID-19 outbreak and finally starting point for the global pandemic [7]. Subsequently, led to a substantial increase in cases since December 2019, and until, writing this paper, according to World Health Organization (WHO) data, there have been approximately of 169,597,415, 3,530,582 and 143,208,832 confirmed cases and death of COVID-19 respectively reported worldwide [8]. In Africa, the incidence of COVID-19 varies considerably amongst countries, likely reflecting variations in volumes of air travel and differences in coverage of SARS-CoV-2 testing [9]. Tackling of COVID-19 is becoming increasingly difficult in Northern and sub-Saharan countries because of unstable situations and weak health system [10, 11]. Only few African states have been successful in establishing detection, prevention, and control measures. Yet the COVID-19 pandemic still a challenge for most African countries. Currently, there is scanty data regarding the epidemiological and spatial spread of the COVID-19 pandemic in Africa [12, 13].
In Libya, the first case of COVID-19 entered Libya, was a man with history of travelling in Saudi Arabia during March 2020 [14]. Since then many COVID-19 confirmed cases have been reported and spread all over the country, and clearly, due to instability of the country and weakness in the public health capacities as well as surveillance system not in place therefore, that was made difficult to estimate the proper data that reflect the epidemiological situation of COVID-19 in the country. Therefore, it is likely that COVID-19 will spread unnoticed in the Libyan community, if no preventive measures are taken seriously. So that, understanding the epidemiological situation and local variations of the pandemic patterns is an important step in implementing effective strategies to mitigate the COVID-19 in vulnerable communities. Unfortunately, currently, there is no a global standard response to the pandemic, and each country is dealing with the crisis based on their own facilities and expertise [15]. Regarding the epidemiological situation of pandemic in Tarhouna city, the case zero were confirmed in June 2020 and lockdown protocol was taken place in October 2020. Obviously, there was no clear data could be pointed out or figure out the exact time and source of the zero case in the city.
This study aimed to examine the status and patterns of COVID-19 pandemic in the city of Tarhouna in Libya, the risk factors associated with this pandemic were in scope of the study. The study also highlights the potential strategies to minimize the impact of this pandemic on the Libyan community.
2. Material and Methods
The cross-sectional study was conducted to investigate the epidemiological situation of COVID-19 and study the risk factors (Age, gender, History of contact and comorbidity condition) associated with infection in the city of Tarhouna from December 2020 to Jan 2021. All data were entered into the Microsoft Excel spreadsheet and coded for analysis. Influence of variables like age, gender, comorbidity and history of contact on infection was calculated. A descriptive analyses frequency and percent were measured for numerical data and number and percent for qualitative data by using SPSS version 22. Chi square test was used to investigate the level of association among variables at the significance level of p<0.05.
3. Results
The present study reported 540 confirmed cases of COVID-19 screened by RT.PCR. The result showed that there was a statistical significant difference (.001) at p < 0.05 amongst four age categories (≤19 year 5.50%, 20-39 year 42.41%, 40-59 year 48.30% and ≥60 year 4.62%) (Table 1 and Fig. 1). Significantly, (P=.04), the gender influence on SARS-CoV-2 in infection rate among target population. The infection rate was estimated to be 70.74% (95% CI: 66.90%-4.58%) and 29.50% (95% CI: 25.42%, 33.10%) in male and female respectively (Fig. 2). Our results reported no statistical difference (P=.09) among comorbidity and non-comorbidity cases (Table 1). Comparatively, the infection was found to be higher in history contact 92.7% (95% CI: 90.59%-94.96%) than non-contact 7.2% (95% CI: 5.04%-9.41%) (Fig. 4). Unexpectedly, the infection rate was estimated to be 72.59% (95% CI: 68.83%-76.35%) and 27.27% (95% CI: 23.65%-31.17%) among asymptomatic and symptomatic patients respectively (Fig. 5).
The results revealed that 90.18% (95% CI: 87.68%-92.69%) and 9.81% (95% CI: 7.31%-12.32%) infection rate of SARS-CoV-2 among non-comorbidities and comorbidities population respectively (Fig.3). Additionally, we found that the health status of the confirmed cases, (P=.09) not significantly influence on infection rate.
Table 1: Result of univariate analysis for variables associated with SARS-CoV-2 infection
|
Variables |
Tested |
% positive |
DF |
X2 |
P value |
|
Age Categories/Year |
3 |
15.62 |
.001 |
||
|
0-19 |
25 |
5.50 |
|||
|
20-39 |
229 |
42.41 |
|||
|
40-59 |
261 |
48.30 |
|||
|
60-100 |
25 |
4.62 |
|||
|
Gender |
1 |
4.2 |
.040 |
||
|
Female |
158 |
29.50 |
|||
|
Male |
382 |
70.74 |
|||
|
History of contact |
1.24 |
.26 |
|||
|
Contact |
501 |
92.7 |
|||
|
Non-Contact |
39 |
7.2 |
|||
|
Healthy status |
1 |
2.76 |
.09 |
||
|
Comorbidity |
53 |
9.81 |
|||
|
Non- Comorbidity |
487 |
90.18 |
|||
|
Clinical aspect |
1 |
||||
|
Symptomatic |
148 |
27.27 |
.912 |
.012 |
|
|
Asymptomatic |
392 |
72.59 |
|||
|
Total |
540 |
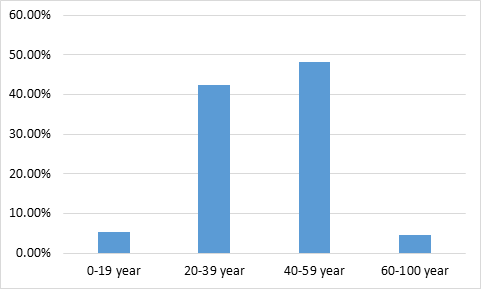
Figure 1: The infection rate of SARS-CoV-2 among of confirmed cases belong to different age group
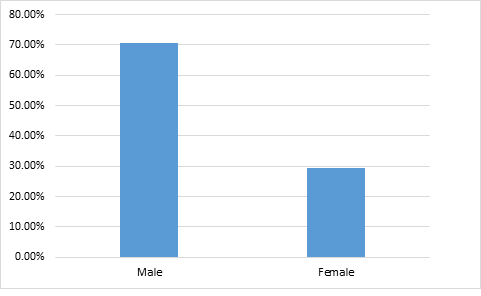
Figure 2: the infection rate of SARS-CoV-2 according to the gender
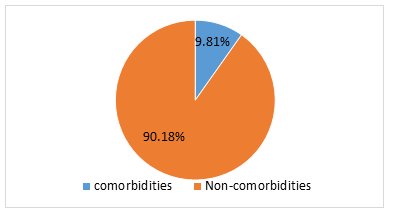
Figure 3: The infection rate of SARS-CoV-2 according to the healthy status
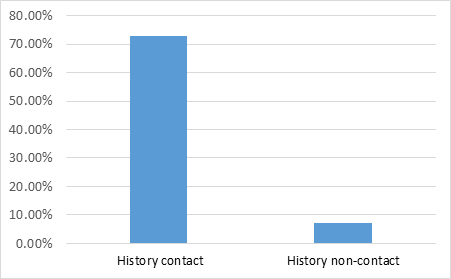
Figure 4: The infection rate of SARS-CoV-2 among population with history and without history of close contact of confirmed cases
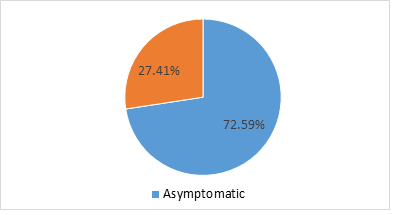
Figure 5: The infection rate of SARS-CoV-2 among the symptomatic and asymptomatic confirmed cases
4. Discussion
The present study reported high infection rate of SARS-CoV-2 among the target population in Tarhouna city. To best our knowledge, this the first study investigates the epidemiological situation of COVID-19 in Tarhouna city in Libya. This city is located southeast of Tripoli, in the Murqub District with a population density of about 300000, and considered one of the largest cities in Libya with a high population. In Libya, since the first case reported on 24 March 2020, still the epidemiological patterns of COVID-19 among different Libyan cities clearly variables [3], however, three months later, the first officially confirmed cases of COVID-19 were reported in Tarhouna, and it seems to be reported before that time and might be overlapped and the reason being that instability of the city was made it difficult to implement the surveillance and trace back of infected cases in the city. In fact, there is still a scarcity of information regarding the epidemiological situation of COVID-19 in the Tarhouna city, and in the country in general, and the epidemic curve of COVID-19 in Libya has risen sharply since July 2020, and the country entered the cluster pandemic stage [3]. Regardless, the obtained results reflect a high percentage of infection in this city, however, the infection rate might be substantially higher than reported. Comparatively, the present study reported the highest infection rate of COVID-19 in males. This variability among gender might be attributable to many factors that influence infection rate, like physiological or/and biological factors [16, 17]. There are many studies reported that expression of angiotensin converting enzyme 2 (ACE2) receptors which have a potential role for SARS-CoV-2 viral entry and transmission is difference between both genders [18, 19]. However, the gender variance of infection rate could be multifactorial that might be influenced by sex bias reported in the present study. Also the gender-based socio-cultural and behavioural differences are other factors that influence the infection rate among males and females. Due to attitudes, costumes, and behaviour life, men are more likely to get an infection [20]. In agreement with different studies reported that the male’s sexes more frequently exposed to be infected with infectious disease [20]. In contrast to other reports, they have found no significant difference between both sexes in the proportion of males and females infected with SARS-CoV-2 [21, 20]. According to the global COVID-19 meta-analysis, the male is considered a risk factor for intensive care unit (ITU) and death [22]. In line with other studies, the infection rate reported significant differences among four age group categories (≤19 years 12%, 20-39 year 6.98%, 40-59 year 11.11%, and ≥60 years 32%), significantly, the age influence on COVID-19 infection rate among the population [23]. The highest infection rate (32%) was reported in ≥60 years while the lowest (6.98%) in 20-39 years. Comparatively, the infection rate difference reported among age groups might be influence by the age-immunity factors [24], however, the high age group more exposed to infection than the lower age group, and consequently clinical features or clinical course of disease more clear and detectable in the elderly cases as contrast young ages, therefore, clinical form of COVID-19 in young age might be silent and undetectable [25]. According to the WHO clinical definition of COVID-19, there are five levels of severity which include mild (silent), severe, acute, sepsis, and septic shock [25]. Significantly, our data showed that, high asymptomatic (silent) cases (72.59%) as compared to symptomatic (27.27%). In agreement with other studies had reported a higher infection rate among silent cases of COVID-19 (26). Clearly, due to low testing capacity, there was infection data missing, and difficult to quantify asymptomatic infection and transmission in the city. Consequently, the infection rate in the city might be higher than that reported and could not be easily detectable. And there are many infected cases that seem to be underestimated, and tracing of index cases to who closely contact it is very hard and difficult to perform for many reasons, likely, the shortage of public health capacities, political instability, and civilian conflict within and around the city had to make it difficult to implement any strategy to combat COVID-19. The present study reported no statistical difference among patients with comorbidities condition. Importantly, due to a shortage in data of the ethnicity and comorbidities individuals in the city, therefore, the non-significant difference results in the present study might not be valuable and could not reflect real results. It is well known that the comorbidities patients are considered the most risk group [24, 27]. In spite, the weakness in the public health capacities and surveillance system in the country since 2016, therefore, WHO has implemented an Early Warning Response Alertness Network (EWRN) in Libya to combat and mitigate emerging and re-emerging of infectious diseases. Notably, the present study findings regarding epidemiological patterns of COVID-19 are considered warranty and valuable at least among the target population in Tahrhouna city.
5. Conclusion
This study is the first in Tarhouna city to provide information on epidemiological characterization of COVID-19 pandemic in this city. The study emphasizes the significant effects of older age, male gender and underling diseases on the risk of mortality among COVID-19 patients. In spite, we excluded risk factors that constituted laboratory findings, vital signs or symptoms and silent cases of COVID-19, clearly that, asymptomatic cases could be (underestimated) under go without being noticed. Therefore, it is recommended to take preventative measures more seriously in the elderly patients, and asymptomatic cases that play a potential silent role in COVID-19 epidemiology, and larger scale studies are highly recommended to investigate deeply the epidemiology of this virus among Libyan population.
6. Acknowledgement
The authors would like to thank the Mr. Ahmed AllafiFarag and Faisal Bashir Alruzayzi from the NCDC Tarhona Branch for their invaluable assistances in collecting data used in the current study.
7. Conflict of interest
There is no conflict of interest
8. References
- Fehr RA, Stanley Perlman S. Corona viruses: An Overview of Their Replication and Pathogenesis. Methods Mol Biol 1282 (2015):1-23.
- Hui DS, Azhar E, Madani TA, Ntoumi F, Kock R, Dar O, et al. The continuing 2019-nCoV epidemic threat of novel corona viruses to global health—the latest 2019 novel corona virus outbreak in Wuhan, China. Int J Infect Dis 91 (2020):264-6.
- Mahmoud AS, Mayouf AS, Dhawi A, Ellafi AM. Preliminary Survey to Understand the Epidemiology of COVID-19 and Its Socio-economic Impacts in Libya. Fortune Journal of Health Sciences 4 (2021): 243-25.
- Wu F, Zhao S, Yu B, Chen Y-M, et al. A new corona virus associated with human respiratory disease in China. Nature (2020).
- Zhu N, Zhang MD, Wang W, Li X, et al. A novel corona virus from patients with pneumonia in China, 2019. N. Engl. J. Med 382 (2020) 727-733.
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel corona virus-infected pneumonia. N Engl J Med (2020).
- Leung G, Wu J. Real-time now cast and forecast on the extent of the Wuhan CoV outbreak, domestic and international spread. Media Conference 27 January (2020).
- World Health Organization (WHO). WHO Corona virus (COVID-19) Dashboard (2021).
- Gilbert M, Pullano G, Pinotti F, et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modeling study. The Lancet 395 (2020) 871-7.
- Da'ar OB, Haji M, Jradi H. Corona virus Disease 2019 (COVID-19): Potential implications for weak health systems and conflict zones in the Middle East and North Africa region. The International journal of health planning and management (2020).
- Gyasi RM. Fighting COVID-19: Fear and internal conflict among older adults in Ghana. Journal of gerontological social work 20 (2020):1-3
- Daw MA, El-Bouzedi AH, Ahmed MO, Cheikh Y. Spatial Distribution and Geographic Mapping of COVID-19 in Northern African Countries; A Preliminary Study. J Clin Immunol Immunother 6 (2020):032.
- Arashi M, Bekker A, Salehi M, Millard S, Erasmus B, Cronje T, Golpaygani M. Spatial analysis and prediction of COVID-19 spread in South Africa after lockdown. arXiv preprint arXiv:2005.09596 (2020).
- National Center for Diseases Control. COVID-19 Updates in Libya (2020).
- Rajendran DK, Rajagopal V, Alagumanian S, et al. Systematic literature review on novel corona virus SARS-CoV-2: a threat to human era. Virus Disease 31:161-173.
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area JAMA 323 (2020):2052.
- Scully EP, Haverfield J, Ursin RL, et al. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat. Rev. Immunol 20 (2020):442-447.
- Bukowska A, Spiller L, Wolke C, et al. Protective regulation of the ACE2/ACE gene expression by estrogen in human atrial tissue from elderly men. Exp. Biol Med 242 (2017):1412-1423.
- Cai G. Bulk and single-cell transcriptomics identify tobacco-use disparity in lung gene expression of ACE2, the receptor of 2019-nCov. Med Rxiv.
- Zhao Y,Zhao Z, Wang Y, et al. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. Am J Respir Crit Care Med 202 (2020):756-759.
- Kragholm K, Andersen IP, Gerds T, et al. Association between male sex and outcomes of Corona virus Disease 2019 (Covid-19) - a Danish nationwide, register-based study. Clin Infect Dis (2020).
- Singh S, Chowdhry M, Chatterjee A, et al. Gender-Based Disparities in COVID-19: Clinical Characteristics and Propensity-matched Analysis of Outcomes. Med Rxiv (2020).
- Tian T, Zhang J, Hu L, et al. Risk factors associated with mortality of COVID-19 in 3125 counties of the United States. Infect Dis Poverty 10 (2020):3.
- Santesmasses D, Castro JP, Zenin AA, et al. COVID-19 is an emergent disease of aging. Aging Cell 19 (2020).
- Frasca D, Blomberg BB, and Paganelli R. Aging, obesity, and inflammatory age-related diseases. Front. Immunol. 8 (2017):1745.
- Wang D,Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Corona virus-Infected Pneumonia in Wuhan, China. JAMA 323 (2020): 1061-1069.
- Manski CF and Molinari F. Estimating the COVID-19 infection rate: Anatomy of an inference problem. Journal of Econometrics 220 (2021):181-192.
