Peritoneal Carcinomatosis of Hepatocellular Carcinoma After Resection-Efficacy of Complete Surgical Resection with Hyperthermic Intraperitoneal Chemotherapy
Article Information
Juliette Boileve1, Pierrine Le Bras1, Frédéric Dumont2, Emilie Thibaudeau2, Jean-Luc Raoul1*
1Department of Medical Oncology, Institut de cancérologie de l’Ouest, Saint Herblain, France
2Department of Surgical Oncology, Institut de cancérologie de l’Ouest, Saint Herblain, France
*Corresponding Author: Jean-Luc Raoul, Department of Medical Oncology, Institut de cancérologie de l’Ouest, 44805 Saint Herblain, France
Received: 31 May 2020; Accepted: 08 June 2020; Published: 18 June 2020
Citation: Juliette Boileve, Pierrine Le Bras, Frédéric Dumont, Emilie Thibaudeau, Jean-Luc Raoul. Peritoneal Carcinomatosis of Hepatocellular Carcinoma After Resection-Efficacy of Complete Surgical Resection with Hyperthermic Intraperitoneal Chemotherapy. Journal of Surgery and Research 3 (2020): 135-138.
Share at FacebookKeywords
Hepatocellular carcinoma; Peritoneal carcinomatosis; Sorafenib; Peritonectomy; HIPEC
Hepatocellular carcinoma articles, Peritoneal carcinomatosis articles, Sorafenib articles, Peritonectomy articles, HIPEC articles
Hepatocellular carcinoma articles Hepatocellular carcinoma Research articles Hepatocellular carcinoma review articles Hepatocellular carcinoma PubMed articles Hepatocellular carcinoma PubMed Central articles Hepatocellular carcinoma 2023 articles Hepatocellular carcinoma 2024 articles Hepatocellular carcinoma Scopus articles Hepatocellular carcinoma impact factor journals Hepatocellular carcinoma Scopus journals Hepatocellular carcinoma PubMed journals Hepatocellular carcinoma medical journals Hepatocellular carcinoma free journals Hepatocellular carcinoma best journals Hepatocellular carcinoma top journals Hepatocellular carcinoma free medical journals Hepatocellular carcinoma famous journals Hepatocellular carcinoma Google Scholar indexed journals Peritoneal carcinomatosis articles Peritoneal carcinomatosis Research articles Peritoneal carcinomatosis review articles Peritoneal carcinomatosis PubMed articles Peritoneal carcinomatosis PubMed Central articles Peritoneal carcinomatosis 2023 articles Peritoneal carcinomatosis 2024 articles Peritoneal carcinomatosis Scopus articles Peritoneal carcinomatosis impact factor journals Peritoneal carcinomatosis Scopus journals Peritoneal carcinomatosis PubMed journals Peritoneal carcinomatosis medical journals Peritoneal carcinomatosis free journals Peritoneal carcinomatosis best journals Peritoneal carcinomatosis top journals Peritoneal carcinomatosis free medical journals Peritoneal carcinomatosis famous journals Peritoneal carcinomatosis Google Scholar indexed journals Sorafenib articles Sorafenib Research articles Sorafenib review articles Sorafenib PubMed articles Sorafenib PubMed Central articles Sorafenib 2023 articles Sorafenib 2024 articles Sorafenib Scopus articles Sorafenib impact factor journals Sorafenib Scopus journals Sorafenib PubMed journals Sorafenib medical journals Sorafenib free journals Sorafenib best journals Sorafenib top journals Sorafenib free medical journals Sorafenib famous journals Sorafenib Google Scholar indexed journals Peritonectomy articles Peritonectomy Research articles Peritonectomy review articles Peritonectomy PubMed articles Peritonectomy PubMed Central articles Peritonectomy 2023 articles Peritonectomy 2024 articles Peritonectomy Scopus articles Peritonectomy impact factor journals Peritonectomy Scopus journals Peritonectomy PubMed journals Peritonectomy medical journals Peritonectomy free journals Peritonectomy best journals Peritonectomy top journals Peritonectomy free medical journals Peritonectomy famous journals Peritonectomy Google Scholar indexed journals fibrotic liver articles fibrotic liver Research articles fibrotic liver review articles fibrotic liver PubMed articles fibrotic liver PubMed Central articles fibrotic liver 2023 articles fibrotic liver 2024 articles fibrotic liver Scopus articles fibrotic liver impact factor journals fibrotic liver Scopus journals fibrotic liver PubMed journals fibrotic liver medical journals fibrotic liver free journals fibrotic liver best journals fibrotic liver top journals fibrotic liver free medical journals fibrotic liver famous journals fibrotic liver Google Scholar indexed journals oxaliplatin articles oxaliplatin Research articles oxaliplatin review articles oxaliplatin PubMed articles oxaliplatin PubMed Central articles oxaliplatin 2023 articles oxaliplatin 2024 articles oxaliplatin Scopus articles oxaliplatin impact factor journals oxaliplatin Scopus journals oxaliplatin PubMed journals oxaliplatin medical journals oxaliplatin free journals oxaliplatin best journals oxaliplatin top journals oxaliplatin free medical journals oxaliplatin famous journals oxaliplatin Google Scholar indexed journals lung metastases articles lung metastases Research articles lung metastases review articles lung metastases PubMed articles lung metastases PubMed Central articles lung metastases 2023 articles lung metastases 2024 articles lung metastases Scopus articles lung metastases impact factor journals lung metastases Scopus journals lung metastases PubMed journals lung metastases medical journals lung metastases free journals lung metastases best journals lung metastases top journals lung metastases free medical journals lung metastases famous journals lung metastases Google Scholar indexed journals resection margins articles resection margins Research articles resection margins review articles resection margins PubMed articles resection margins PubMed Central articles resection margins 2023 articles resection margins 2024 articles resection margins Scopus articles resection margins impact factor journals resection margins Scopus journals resection margins PubMed journals resection margins medical journals resection margins free journals resection margins best journals resection margins top journals resection margins free medical journals resection margins famous journals resection margins Google Scholar indexed journals prognosis articles prognosis Research articles prognosis review articles prognosis PubMed articles prognosis PubMed Central articles prognosis 2023 articles prognosis 2024 articles prognosis Scopus articles prognosis impact factor journals prognosis Scopus journals prognosis PubMed journals prognosis medical journals prognosis free journals prognosis best journals prognosis top journals prognosis free medical journals prognosis famous journals prognosis Google Scholar indexed journals
Article Details
1. Case Report
The incidence of Hepatocellular carcinoma (HCC) is increasing worldwide. HCC usually complicates an underlying chronic liver disease. Due to advances in the treatment of chronic liver disease, and the increase in non-alcoholic steatohepatitis (HCC usually arises before cirrhosis), many HCC cases are not currently associated with a decompensated cirrhosis of the liver at diagnosis [1]. In recent years, the therapeutic armamentarium has expanded and this increase in treatment options requires cooperation between physicians for efficient management of these patients such as with dedicated multidisciplinary tumor boards [2]. HCC metastasizes late and infrequently; and usually affects the bones, lungs, lymph nodes, and adrenal glands. Isolated peritoneal metastases are an uncommon presentation and are mainly observed after spontaneous tumor rupture, biopsy or tumor resection, when they can be rapidly fatal. We report a case of a peritoneal carcinomatosis that developed after resection of HCC. This case benefited from a treatment of Sorafenib, allowing complete surgical resection associated with a hyperthermic intraperitoneal chemotherapy (HIPEC) and favorable outcome.
In 2016, a very large right liver tumor mass was detected by an ultrasound exam in a 63-year-old man experiencing dysuria. Liver and tumor biopsies confirmed the diagnosis of HCC arising in a mildly fibrotic liver. Liver function tests and AFP serum levels were normal and except alcoholism, no other aetiology could be found. In December 2016, the patient underwent an uncomplicated right hepatectomy. A pathological exam demonstrated a 115 mm, well- differentiated tumor of axis HCC, with microscopic vascular emboli, and borders 1 mm adjacent to Glisson’s capsule. The peritumoral liver had minimal fibrosis (Figure 1). In October 2017, 11 months later, a CT scan revealed multiple peritoneal nodules (>10, ranging from 5 to 30 mm in size) predominantly close to the liver resection margin (Figure 1) and also along the right colon and the omentum. After ruling out intrahepatic recurrence by MRI, treatment with Sorafenib (Nexavar™) at 800 mg/day was initiated. Four months later, the nodule size and vascularization had decreased (Objective Response) (Figure 2). A complete surgical resection with HIPEC was then performed in April 2018. Intra-operatively, a dozen tumor nodules were found on the omentum, appendix, right colon, and near the resection margin. The peritoneal carcinomatosis index (PCI) was evaluated at 7. After a complete cytoreduction (CCR 0), HIPEC using oxaliplatin at 42°C was administered for 30 min. No adverse events were noticed and the patient was discharged on day 9. Sorafenib was not resumed post- operatively. In May 2019, 13 months after the HIPEC, a CT scan did not detect intra-abdominal recurrence however 6 small (less than 1 cm) lung metastases were identified. Sorafenib was reintroduced and 12 months later (May 2020), 32 months after the initial diagnosis of intra-abdominal recurrence, the metastases were controlled.
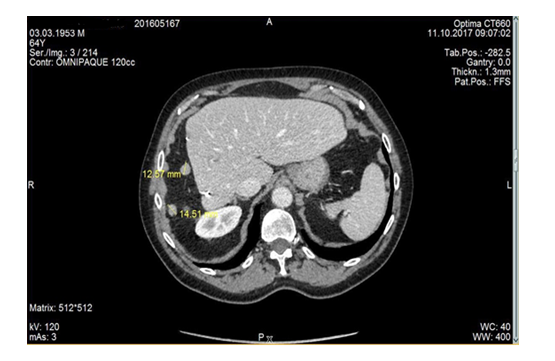
Figure 1: CT scan at diagnosis: small peritoneal nodules near surgical margin in left upper quadrant.
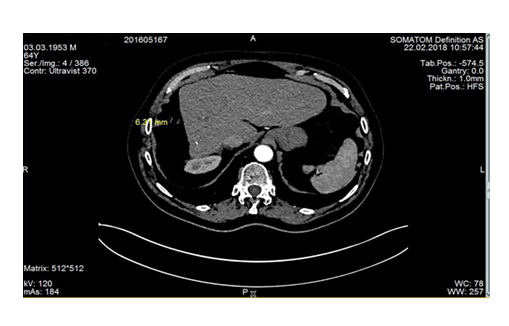
Figure 2: Decrease in size and in vascularization of these nodules after 4 months of sorafenib 800 mg/d.
2. Discussion
This case raises some issues regarding peritoneal carcinomatosis complicating HCC. The first question concerns the risk factors of developing peritoneal carcinomatosis particularly after liver resection for HCC. Usually, cases are described after tumor rupture, major tumor invading the capsule, or after biopsy or surgical resection. In a large series of 1222 hepatectomies performed in Seoul, 36 patients (3%) developed peritoneal carcinomatosis [3]. The major risk factors were tumor size over 5 cm, presence of microvascular invasion, and positive resection margins, consistent with the findings in our patient [3]. The prognosis of peritoneal carcinomatosis complicating HCC is not well known and depends largely on the global picture. A series of 53 patients from Taiwan (10 synchronous and 43 metachronous peritoneal carcinomatosis) demonstrated that the median overall survival (mOS) of those treated by surgical resection was greater than those who received only chemotherapy (12.5 vs 2.1 months), however liver function was the most significant prognostic factor [4].
Only patients who could benefit from resection of the carcinomatosis exhibited favorable outcomes, including survival more than 5 years after resection. In an American series of 22 HCC patients with peritoneal carcinomatosis who underwent complete surgical resection, including 5 with additional HIPEC, the mOS was close to 2 years [5]. In appreciation of the aggressiveness of this recurrence, our patient received Sorafenib [6] as a first-line treatment. Partial response under Sorafenib, as observed here, is infrequent in medical series (2%) [6], but is always associated with a favorable prognosis (mOS of 47 months in one series) [7]. Taking this into account, we considered that a surgical option to remove all peritoneal deposits was possible in this patient with a minor liver disease.
Reports of cytoreductive surgery followed by HIPEC for peritoneal carcinomatosis of HCC are infrequent in the literature and are mostly found in case reports; however, there exist two studies of 14 and 21 patients respectively [8, 9]. A study from New York reported 14 cases (10 without cirrhosis and 4 with Child-Pugh A cirrhosis; 13 post-operative recurrences) treated by cytoreductive surgery (mean PCI 9.9), with 7 of these receiving additional HIPEC treatment using Mitomycine C. Complete cytoreduction was achieved in 13 cases. Post-operatively one patient died (PCI 33). Metachronous peritoneal recurrence occurred after a median of 23 months, mOS for CCR 0-1 was 35.6 months. The second series was multinational and reported 21 cases (median age: 46 years) in 25 years from 10 reference centers [8]. The median PCI was 14; the surgery was completed in 16 cases (CCR 0-1); 5 different chemotherapy agents were used (cisplatin, mitomycine D, adriamycin, oxaliplatin and irinotecan); 10 had severe (grade 3-4) adverse events, and mOS of CCR0-1 patients (over 5 years) was not reached while for CCR2-3 this mOS was 5.9 months.
We posit that complete surgical resection followed by hyperthermic intraperitoneal chemotherapy must be considered for patients with a good performance status, without decompensated cirrhosis, and with a low PCI. This combination may allow for a longer survival. Preoperatively, a neoadjuvant period of systemic treatment could allow for better candidate selection for this surgery.
References
- European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol 69 (2018): 182-236.
- Raoul JL, Faivre S, Frenel JS, et al. Medical oncologists must get more involved in systemic treatment. Ann Oncol 30 (2019): 6-8.
- Kow AW, Kwon CH, Song S, et al. Risk factors of peritoneal recurrence and outcome of resected peritoneal recurrence after liver resection in hepatocellular carcinoma: review of 1222 cases of hepatectomy in a tertiary institution. Ann Surg Oncol 19 (2012): 2246- 2255.
- Lin CC, Liang HP, Lee HS, et al. Clinical manifestations and survival of hepatocellular carcinoma patients with peritoneal metastasis. J Gastroenterol Hepatol 24 (2009): 815-820.
- Berger Y, Spivack JH, Heskel M, et al. Extrahepatic metastasectomy for hepatocellular carcinoma: Predictors of long-term survival. J Surg Oncol 114 (2016): 469-474.
- Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 359 (2008): 378-390.
- Raoul JL, Adhoute X, Penaranda G, et al. Sorafenib: Experience and Better Manage- ment of Side Effects Improve Overall Survival in Hepatocellular Carcinoma Patients: A Real- Life Retrospective Analysis. Liver Cancer 8 (2019): 457-467.
- Mehta S, Schwarz L, Spiliotis J, et al. Is there an oncological interest in the combination of CRS/HIPEC for peritoneal carcinomatosis of HCC? Results of a multicenter international study. Eur J Surg Oncol 44 (2018): 1786-1792.
- Tabrizian P, Franssen B, Jibara G, et al. Cytoreductive surgery with or without hyperthermic intraperitoneal chemotherapy in patients with peritoneal hepatocellular carcinoma. J Surg Oncol 110 (2014): 786-790.
