Practical Knowledge and Attitudes of Caregivers Faced with Covid-19 At Sikasso Hospital - Mali
Article Information
Dadé Ben Sidi Haidara*, 1, Kante M2, Cissouma A3, Traore M4, Traore O5, Dolo A6, Traore AK7, Denou M8, O Koita9, G Dabo10.
1Epidemiologist, Administration Department, Sikasso Hospital, MD-PhD Epidemiology, Director General, Hôpital de Sikasso, Mali
2Department of Anesthesia and Intensive Care, Sikasso Hospital-Mali
3Pediatric Service, Sikasso-Mali Hospital, Mali
4Department of Medicine, Sikasso-Mali Hospital, Mali
5Department of Medicine, Sikasso-Mali Hospital, Mali
6Department of Medicine, Sikasso-Mali Hospital, Mali
7Cardiology Department, Sikasso-Mali Hospital, Mali
8Traumatology-Orthopedics Department, Sikasso-Mali Hospital, Mali
9USTTB-FAPA-LBMA(Université des Sciences Techniques et Technologie de Bamako)-Faculty of Pharmacy- Applied Molecular Biology Laboratory-Bamako-Mali
10USTTB-FMOS (University of Technical Sciences and Technology of Bamako)-Faculty of Medicine and Odonto-Stomatology- Hospital of Mali
*Corresponding author: Dadé Ben Sidi Haidara. Epidemiologist, Administration Department, Sikasso Hospital, MD-PhD Epidemiology, Director General, Hôpital de Sikasso, Mali.
Received: 16 February 2023; Accepted: 12 May 2023; Published: 19 May 2023
Citation: Dadé Ben Sidi Haidara, Kante M, Cissouma A, Traore M, Traore O, Dolo A, Traore AK, Denou M. Practical Knowledge and Attitudes of Caregivers Faced with Covid-19 At Sikasso Hospital - Mali. Fortune Journal of Health Sciences. 6 (2023): 215-221.
Share at FacebookAbstract
Background: Since the introduction of coronavirus in Mali in March 2020, Sikasso Hospital has been designated a management center. The aim of this study was to determine the level of knowledge and practical attitudes of health care providers regarding COVID-19.
Method/Results: This was a qualitative cross-sectional study conducted from December 10 to 12, 2020. Our sample was nonrandomized for convenience, with 42 caregivers. Direct observation and questionnaire interview techniques were used. Data were analyzed using SPSS 23.0 and Excel 2017 software. The average age was 42.3 ± 8.1 years; 85.7% of respondents were male versus 14.3% female. This population consisted of 31% physicians/pharmacists, 47.6% nurses and 21.4% support staff. The majority (69%) had a level of education that allowed them to make appropriate judgments about a health problem. All agents were informed about COVID-19 through the media, the department, their families or friends. The screening rate was 2.56 ‰. The majority of patients were also health workers (16.5%). The change in the status of the hospital as a center for the management of the disease caused "fear, stress, panic" among the caregivers.
Conclusion: This study allowed us to determine the level of WTP of caregivers in the face of this disease at the hospital level.
Keywords
COVID-19, Knowledge Attitudes Practices, Hospital
Article Details
1. Introduction
During recent decades, a large number of people have been affected by the 3 epidemics caused by the coronavirus family (SARS-2003, MERS-2012 and COVID-2019) worldwide. Nevertheless, there is significant genetic dissimilarity between the pathogens of the three previous epidemics, especially MERS with COVID-19. In previous epidemics, the initial disease foci were the Middle East, Saudi Arabia (MERS), and China, and animal-to-human and human-to-human pathogen transmissions have been reported in other countries [1,2]. For COVID-19, as suggested by epidemiological evidence in China, this outbreak began in a seafood and live animal shopping mall in Wuhan, Hubei Province, on December 12, 2019. However, similar to two previous outbreaks, the current outbreak also shifted immediately to human-to-human transmission and swept through most parts of China even faster than previous pandemics. [3] Recent epidemics of viral respiratory diseases around the world began in China (with the exception of MERS originating in Saudi Arabia), and there are several possible reasons for this. From an economic point of view, China has become one of the major producing countries of various commodities, especially in the last decade, and given the huge volume of trade, tourism and military transactions with other countries, there was no doubt that the virus would spread to other parts of the world [4].
Since March 25, 2020, Mali has recorded its first case of COVID-19 through an introduction from Europe and was the start of community transmission. The country has recorded 3,980 positive cases, 141 deaths, 89 of which occurred in care centers and 52 in communities; 2,972 cured and 672 contact persons followed [5]. This case-fatality rate is low compared to that of Europe, but this epidemic has shown the fragility of our health system in the detection and management of severe cases of this disease. The measures taken by our states, notably the closing of borders and the curfew, have had an impact on the movement of people and goods. The economic impact of COVID-19 has not been fully assessed, especially on the informal economic system.
Hospitals constitute a favourable environment for the spread of pathogens with epidemic potential if prevention measures are not properly implemented.
The first human coronaviruses were isolated in the 1960s from the respiratory tract of subjects with the common cold [6,7]. In humans, there are 4 strains that are well known and circulating: HCoV-229E, HCoV-OC43, HCoV-NL63 and HCoV-HKU1 [8,9], which are responsible for 15% of colds, and 90% of adults have antibodies directed against these 4 strains [10,11]. These coronaviruses are most similar to SARS-CoV-2 in their ability to replicate in the respiratory tract. Current data suggest that immunity in animals is of short duration of response, requiring both a fine balance of cellular and humoral immunity. [9] No data are available to affirm that this is the case in humans.
A study on the knowledge and practical attitudes of caregivers regarding COVID-19 could be conducted to contribute to the fight against the current pandemic. To address this issue, the management of the Sikasso Hospital and the EIR (Rapid Intervention Team) attempted to examine the knowledge and practical attitudes (CAP) of caregivers in relation to COVID-19. The objective of this study was to determine the level of knowledge and practical attitudes of health care providers regarding the risk of coronavirus.
2. Materials/Methods
Study setting: Sikasso Hospital
The hospital in Sikasso served as the study setting, and its missions are to
- Ensure the diagnosis and treatment of sick, injured and pregnant women;
- Take charge of emergencies and referrals;
- To ensure the initial and continuing training of health professionals;
- Conduct research in the medical field.
Hospital Capabilities: The hospital has 15 departments with 163 beds. There are 253 agents.
Organization of care: PEC center
Mali, like other countries, has declared cases of coronavirus since March 25, 2020.
With regard to the regional plan of response to the disease, the hospital of Sikasso plays an important role in the detection of cases but also in transit while waiting for biological confirmation.
On 16/03/20, the first meeting of the RIT was held, which was set up to
- To sensitize the staff, patients and accompanying persons to the prevention of COVID-19
- Help the consultation teams to isolate suspected cases of COVID-19 at the hospital level
- Ensuring the collection of samples
- Send the sample to the DRS (Direction Régionale de la Santé) of Sikasso
- Take charge of the suspected case while waiting for the results
Thus, a white plan was developed to respond to possible cases at the facility, and five subteams were formed:
- The logistics sub-team chaired by the hospital pharmacist and the supervisor to make available and on time the consumables and inputs to address the suspected case;
- The sampling sub-team, made up of the laboratory manager and his technicians. Its role will be to take the sample and send it to the DRS.
- The care sub-team, chaired by the infectious disease physician, is composed of anaesthesiologists, nephrologists, ENT (ear, nose and throat) physicians, general practitioners and nurses. Its role is to take charge of all suspected cases before the diagnosis is confirmed;
- The disinfection sub-team: under the direction of the head of hospital hygiene and the general supervisor of the hospital, will proceed to the total disinfection of the space used to see the patient, his family environment and his route;
- The communication and psycho-social care sub-team under the direction of the representative of the social service will take into account all the exchanges to obtain a favourable behaviour of the patients and accompanying persons during their stay in the hospital, as well as the psycho-social accompaniment of the victims and their relatives in case of infection by the coronavirus disease.
Itinerary of the patient
Entrance of the patient to the hospital:
A team composed of advanced trainees and the general supervisor of the hospital will take the temperature of each passer-by (patient and accompanying persons) and will observe hand washing with soap; a triage form with a score of the patients who came for consultation will be used at the entrance of the patient to allow the detection in real time of a patient suspected of COVID-19 to further warn the staff and other patients hospitalized within the structure.
- If the patient has a score ≥ 4, he/she will be referred to the consultation tent in front of the emergency room, or a team will take care of his/her ECP involving the referring physician for whom the consultation is requested;
- If the patient has a score of less than 4, he/she continues his/her therapeutic itinerary
Isolation of the suspected patient.
In front of each case that meets the definition of a suspect case, the health worker who is in front of the patient alerts the president of the RIT.
The role of the RIT in this specific case will be to carry out the necessary investigations to confirm or deny the suspected case.
Type of study:
This is a qualitative study from December 10-12, 2020.
Study Population:
The target population was caregivers at Sikasso Hospital involved in the management of coronavirus disease.
Inclusion criteria: Included were:
- All personnel involved in the management of patients with COVID-19 and cared for at the Sikasso Hospital.
Non-inclusion criteria: Other caregivers not involved in the care of patients with COVID-19 were excluded from this study.
Sampling
Sampling method: It was non-probabilistic with two techniques:
Reasoned selection of all personnel involved in the care of patients with COVID-19, i.e. Forty-two caregivers: administrative personnel, infectious disease specialists, an anesthesiologist-intensive care physician, biologists, radiologists, gynecologists, general practitioners, laboratory technicians, nurses, a hygienist, laborers and drivers.
Because of time constraints, no rigid interview schedule was established.
Sample size: A total of 42 officers were interviewed.
Data Collection:
Collection technique: Two techniques were used: observation of the hospital environment and interviews with hospital staff.
Data collection tools: Following the techniques, two data collection tools were used: the Observation Grid and the Interview Guide.
Data collection process:
Data collection took place from 10/12/2020 to 19/12/2020.
The interviews with hospital staff members were conducted from 10/12/2020 to 12/15/2020. Observation of the hospital environment covered the entire data collection period.
Data Analysis Plan:
Proportions were calculated to describe qualitative variables and means followed by standard deviation for quantitative variables with a symmetrical distribution. Interview and observation data were analyzed and triangulated qualitatively. In contrast, each interview was an opportunity to clarify the issues in relation to the concepts identified without going back over certain factual aspects that differed little from one interviewee to another. Once these interviews had been synthesized (Appendix 4), analyzed and cross-checked, the results were compared with the literature in organizational sociology, in particular the concept of the hospital as a negotiated order by A. Strauss. The bibliographic references are presented in the order of call according to the Vancouver standard.
Ethical considerations
After explaining the benefits of this study, informed consent was obtained from all interviewees, and the confidentiality of the data collected was guaranteed by keeping the names anonymous.
3. Results
Descriptive analysis of variables:
Forty-two involved personnel were interviewed.
Sociodemographic and clinical characteristics:
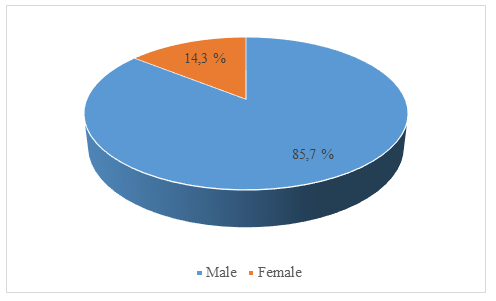
The mean age was 42.3 ± 8.1 years. More than half (85.7%) of the respondents were male, with a sex ratio (male/female) of 6 (Figure 1).
This population consisted of 31% physicians/pharmacists, 47.6% nurses and 21.4% support staff. Approximately ninety-eight percent (97.6%) of the respondents were living with a partner, and 54.8% had no experience in epidemic management (Table 1).
Table 1: Sociodemographic and professional characteristics of agents
|
Variables |
Number (n=42) |
Percentage (%) |
|
Age, mean ± SD |
42,3 ± 8,1 ans |
- |
|
Professional Category |
||
|
Physicians/Pharmacists |
13 |
31, 0 |
|
Nurses |
20 |
47,6 |
|
Other |
9 |
21,4 |
|
Gender |
||
|
Male |
36 |
85,7 |
|
Female |
6 |
14,3 |
|
Marital status |
||
|
Married |
41 |
97,6 |
|
Not married |
1 |
2,4 |
|
Experiences Epidemic management |
||
|
Yes |
19 |
45,2 |
|
No |
23 |
54,8 |
The majority (69%) had a level of education that would allow them to make appropriate judgments about a health problem. All agents were informed about COVID-19 through the media, the service, their families or friends. The screening rate was 2.56 per thousand (1826/711949 inhabitants of the Sikasso Health District). The majority of patients were health workers (16.5%). The positivity rate was 30.79% (97 cases/315 samples). Behavior and Practical Attitudes of Caregivers to COVID-19.
Institutional responses to the risk of coronavirus:
As soon as the first cases of COVID-19 appeared in Mali, the change in the status of the hospital as a center for the management of the disease caused "fear, stress, panic, and even constraint" among the caregivers. Some expressed, "I am afraid not to get the disease and contaminate my family". The facility did not receive any official notification to be designated as a care or diagnostic center. The caregivers were not sufficiently prepared at the beginning, and it was as the pandemic evolved that they received specific training on the disease. "As far as I am concerned, the coronavirus is an infectious disease but not like the others because there is no unanimous treatment.
In view of the lethality rate revealed by Media? to other countries/cities, the caregivers doubted the correct management of cases at our level. All of them affirmed that the hospital conveyed information about this disease, both about preventive measures and case management. "The most important communication in the face of the situation was the training of all staff on covid-19, and then the information and exchange meetings of the members of the EIR.
The organization and the means implemented:
Faced with a suspected and probable case, physical distancing and containment; confirmed case, isolation and treatment. The COVID-19 protocol was in line with the department's objectives. Biomedical waste management was carried out according to the following procedure: sorting, collection, treatment and disposal. The individual and collective protection means were insufficient at the beginning. Obtaining the result after a PCR (polymerase chain reaction) diagnostic test was always difficult due to the waiting time of 2 to 5 days. This increased the stress for caregivers, patients and their families, especially if it preceded a death. Many said they assessed the risk/benefit through cure rates, preventive measures, and impact on hospital operations. Financial resources were insufficient for most caregivers: "We were given few gels and bibs per month".
In our context, commendable efforts have been made to facilitate the implementation of barrier measures in health facilities through the presence of functional hand-washing devices and the existence of specific garbage cans for the management of biomedical waste. It is therefore necessary to redirect actions by placing particular emphasis on IEC to improve compliance with barrier measures in the effective fight against VIDOC-19. Similarly, interdisciplinary and population-based collaboration would be necessary for behavior change with respect to barrier actions.
Staff reactions:
In a positive way, we noted an improvement in hygiene in general, with respect to barrier measures and the acquisition of new equipment by the structure, including respirators, oxygen extractors and multiparametric monitors.
On the other hand, the under-attendance of the establishment at the beginning of the pandemic due to the fear of getting sick led to a decrease in financial revenues. In the end, a huge dysfunction occurred with the breakdown of much equipment. "Each case is a sum of experiences, shared visions. As expressed by many caregivers, this experience allowed them to reflect on the modalities of care in an epidemic situation, on the reflexes to be integrated in front of the risk and on the possible constraints that could limit the full efficiency of the system already put in place by the administration.
4. Discussion
Our study was based on data collected from the nursing staff of the COVID-19 care center and from observation of the hospital environment. The average age was 42.3 ± 8.1 years. A total of 85.7% of the respondents were men, and 14.3% were women. This population consisted of 31% physicians/pharmacists, 47.6% nurses and 21.4% support staff. These results are higher than those found by NGOYI et al [12]. This could be explained by the difference between the two professional and academic groups. Health workers were the most affected (16.5%) and had easy access to information and testing services for COVID-19. The positivity rate in our study was 30.79% (97 cases/315 samples), comparable to that found by O Sangho et al. (30.90%). [It is higher than those found by Togola et al [14] and Moubarak Lo et al [15]. with 14.86% and 10-20%, respectively, but lower than that of Greffe, S et al [16]. with 38%. The detection rate was 2.56 ‰, which is comparable to that found by O Sangho et al [13] which would explain an under notification of cases due to the delay in the delivery of samples and the availability of results by the INSP (National Institute of Public Health), which was the reference laboratory located 380 kms from Sikasso. Thirty-six percent of positive patients (35/97) were treated at the treatment center, and 62 were treated as outpatients.
The majority of respondents had good knowledge of COVID-19. These results are similar to those found by other authors [17, 18], notably in the DRC, Uganda, Vietnam and China. This may be related in part to high exposure to information provided by the media and the awareness raised by the media since the spread of the virus. Media coverage may be considered an effective way to mitigate the spread of the disease [19].
The change in status of the hospital as a center for disease management has caused "fear, stress, panic" among caregivers. More than half of the respondents had no experience in managing epidemics. This inexperience supported fear, anxiety and even panic. In summary, the anticipation of the seriousness of the epidemic in terms of pulmonary prognosis led to two main types of decisions: measures to limit the spread of the virus via barrier measures (wearing masks, hand washing, confinement); a reorientation of care activities towards resuscitation and respiratory assistance practices, which required the mobilization of a considerable number of health care personnel and led, in parallel with the containment measures, to the cessation of a whole series of ambulatory or non-VIDOC-related activities [20].
Recently, Brooks et al. summarized these in the Lancet [21]. The review reports approximately twenty studies, mainly in Asian countries but also in Canada, Sweden and some African countries. In general, a negative psychological impact is described, with an increase in symptoms of acute stress, anxiety, dissociative confusion, anger and posttraumatic syndromes. Some studies have also reported long-term effects. In terms of the intensity of the consequences of confinement, these are more frequent when the quarantine is prolonged. P. SLOVIC has thus demonstrated that there was a very high correlation between the perception of the average incidence of risks and the frequency of their coverage in the press, so he could conclude that the media have a strong influence on collective beliefs in terms of health risks. 22] J. DELUMEAU has thus highlighted the continuities in the object of fears in the West. His study of epidemics over the centuries reveals the constancy of the episodes of collective panic that they provoke. This historically generalized anxiety may have been further aggravated by the fact that the re-emergence of infectious diseases has undermined Westerners' confidence in the ability of modern medicine to contain such epidemics [23]. Members of the rapid response team at one point felt isolated and ostracized. This feeling of isolation was less among physicians and among health care managers who participated in many meetings with teams from other departments. This result corroborates the finding of NICKELL and colleagues that "having a management or supervisory position reduces the likelihood of feeling isolated within the hospital during an outbreak." [24]
The change in the status of the hospital as a center for the management of the disease caused "fear, stress, panic and even constraint" among the caregivers. Subsequently, with media pressure and staff training, this fear gradually dissipated. Despite these fears and uncertainties expressed by the health care personnel, the hospital was able to carry out its missions and benefited from equipment and materials to fight COVID-19. This information is similar to that reported by Jenny et al [17]. during a study on Ebola: "In this respect, it has been shown that the appearance of the risk of Ebola has disrupted these social representations. At the same time, the organizational response resulting from the confrontation with the risk also contributed to destabilizing them. However, in regard to assessing the situation, once the risk has been integrated, it is clear that the normalization of the risk has helped to reinforce pre-existing representations.
"In the end, there is great uncertainty about the characteristics of the disease (number of reservoirs, transmission routes, incubation period, etc.) and the means to be deployed to address it (protective equipment, care protocols, etc.). Moreover, the Ebola epidemic was part of a particularly frightening frame of reference: that of the risk of spreading a fatal disease in a context of globalization. Although contemporary health crises no longer cause mass casualties as they did in the past, the frame of reference of a deadly crisis, such as the Black Death or the Spanish flu, in the case of Ebola, strongly structures the definition of a health crisis event. This feeling of unpreparedness, more or less strong depending on the services because of their own habits in taking care of patients suffering from an infectious disease, was exacerbated by anxiety-provoking media coverage of the epidemic, as our interviews showed.
It seems, therefore, that the global health crisis has exacerbated dysfunction at the hospital level among caregivers. It has, in this way, highlighted the differences between the health structures of the South and the North, including access to intensive care with adequate equipment and anti-COVID-19 vaccination coverage. The different efforts of preparation, training, communication and support in the care system have, at first, challenged some hospital routines by the implementation of new procedures, the drafting of protocols and the installation of new devices. This process of setting up the health response also highlighted the usual problems of hospital organization and was able to support certain classic claims of the various professionals.
Conclusion
This study has enabled us to analyze the hospital organization from its point of entry. It irrigated our reflection on different aspects of it, in particular its adaptability: the hospital structures, supported by the caregivers, were indeed reactive in the face of the health crisis constituted by the COVID-19 pandemic, despite the degree of uncertainty surrounding the modalities of care.
State of knowledge on the subject
- This phenomenon has been observed and documented in other health structures;
- The importance of individual and collective prevention means among health workers.
Contribution of our study to knowledge
- The impact of COVID-19 on the behavior and attitude of health care workers;
- The fear and anxiety reported by caregivers during COVID-19.
Acknowledgements
We would like to thank all the staff of the Sikasso Hospital and all the authors. All the authors contributed to the writing of this work. They also read and approved the final version of this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
List of Abbreviations:
RIT: Rapid Response Team
CAP: Knowledge attitude practices
PEC: Prise En Charge
DRS: Direction Régionale de la Santé (Regional Health Department)
ENT: Ear, Nose and Throat
References
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet (London, England) 395 (2020): 565-74.
- Zhang L, Shen FM, Chen F, Lin Z. Origin and evolution of the 2019 novel coronavirus. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America (2020).
- Perlman S. Another Decade, Another Coronavirus. New England Journal of Medicine 382 (2020): 760-2.
- Phelan AL, Katz R, Gostin LO. The Novel Coronavirus Originating in Wuhan, China: Challenges for Global Health Governance. Jama (2020).
- Ministry of Health and Social Development Communiqué No. 260 of 11/17/2020 on follow-ups of prevention and response actions to Coronavirus disease.
- MCINTOSH, Kenneth, BECKER, Walter B, and CHANOCK, Robert M. Growth in suckling-mouse brain of" IBV-like" viruses from patients with upper respiratory tract disease. Proceedings of the National Academy of Sciences of the United States of America 58 (1967): 2268.
- MAERTZDORF, Jeroen, WANG, Chiaoyin K., BROWN, Jennifer B., et al. Real-time reverse transcriptase PCR assay for detection of human metapneumoviruses from all known genetic lineages. Journal of clinical microbiology 42 (2004): 981-986.
- SIOW, Yaw L, GONG, Yuewen, AU-YEUNG, Kathy KW, et al. Emerging issues in traditional Chinese medicine. Canadian Journal of Physiology and Pharmacology 83 (2005): 321-334.
- GORSE, Geoffrey J, PATEL, Gira B, VITALE, Joseph N, et al. Prevalence of antibodies to four human coronaviruses is lower in nasal secretions than in serum. Clinical and Vaccine Immunology 17 (2010): 1875-1880.
- B Koné, AY Dembélé, SS Diarra, I Berthé, A Koné, A Boly et al. Clinical and epidemiological characteristics of COVID-19 deaths in Mali. MALI MEDICAL (2021).
- Jin JM, Bai P, He W, Wu F, Liu XF, Han DM, et al. Gender Differences in Patients With COVID-19: Focus on Severity and Mortality. Frontiers in Public Health 8 (2020).
- NGOYI, Jean M., KABAMBA, Léon N., TAMBWE, Pierre N., et al. Knowledge, attitudes and practices related to SARS-COV-2 (COVID-19) among students at the Institut Supérieur des Techniques Médicales de Lubumbashi. Rev l'Infirmier Congo 4 (2020): 8-12.
- G, F E, C D, S L, M S, B M. RT-PCR evaluation of nasopharyngealA? carriage of SARS-Cov-2 in symptomatic health care personnelA? suspected of COVID-19 in a suburban Parisian university hospital | Elsevier Enhanced Reader 41 (2020): 510-6.
- World Health Organization. COVID-19: Update on the situation in the WHO African Region (2021).
- World Health Organization (WHO). Regional Office for Africa Social and environmental factors considered to cause low COVID-19 levels in Africa. Available September 24, 2020 at: Social and environmental factors considered to be the cause of low COVID-19 levels in Africa | WHO | Regional Office for Africa (2020).
- Michel G. The irony of Corona: Covid-19 epidemic and development in Africa. The first 6 months. 271. FERDI 30 (2020).
- Kabamba LN, Kabamba MO, Mukonkole JN, Kabyla BL, Luboya ON. Knowledge, attitudes and practices of private pharmacy workers on covid-19: case of Kintambo commune in Kinshasa. Revue de l'infirmier congolais 4 (2020): 6-8).
- Zhang M, Zhou M, Tang F, Wang Y, Nie H, You G. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J Hosp Infect 105 (2020): 183-187.
- Zhou W, Wang A, Xia F, Xiao Y, Tang S. Effects of media reporting on mitigating spread of COVID-19 in the early phase of the outbreak. Mathematical Biosciences and Engineering 17 (2020): 2693-2707.
- Cohen Understanding COVID-19 as a child and adolescent psychiatrist; L'Encéphale 46 (2020): S99-S106
- Brooks SK, Webster RK, Smith LE, et al. The psycholo-gical impact of quarantine and how to reduce it: rapidreview of the evidence. Lancet 395 (2020): 912–20.