Peripherally Inserted Central Catheters and Upper Extremity Deep Venous Thrombosis: Incidence and Risk Factors
Article Information
Osama Batayneh1*, Ratib Mahfouz1, David Rabinovich1, Hadeel Zainah2
1Department of Internal Medicine, Kent County Memorial Hospital, Brown University, Rhode Island, United States
2Department of Internal Medicine, Division of Infectious diseases, Kent County Memorial Hospital, Rhode Island, United States
*Corresponding author: Osama Batayneh, Department of Internal Medicine, Kent-County Hospital, Brown University, Rhode Island, United States
Received: 05 February 2022; Accepted: 15 February 2022; Published: 02 March 2022
Citation:
Batayneh O, Mahfouz R, Rabinovich D, Zainah H. Peripherally Inserted Central Catheters and Upper Extremity Deep Venous Thrombosis: Incidence and Risk Factors. Archives of Internal Medicine Research 5 (2022): 71-076.
Share at FacebookAbstract
Introduction: Peripherally inserted central catheters (PICCs) are becoming increasingly popular due to their ease of insertion through upper extremity veins, although they are not complications-free. PICCs can be irritating and cause endothelial injury and inflammation resulting in deep venous thrombosis (DVT). Estimates suggest that more than a third of all DVT in the upper extremities is caused by PICCs. This research highlights the incidence of upper extremity DVT in patients with PICCs and the relation with other comorbidities.
Methods: A retrospective matched cohort was cond- conducted at a community hospital. The records of 438 patients were reviewed from 2017 to 2020. Subjects were at least 18 years old, underwent PICC insertion, and received outpatient parenteral antibiotic therapy (OPAT). The data included demographics and comorbidities, such as hypertension (HTN), diabetes mellitus (DM), chronic kidney disease (CKD), coronary artery disease (CAD), congestive heart failure (CHF), active malignancy, previous DVT, and concomitant anticoagulation. The DVTs were confirmed by doppler ultrasound.
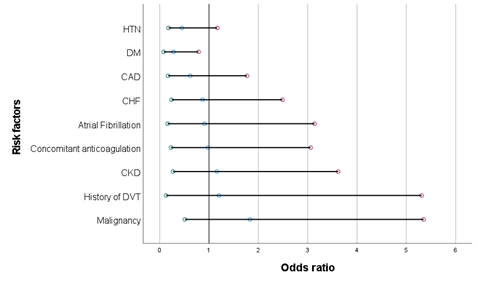
Results: DVTs were diagnosed in 24 patients (5.7%). The average age was 64.9 years. Seventeen (70%) patients were males and 24 (100%) were white. The median time to diagnosis was 21 days from PICC insertion. Patients with DM were 72% less likely to be diagnosed with DVT compared to those without diabetes (OR = 0.28, P= 0.008). There was no relation between the diagnosis of DVT and the other comorbidities, including HTN (OR = 0.45, P = 0.059), CAD (OR = 0.62, P = 0.353), CHF (OR = 0.87, P = 0.79), Afib (OR = 0.91, P = 0.589), concomitant anticoagulation (OR = 0.98, P = 0.62), CKD (OR = 1.16, P = 0.725), malignancy (OR = 1.83, P = 0.242), and previous DVT (OR = 1.2, P = 0.763). Age was not associated with higher risk of DVT (OR=1.6, P = 0.304).
Conclusion: The risk of DVT w
Keywords
Peripherally Inserted Central Catheters, Deep Venous Thrombosis, Upper Extremity
Article Details
1. Introduction
Peripherally inserted central catheters (PICCs) have been popularly used since the 1980s. PICCs play a major role for patients as they serve as central venous access for antibiotics and chemotherapy agents during long-term drug therapy [1]. According to a recent analysis, PICCs are inserted in approximately 5 million people annually in the United States [2]. PICC is a thin and long flexible catheter made of biocompatible material, inserted percutaneously into the basilic or cephalic vein in the forearm or the antecubital fossa, often with the help of an ultrasound or fluoroscopy, the catheter is then advanced into the central circulation [3].
PICCs have become more popular and a very good alternative intravenous (IV) access for central lines due to its different advantages, including the easy insertion, short procedure time, few complications and the high rate of patient satisfaction [4, 5]. Although PICCs have brought numerous benefits, there are some potential complications, including deep venous thrombosis (DVT), infection, mecha-nical failure (migration, obstruction), and few others [6, 7]. Here in this study, we discuss the incidence of upper extremity (UE) DVT in patients with PICCs, and the significance and clinical correlation of some associated chronic comorbidities.
2. Materials and Methods
This study is a retrospective matched cohort, cond-ucted at a 343-bed community hospital in Rhode Island between January 2017 and December 2020. The IRB committee approved the protocol. The study goal was to find out the incidence of UE DVT in patients with PICCs, along with the relation of the clinical characteristics.We identified patients who received antibiotics through PICCs in our outpatient parenteral antibiotic therapy (OPAT) program. Those patients were discharged from the hospital with PICCs or received PICCs in the outpatient setting; and had received antibiotics for a period of 4 - 6 wee-ks for various infections.Duplex ultrasound results were reviewed to identify the patients with DVT. UE venous duplex scans were ordered for all patients who exhibited any signs or symptoms concerning for UE DVT including swelling, pain, redness around the PICC, fever, chills, or PICC malfunction.
An electronic medical record query was performed to identify all the patients meeting inclusion criteria. The patients were included if they were > 18 years old, had a PICC, and received IV antibiotics for a total of 4 - 6 weeks. Patients with superficial throm-bosis or thrombosis in another site were excluded. The incidence of PICC-associated UE DVT was calculated using simple statistics. The median time for UE DVT after PICC placement was calculated. Univariable analysis was used to determine if some comorbidities were associated with UE DVT. The level of significance was determined using P value of <0.05. Patients with PICC-associated UE DVT were compared with a control group of patients with PICCs but without UE DVT.
Analysis was done with statistical analysis system software. The clinical variables evaluated included age, gender, race, active malignancy, anticoagulation use before PICC insertion, prior history of DVT, hypertension (HTN), diabetes mellites (DM), chronic kidney disease (CKD), coronary artery disease (CAD), congestive heart failure (CHF) and atrial fibrillation (Afib). Results are presented as odds ratios (ORs) with 95% confidence intervals (CIs). Patients with confirmed PICC-associated UE DVT were referred to the emergency department (ED) for further evaluation and management. Subsequently, the number of PICCs removed along with treatment with anticoagulation were calculated.
3. Results
During the 4-year period, we reviewed the charts of 862 patients seen in the outpatient clinic, 438 patients with PICCs were followed in the OPAT program. UE DVT was diagnosed in 24 patients (5.47%).The median time to diagnosis was 21 days from PICC insertion. In patients who developed PICC-associated UE DVT, 4 patients (16%) were receiving thera-peutic dose of anticoagulation before the diagnosis of DVT. Once the DVT was diagnosed, patients were referred to the ED for further evaluation and management. All PICCs were removed in the ED after DVT diagnosis. We found that 30-day-mortality rate was zero.
Table 1 lists baseline characteristics for all study patients. The mean age for patients with UE DVTs and without DVTs was 64.88, and 65.69 years respectively (P= 0.389). For those with DVT, 17 patients (70.83%) were males and 24 (100%) were white. Patients with DM were 72% less likely to be diagnosed with DVT compared to those without diabetes (OR = 0.28, P= 0.008). There was no relation between the diagnosis of DVT and the other comorbidities, including HTN (OR = 0.45, P =0.059), CAD (OR = 0.62, P = 0.353), CHF (OR = 0.87, P = 0.79), Afib (OR = 0.91, P = 0.589), concomitant anticoagulation (OR = 0.98, P = 0.62), CKD (OR = 1.16, P = 0.725), malignancy (OR = 1.83, P =0.242),or previous DVT (OR = 1.2, P = 0.763). Furthermore, age was not associated with higher risk of DVT (OR=1.6, P = 0.304).
Table 2 lists univariable analysis of the clinical characteristics for both groups (PICCs with UE DVT, PICCs without DVT). A significant lower incidence of UE DVT was seen in patients with DM (OR=0.28, P= 0.008). A statistically non-significant lower UE DVT incidence was seen in patients with HTN (OR= 0.45, P= 0.059), CAD (OR= 0.62, P = 0.353), CHF (OR = 0.87, P= 0.79), Afib (OR= 0.91, P = 0.589), and concomitant anticoagulation (OR = 0.98, P = 0.62). A statistically non-significant higher UE DVT incidence was seen in patients with CKD (OR = 1.16, P = 0.725), malignancy (OR = 1.83, P =0.242), and previous DVT (OR = 1.2, P = 0.763).
|
DVT 24 No. (%) |
No DVT 414 No. (%) |
P-Value |
||
|
Average Age (year) |
64.88 |
65.69 |
0.389 |
|
|
Gender |
Male |
17 (70.83) |
249 (60.14) |
0.304 |
|
Race |
White |
24 (100) |
402 (97.10) |
0.855 |
|
Other |
0 |
12 |
||
Table 1: Baseline characteristics for all patients involved in the study.
|
DVT 24 No. (%) |
No DVT 414 No. (%) |
Odds Ratio (OR) |
Confidence intervals (CIs) |
P-Value |
|
|
HTN |
14 (58.33) |
313 (75.60) |
0.45 |
0.18 - 1.17 |
0.059 |
|
DM |
5 (20.83) |
201 (48.55) |
0.28 |
0.08 - 0.79 |
0.008 |
|
CAD |
5 (20.83) |
123 (29.71) |
0.62 |
0.17 - 1.77 |
0.353 |
|
CHF |
5 (20.83) |
96 (23.19) |
0.87 |
0.24 - 2.49 |
0.79 |
|
Atrial Fibrillation |
3 (12.5) |
56 (13,53) |
0.91 |
0.16 - 3.14 |
0.589 |
|
Previous anticoagulation |
4 (16.67) |
20 (4.83) |
0.98 |
0.23 - 3.06 |
0.62 |
|
CKD |
4 (16.67) |
61 (14.73) |
1.16 |
0.27 - 3.62 |
0.725 |
|
History of DVT |
2 (8.33) |
29 (7.0) |
1.2 |
0.13 - 5.31 |
0.763 |
|
Malignancy |
5 (20.83) |
52 (12.56) |
1.83 |
0.51 - 5.35 |
0.242 |
Table 2: Univariable analysis of clinical characteristics for both groups.
4. Discussion
There were two main purposes for this study. The first was to assess the frequency of DVT in patients who had PICCs in the upper extremity. In this regard, the incidence was 5.47% (24/438); this was similar to a previous study in Spain which showed an incidence of 4.9% for catheter related thrombosis [8]. The second aim was to evaluate which comorbidities would affect the incidence of DVT. In that vain, there were three notable comorbidities that increased the odds of DVT (but not statistically significant), active cancer (OR 1.83, P = 0.242), CKD (OR 1.16, P = 0.725), and previous DVT (OR 1.2, P = 0.763). Nevertheless, among these three factors, active can-cer did appear to be the most impactful on the risk of developing DVT.
On the other hand, there were some unexpected findings. Diabetes mellitus was found to have a lower association with DVT (OR 0.28, P = 0.008). This finding is not supported by previous literature. In fact, a previous study has shown results suggestive of higher incidence of DVT in diabetic patients [9]. There were other variables that also showed a negative correlation with DVT including hyper-tension (OR 0.45, P = 0.059), CAD (OR 0.62, P = 0.353), CHF (OR 0.87, P = 0.79), AFib (OR 0.91, P = 0.589), and previous anticoagulation (OR 0.98, P = 0.62), but this association was not statistically significant. An earlier study showed that preexisting diagnosis of hypertension, malignancy, and CKD were all independent risk factors for developing UE DVT [10]. The reason as to why patients in the current study who had diabetes or hypertension were less likely to develop DVT is unclear. Perhaps they were taking medications that prevented DVT, such as an antiplatelet drug. Further research should be undertaken to analyze the effect of diabetes and hypertension on DVT risk before any strong conclusions are made.
Finally, there have been studies investigating the use of anticoagulation to prevent central venous catheter-related thrombosis. One of which is a meta-analysis which included 15 randomized controlled trials. It showed anticoagulation to be effective in decreasing the risk of both symptomatic and asymptomatic central line-associated DVT (RR 0.31 – 0.73). However, that was not the case for symptomatic DVT alone (RR 0.28 – 0.72) [11]. Our study has some limitations related to the retrospective nature, inclu-ding the unmeasured variables, and the control selection bias. Furthermore, our study is a single center study, had a small sample size, and at risk for recordkeeping and reviewing errors.
5. Conclusion
The risk of DVT in this study was 5.7 % in patients who had PICCs. There was less risk of DVT in patients with diabetes mellitus, while there was no risk association with the other comorbidities.This study could serve as a step to further to evaluate PICC-related DVTs and the associated risk factors. Further prospective studies or clinical trials are needed in this area before any strong conclusion can be made.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- Baxi SM, Shuman EK, Scipione CA, et al. Impact of postplacement adjustment of peripherally inserted central catheters on the risk of bloodstream infection and venous thrombus formation. Infect Control Hosp Epidemiol 34 (2013): 785-792.
- Deshmukh M, Shinde M. Impact of structured education on knowledge and practice regarding venous access device care among nurses. Int J Sci Res 3 (2014): 895-901.
- Johansson E, Hammarskjöld F, Lundberg D, et al. Advantages and disadvantages of peripherally inserted central venous catheters (PICC) compared to other central venous lines: A systematic review of the literature. Acta Oncologica (2013): 886-892.
- Cotogni P, Barbero C, Garrino C, et al. Peripherally inserted central catheters in non-hospitalized cancer patients: 5-year results of a prospective study. Support Care Canc 23 (2015): 403-409.
- Liem TK, Yanit KE, Moseley SE, et al. Peripherally inserted central catheter usage patterns and associated symptomatic upper extremity venous thrombosis. J Vasc Surg 55 (2012): 761-767.
- Chopra V, Anand S, Krein SL, et al. Bloodstream infection, venous thrombosis, and peripherally inserted central catheters: reappraising the evidence. Am J Med 125 (2012): 733-741
- Bertoglio S, Faccini B, Lalli L, et al. Peripherally inserted central catheters (PICCs) in cancer patients under chemotherapy: a prospective study on the incidence of complications and overall failures. J Surg Oncol 113 (2016): 708-714.
- Iriondo J, Iñarra O, Sarriegui B, et al. Peripherally Inserted Central Catheter (PICC) Related Deep Venous Thrombosis: A Retrospective Cohort Study on Incidence and Risk Factors in a Single Center. Blood 136 (2020): 30-31.
- Petrauskiene V, Falk M, Waernbaum I, et al. The risk of venous thromboembolism is markedly elevated in patients with diabetes. Diabetologia 48 (2005): 1017-1021.
- Tohme S, Vancheswaran A, Mobbs K, et al. Predictable Risk Factors of Upper-Extremity Deep Venous Thrombosis in a Level I Trauma Center. International Journal of General Medicine 14 (2021): 2637-2644.
- Kirkpatrick A, Rathbun S, Whitsett T, et al. Prevention of Central Venous Catheter-Associated Thrombosis: A Meta-analysis. The American Journal of Medicine 120 (2007): 901.e1-13.