Pre and Post-Operative Computer Tomography Findings of a patient with a Type A Aortic Dissection Extending from the Aortic Valve to Iliac Vessels
Article Information
Saqib M Rafiq1*, Manjit Riyat2
1Watford General Hospital, Watford, UK
2Wexham Park Hospital, Slough, UK
*Corresponding Author: Saqib M Rafiq, Watford General Hospital, Watford, UK
Received: 07 May 2020; Accepted: 28 May 2020; Published: 01 July 2020
Citation: Saqib M Rafiq, Manjit Riyat. Pre and Post-Operative Computer Tomography Findings of a patient with a Type A Aortic Dissection Extending from the Aortic Valve to Iliac Vessels. Journal of Radiology and Clinical Imaging 3 (2020): 074-079.
Share at FacebookAbstract
Aortic dissection is a high morbidity, high mortality, medical catastrophe. It is twice as common as ruptured abdominal aortic aneurysm and the mortality following acute aortic dissection is often quoted in hours. The presentation of Aortic Dissection is variable and can be diagnostically challenging, which can have a direct effect on mortality in often young and relatively healthy patients. We present the case of a young man who presented to the emergency departments with central chest pain and ST depression laterally on his ECG. A computer tomography (CT) scan revealed The CT scan showed a proximal Type A dissection involving the aortic valve and the coronary arteries, extending down to the iliac vessels. The patient was transferred to a cardiothoracic centre to undergo emergency surgery and had repair of the aortic dissection, he made a good post-operative recovery and has no residual neurological deficit. A further computer tomography scan was performed 8 months later which showed no change in the patient vascular anatomy.
Keywords
Type A Dissection; Computer Tomography Scan; Surgery; Chest Pain; Investigations
Type A Dissection articles, Computer Tomography Scan articles, Surgery articles, Chest Pain articles, Investigations articles
Type A Dissection articles Type A Dissection Research articles Type A Dissection review articles Type A Dissection PubMed articles Type A Dissection PubMed Central articles Type A Dissection 2023 articles Type A Dissection 2024 articles Type A Dissection Scopus articles Type A Dissection impact factor journals Type A Dissection Scopus journals Type A Dissection PubMed journals Type A Dissection medical journals Type A Dissection free journals Type A Dissection best journals Type A Dissection top journals Type A Dissection free medical journals Type A Dissection famous journals Type A Dissection Google Scholar indexed journals Computer Tomography Scan articles Computer Tomography Scan Research articles Computer Tomography Scan review articles Computer Tomography Scan PubMed articles Computer Tomography Scan PubMed Central articles Computer Tomography Scan 2023 articles Computer Tomography Scan 2024 articles Computer Tomography Scan Scopus articles Computer Tomography Scan impact factor journals Computer Tomography Scan Scopus journals Computer Tomography Scan PubMed journals Computer Tomography Scan medical journals Computer Tomography Scan free journals Computer Tomography Scan best journals Computer Tomography Scan top journals Computer Tomography Scan free medical journals Computer Tomography Scan famous journals Computer Tomography Scan Google Scholar indexed journals Surgery articles Surgery Research articles Surgery review articles Surgery PubMed articles Surgery PubMed Central articles Surgery 2023 articles Surgery 2024 articles Surgery Scopus articles Surgery impact factor journals Surgery Scopus journals Surgery PubMed journals Surgery medical journals Surgery free journals Surgery best journals Surgery top journals Surgery free medical journals Surgery famous journals Surgery Google Scholar indexed journals Chest Pain articles Chest Pain Research articles Chest Pain review articles Chest Pain PubMed articles Chest Pain PubMed Central articles Chest Pain 2023 articles Chest Pain 2024 articles Chest Pain Scopus articles Chest Pain impact factor journals Chest Pain Scopus journals Chest Pain PubMed journals Chest Pain medical journals Chest Pain free journals Chest Pain best journals Chest Pain top journals Chest Pain free medical journals Chest Pain famous journals Chest Pain Google Scholar indexed journals Investigations articles Investigations Research articles Investigations review articles Investigations PubMed articles Investigations PubMed Central articles Investigations 2023 articles Investigations 2024 articles Investigations Scopus articles Investigations impact factor journals Investigations Scopus journals Investigations PubMed journals Investigations medical journals Investigations free journals Investigations best journals Investigations top journals Investigations free medical journals Investigations famous journals Investigations Google Scholar indexed journals ECG articles ECG Research articles ECG review articles ECG PubMed articles ECG PubMed Central articles ECG 2023 articles ECG 2024 articles ECG Scopus articles ECG impact factor journals ECG Scopus journals ECG PubMed journals ECG medical journals ECG free journals ECG best journals ECG top journals ECG free medical journals ECG famous journals ECG Google Scholar indexed journals CT aortogram articles CT aortogram Research articles CT aortogram review articles CT aortogram PubMed articles CT aortogram PubMed Central articles CT aortogram 2023 articles CT aortogram 2024 articles CT aortogram Scopus articles CT aortogram impact factor journals CT aortogram Scopus journals CT aortogram PubMed journals CT aortogram medical journals CT aortogram free journals CT aortogram best journals CT aortogram top journals CT aortogram free medical journals CT aortogram famous journals CT aortogram Google Scholar indexed journals vascular anatomy articles vascular anatomy Research articles vascular anatomy review articles vascular anatomy PubMed articles vascular anatomy PubMed Central articles vascular anatomy 2023 articles vascular anatomy 2024 articles vascular anatomy Scopus articles vascular anatomy impact factor journals vascular anatomy Scopus journals vascular anatomy PubMed journals vascular anatomy medical journals vascular anatomy free journals vascular anatomy best journals vascular anatomy top journals vascular anatomy free medical journals vascular anatomy famous journals vascular anatomy Google Scholar indexed journals PCI articles PCI Research articles PCI review articles PCI PubMed articles PCI PubMed Central articles PCI 2023 articles PCI 2024 articles PCI Scopus articles PCI impact factor journals PCI Scopus journals PCI PubMed journals PCI medical journals PCI free journals PCI best journals PCI top journals PCI free medical journals PCI famous journals PCI Google Scholar indexed journals Radio-femoral delay articles Radio-femoral delay Research articles Radio-femoral delay review articles Radio-femoral delay PubMed articles Radio-femoral delay PubMed Central articles Radio-femoral delay 2023 articles Radio-femoral delay 2024 articles Radio-femoral delay Scopus articles Radio-femoral delay impact factor journals Radio-femoral delay Scopus journals Radio-femoral delay PubMed journals Radio-femoral delay medical journals Radio-femoral delay free journals Radio-femoral delay best journals Radio-femoral delay top journals Radio-femoral delay free medical journals Radio-femoral delay famous journals Radio-femoral delay Google Scholar indexed journals
Article Details
1. Case Report
A 38 year-old male with an unremarkable medical history was brought into resus as a pre-alert by the paramedics with central chest pain and ST depression laterally on his ECG. He had been discussed en-route with a PCI centre who declined urgent PCI as there was no ST elevation observed. At presentation he looked uncomfortable and was writhing in pain, he described central chest discomfort and a dull ache posteriorly, which started abruptly an hour prior to admission. He was sweating and was nauseous. He appeared in pain from the end of the bed and was connected to a cardiac monitor as the handover was being received from the paramedics.
It was noted that his heart rate was 71 beats per minute, sinus, but looking at the monitor there appeared to be some occasional pauses on his ECG, lasting less than 2 seconds. His blood pressure was 155/47 in the left arm and 149/51 in the right arm. On auscultation of the chest he had a soft ejection systolic murmur and a harsh, loud, decrescendo diastolic murmur heard throughout the precordium, loudest at the lower left sternal edge. No radial-radial or radio-femoral delay could be appreciated. He had a normal cranial nerve examination. Peripheral neurological examination showed normal tone, power, sensation, reflexes and co-ordination of all 4 limbs.
An urgent CT aortogram was requested due to suspicion of a proximal aortic dissection involving the aortic valve. A volumetric acquisition of the thorax, abdomen and pelvis with intravenous contrast showed a proximal Type A dissection. The aneurysmal dilation of the ascending aorta measured 70 mm in approximate diameter. The dissection flap extended from the aortic root into the arch, descending, abdominal aortic segments and subsequently the external and internal iliac arteries bilaterally. The flap also involved the origin of the brachiocephalic artery as well as the coronary arteries Figures 1a-c).
The Figures were linked to the dissection service on call hospital and referral was made. The patient was accepted for transfer and whilst waiting for paramedic arrival an arterial line was placed for invasive beat to beat blood pressure monitoring. An intravenous labetalol infusion was started and up-titrated gradually to 4mg/minute which slowed the heart rate to 66 bpm, reduced blood pressure to 105/43 and allowed coronary perfusion, which led to resolution of ECG pauses.
The patient was transferred to a cardiothoracic centre to undergo emergency surgery and had repair of the aortic dissection, he made a good post-operative recovery and has no residual neurological deficit. The patient returned to the hospital with chest pain 8 months later and another CT aortogram was performed which demonstrated no acute pathology to cause the patients symptoms (Figures 2a-c). The patient was observed overnight and discharged home.

Figure 1a: Dissection flaps visible in both ascending and descending aorta.

Figure 1b: CT aortogram showing dissection at the level of the aortic arch.

Figure 1c: Dissection flaps extending into both common iliac arteries.
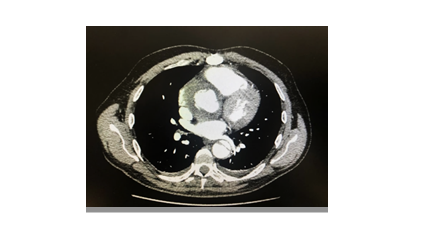
Figure 2a: Dissection flaps visible in both ascending and descending aorta 8 months post operatively.
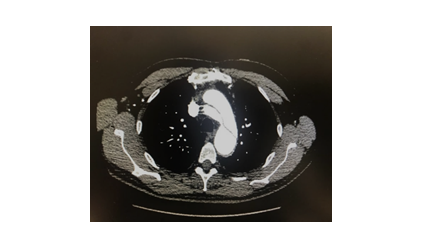
Figure 2b: CT aortogram showing dissection at the level of the aortic arch 8 months post operatively.
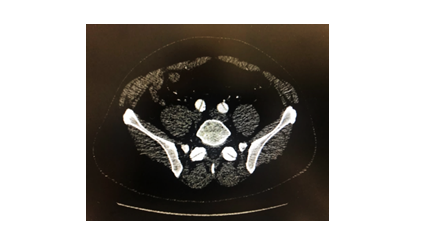
Figure 2c: Dissection flaps extending into both common iliac arteries 8 months post operatively.
2. Discussion
Aortic dissection occurs at a rate of 3 per 100,000 per year, risk factors include hypertension, hypercholesterolaemia, amphetamine use, connective tissue disease, male gender and trauma. 75% of those who suffer aortic dissection have pre-existing hypertension [1]. Classification is commonly based on the DeBakey or Stanford systems of classification [2].
—DeBakey:
—Type I – Ascending aorta, arch and descending aorta (Stanford type A).
—Type II – Ascending aorta only (Stanford type A).
—Type IIIa – Descending aorta distal to left subclavian artery and proximal to coeliac trunk (Stanford type B).
—Type IIIb – Descending aorta distal to left subclavian artery extending into abdominal aorta.
Patients most commonly present with an abrupt severe sharp stabbing or tearing type pain. Chest pain is more common in type A dissections, In type B dissections more commonly present with back pain and abdominal pain [2]. On examination patients may present with tachycardia alongside hypertension, new murmur of aortic regurgitation and neurological deficit [3]. Hypotension usually presents in cases of aortic rupture, pericardial tamponade and myocardial ischemia if the coronary arteries are involved [2].
In suspected aortic dissections urgent imaging is vital to confirm diagnosis. Multiple modalities can be used to facilitate diagnosis. A chest x-ray can be performed and may show a widened mediastinum which is present in 60% of cases however it may not reveal any abnormality [4]. Echocardiography can be used at the bedside which is suitable for hemodynamically unstable patients.
Transoesophageal echocardiography has a higher sensitivity and specificity than transthoracic echocardiography, however this accuracy is operator dependant. Transoesophageal echocardiography is difficult in obese patients and the upper ascending aorta and arch may not be visualised well as a result; false positive results may occur [5]. CT angiography is the most frequently used in acute settings and is recommended by the European Society of Cardiology as the first line investigation of suspected aortic dissection. It allows for urgent assessment of the dissection, including the extent of the dissection, differentiation of true and false lumens and allows planning for open or endovascular surgery [3, 6]. CT angiography is not suitable in patients with renal impairment or contrast allergy. It may also be difficult to transfer haemodynamically unstable patients for a CT scan [7].
Management includes analgesia and aggressive treatment of hypertension, commonly using intravenous beta blockers, with an aim of systolic BP between 100-120. Coagulopathy should be corrected and cardiothoracic surgery is indicated for those with a Type A dissection, meanwhile type B dissections can be managed conservatively with long term control of hypertension and monitoring [2]. Ten-year survival rate of patients discharged from hospital ranges from 30% to 60% [3]. Patients require medical follow up with monitoring of blood pressure regularly and radiological surveillance [2].
3. Conclusion
In-hospital mortality in aortic dissections remains high despite advances in diagnosis and management of the condition. Dissections can present with typical symptoms such as sharp stabbing chest pain or subtle symptoms such as mild backpain with neurological symptoms. This case highlights some of the salient clinical features in aortic dissection. In addition, it emphasises the importance of radiological examination and the role of the radiologist in improving survival rates of aortic dissection. Prompt diagnosis, which allows for timely management, is crucial in improving outcomes for this cohort of patients.
Conflict of Interest
We have no conflicts of interests to declare in writing this case report.
References
- LeMaire SA, Russell L. Epidemiology of thoracic aortic dissection. Nature reviews cardiology 8 (2011): 103.
- Hebballi R, Swanevelder J. Diagnosis and management of aortic dissection. Continuing education in anaesthesia, critical care and pain 9 (2009): 14-18.
- Thrumurthy SG, Karthikesalingam A, Patterson BO, et al. The diagnosis and management of aortic dissection. Bmj 344 (2012): d8290.
- Gomes AS, Bettmann MA, Boxt LM, et al. Acute chest pain--suspected aortic dissection. American College of Radiology. ACR Appropriateness Criteria. Radiology 215 (2000): 1.
- Meredith EL, Masani ND. Echocardiography in the emergency assessment of acute aortic syndromes. European Journal of Echocardiography 10 (2009): i31-i39.
- Erbel R, Alfonso F, Boileau C, et al. Diagnosis and management of aortic dissection: task force on aortic dissection, European society of cardiology. European heart journal 22 (2001): 1642-1681.
- Nasim B, Mohammad A, Zafar S, et al. Aortic Dissection. In Differential Diagnosis of Chest Pain. IntechOpen (2019).
