Observers’ Perspectives on Virtual Reality Reducing Responsive Behaviours in Dementia: An Interpretive Description
Article Information
M Sultana1, 2*, M Jennings1, G Teachman3, D Bryant4, K Campbell5, J Knowlton6, A St. George7, M Montero-Odasso1,2, JB Orange8
1Health and Rehabilitation Sciences, Western University
2Parkwood Institute, London, ON, Canada
3School of Occupational Therapy, Western University, London, ON, Canada
4School of Physical Therapy and Schulich School of Medicine & Dentistry (Orthopaedic Surgery), Western University, London, ON, Canada
5International Skin Tear Advisory Panel, Canada
6Primacare Living Solutions Inc.™, Toronto, ON, Canada
7Crosswater Digital Media, US
8School of Communication Science and Disorders and Canadian Centre for Activity and Aging, Western University, London, ON, Canada
*Corresponding Author: M. Sultana, Health and Rehabilitation Sciences, Western University, Canada.
Received: 11 April 2022; Accepted: 29 April 2022; Published: 03 May 2022
Citation: M Sultana, M Jennings, G Teachman, D Bryant, K Campbell, J Knowlton, A St. George, M Montero-Odasso, JB Orange. Observers’ Perspectives on Virtual Reality Reducing Responsive Behaviours in Dementia: An Interpretive Description. Journal of Psychiatry and Psychiatric Disorders 6 (2022): 110-127.
Share at FacebookKeywords
Responsive behaviours in Dementia; Interpretive description; Virtual Reality; Long-term care home
Responsive behaviours in Dementia articles; Interpretive description articles; Virtual Reality articles; Long-term care home articles
Responsive behaviours in Dementia articles Responsive behaviours in Dementia Research articles Responsive behaviours in Dementia review articles Responsive behaviours in Dementia PubMed articles Responsive behaviours in Dementia PubMed Central articles Responsive behaviours in Dementia 2023 articles Responsive behaviours in Dementia 2024 articles Responsive behaviours in Dementia Scopus articles Responsive behaviours in Dementia impact factor journals Responsive behaviours in Dementia Scopus journals Responsive behaviours in Dementia PubMed journals Responsive behaviours in Dementia medical journals Responsive behaviours in Dementia free journals Responsive behaviours in Dementia best journals Responsive behaviours in Dementia top journals Responsive behaviours in Dementia free medical journals Responsive behaviours in Dementia famous journals Responsive behaviours in Dementia Google Scholar indexed journals Interpretive description articles Interpretive description Research articles Interpretive description review articles Interpretive description PubMed articles Interpretive description PubMed Central articles Interpretive description 2023 articles Interpretive description 2024 articles Interpretive description Scopus articles Interpretive description impact factor journals Interpretive description Scopus journals Interpretive description PubMed journals Interpretive description medical journals Interpretive description free journals Interpretive description best journals Interpretive description top journals Interpretive description free medical journals Interpretive description famous journals Interpretive description Google Scholar indexed journals Virtual Reality articles Virtual Reality Research articles Virtual Reality review articles Virtual Reality PubMed articles Virtual Reality PubMed Central articles Virtual Reality 2023 articles Virtual Reality 2024 articles Virtual Reality Scopus articles Virtual Reality impact factor journals Virtual Reality Scopus journals Virtual Reality PubMed journals Virtual Reality medical journals Virtual Reality free journals Virtual Reality best journals Virtual Reality top journals Virtual Reality free medical journals Virtual Reality famous journals Virtual Reality Google Scholar indexed journals Long-term care home articles Long-term care home Research articles Long-term care home review articles Long-term care home PubMed articles Long-term care home PubMed Central articles Long-term care home 2023 articles Long-term care home 2024 articles Long-term care home Scopus articles Long-term care home impact factor journals Long-term care home Scopus journals Long-term care home PubMed journals Long-term care home medical journals Long-term care home free journals Long-term care home best journals Long-term care home top journals Long-term care home free medical journals Long-term care home famous journals Long-term care home Google Scholar indexed journals Psychological Symptoms of Dementia articles Psychological Symptoms of Dementia Research articles Psychological Symptoms of Dementia review articles Psychological Symptoms of Dementia PubMed articles Psychological Symptoms of Dementia PubMed Central articles Psychological Symptoms of Dementia 2023 articles Psychological Symptoms of Dementia 2024 articles Psychological Symptoms of Dementia Scopus articles Psychological Symptoms of Dementia impact factor journals Psychological Symptoms of Dementia Scopus journals Psychological Symptoms of Dementia PubMed journals Psychological Symptoms of Dementia medical journals Psychological Symptoms of Dementia free journals Psychological Symptoms of Dementia best journals Psychological Symptoms of Dementia top journals Psychological Symptoms of Dementia free medical journals Psychological Symptoms of Dementia famous journals Psychological Symptoms of Dementia Google Scholar indexed journals audio-recorder articles audio-recorder Research articles audio-recorder review articles audio-recorder PubMed articles audio-recorder PubMed Central articles audio-recorder 2023 articles audio-recorder 2024 articles audio-recorder Scopus articles audio-recorder impact factor journals audio-recorder Scopus journals audio-recorder PubMed journals audio-recorder medical journals audio-recorder free journals audio-recorder best journals audio-recorder top journals audio-recorder free medical journals audio-recorder famous journals audio-recorder Google Scholar indexed journals transcriptionist articles transcriptionist Research articles transcriptionist review articles transcriptionist PubMed articles transcriptionist PubMed Central articles transcriptionist 2023 articles transcriptionist 2024 articles transcriptionist Scopus articles transcriptionist impact factor journals transcriptionist Scopus journals transcriptionist PubMed journals transcriptionist medical journals transcriptionist free journals transcriptionist best journals transcriptionist top journals transcriptionist free medical journals transcriptionist famous journals transcriptionist Google Scholar indexed journals Image articles Image Research articles Image review articles Image PubMed articles Image PubMed Central articles Image 2023 articles Image 2024 articles Image Scopus articles Image impact factor journals Image Scopus journals Image PubMed journals Image medical journals Image free journals Image best journals Image top journals Image free medical journals Image famous journals Image Google Scholar indexed journals Registered Nurses’ Association of Ontario articles Registered Nurses’ Association of Ontario Research articles Registered Nurses’ Association of Ontario review articles Registered Nurses’ Association of Ontario PubMed articles Registered Nurses’ Association of Ontario PubMed Central articles Registered Nurses’ Association of Ontario 2023 articles Registered Nurses’ Association of Ontario 2024 articles Registered Nurses’ Association of Ontario Scopus articles Registered Nurses’ Association of Ontario impact factor journals Registered Nurses’ Association of Ontario Scopus journals Registered Nurses’ Association of Ontario PubMed journals Registered Nurses’ Association of Ontario medical journals Registered Nurses’ Association of Ontario free journals Registered Nurses’ Association of Ontario best journals Registered Nurses’ Association of Ontario top journals Registered Nurses’ Association of Ontario free medical journals Registered Nurses’ Association of Ontario famous journals Registered Nurses’ Association of Ontario Google Scholar indexed journals dementia articles dementia Research articles dementia review articles dementia PubMed articles dementia PubMed Central articles dementia 2023 articles dementia 2024 articles dementia Scopus articles dementia impact factor journals dementia Scopus journals dementia PubMed journals dementia medical journals dementia free journals dementia best journals dementia top journals dementia free medical journals dementia famous journals dementia Google Scholar indexed journals
Article Details
1. Introduction
Responsive behaviours associated with dementia are also known as Behavioural and Psychological Symptoms of Dementia (BPSD) [1]. BPSD include but are not limited to symptoms such as apathy, depression, agitation, aggression, sleep disorders, and psychosis [1]. Depression and apathy are common in vascular dementia [2]. Frontotemporal dementia typically presents with gross decline in behaviours and speech/language [3] with disinhibition and eating disturbances being common [2]. In Alzheimer's dementia, delusion is common [2]. Responsive behaviours worsen as dementia progresses [4] intensifies caregiver distress [5], and thereby accelerates the decision to institutionalize the individuals with dementia [6]. Responsive behaviours can harm (physical injuries, emotional trauma, and death) the individual exhibiting the behaviours, his/her caregivers, and people cohabitating with him/her [7-9]. Caregivers are at a higher risk of being physically and emotionally harmed as responsive behaviours are reported to manifest more during direct care such as toileting, bathing, mouth care, feeding, and dressing [10, 11]. The Registered Nurses’ Association of Ontario (RNAO) [12] recommended non-pharmacologic interventions to manage responsive behaviours for individuals with dementia, irrespective of drug treatments received [12]. The Virtual Reality (VR) experience is considered as a non-pharmacologic intervention [13]. We conducted a pilot study on the feasibility of VR as a non-pharmacologic intervention during November 2018-January 2019 [14]. We noticed several changes in the residents during and after the VR intervention, previously not identified as possible study outcomes. We realized that a qualitative study might unlock previously unknown effects of VR intervention useful for future clinical interventions for persons living with dementia. The pilot study provided VR intervention with BroomX© (https://broomx.com/) consisting of a MK Player360© hardware and a software. A MK Player360© is a projection device with light and sound control displaying 3600 videos on a frameless screen (e.g. a room) (Figure 1).

Figure 1: Immersive experience with Broomx©. Reprinted from “MKplayer360+” by Broomx Technologies, 2022.
One of the authors (ASG) created a customized library of images and music for the pilot to be accessed by a smartphone app. We provided the VR intervention for 30 minutes, five days a week (Monday to Friday) for two weeks either in a predetermined intervention area or in the residents' own room depending on their mobility status. Residents experienced images such as Cherry Blossom (an afternoon stroll in the park with blooming cherry flowers set to soft classical music), Farm (morning walk in a farmyard with cows and chicken set to animal and bird sound), Truck driving (day time simulated driving in the country roads), Symphony (a concert playing classical music), London, UK (aerial view of city streets and iconic building in London, UK set to soft classical music), Bavarian Alps (a morning stroll in the alpine meadow set to bird sound), Fishing (simulated fishing in the river set to water sound), Dolphin Swim club (simulated under water diving set to water sound), Ireland (aerial view of city streets and iconic building in Ireland set to soft classical music). Boat ride (a simulation of riding a boat along the river), Dream beach (image of sandy beach), and Sun and clouds (image of daytime sky).
To understand the usefulness of the inquiry, we searched databases such as PubMed, Scopus, Psych Info (search phrase was virtual reality AND dementia AND qualitative research with no limiting criteria) and retrieved 12 papers (qualitative inquiry [n=10], review article [n=2]). Out of 10 qualitative inquiries, one was a conference proceeding, one was written in Spanish language, one did not use VR as intervention, and one used VR intervention for family caregivers. One of the co-authors (JBO) provided one related study [15]. Based on these papers [15-20], we concluded that an inquiry into caregiver and family’s perception of the VR experience was likely to produce new and necessary information about VR intervention (Table 1: Available qualitative research on virtual reality and dementia published in English). We also learned that no other peer-reviewed published qualitative inquiries currently exist on VR intervention with BroomX© in nursing home residents with moderate to severe dementia.
|
Reference |
Participants |
Intervention |
Method |
Results |
Implications |
|
Appel et al., [15] |
Older adults with cognitive impairment (n=66) |
Single visit 20-minute nature scene provided with headset |
Mixed-method study |
Caregivers reported participants being more relaxed during the experience |
The technology is feasible. However, a better picture quality and an accompanying audio file may improve the experience |
|
Baker et al., [16] |
Residential aged care facility members (n=5) and staff (n=5) |
Two-week virtual experience with headset |
Qualitative interviews |
Virtual experience can play a role in engaging residents who might otherwise self-isolate |
The technology is feasible. Headset can create a potential negative impact on those living with dementia |
|
Ferguson, Shade, Boron, Lyden, & Manley, [17] |
Hospice patients living with dementia (n=25) |
A single visit 30-minute YouTube Video of a beach scene using a headset |
Narrative inquiry |
Four themes: narration (commented about their experience), affirmation (enjoyed or was appreciative of the experience), comfort level (headset too tight, headache, dizziness, nausea), and unfulfilled (was bored watching the same scene for a long time) |
Realization of a need for a devise for comfortable experience, and an inquiry into caregiver and family’s perception of the experience |
|
Rose, Stewart, Jenkins, Tabbaa, Ang, & Matsangidou, [18] |
People with mild to moderate dementia (n=8) living in an inpatient Psychiatric Care setting |
Virtual experience (5 still images) for 15 minutes, once a week for two weeks with headset |
Mixed-method study |
The participants had a positive virtual experience and described their experience as a good “change in environment” |
Realization of a need for a wide variety of images to keep the participants engaged |
|
Moyle, Jones, Dwan, & Petrovich, [19] |
People with dementia (n=10) from two nursing homes, their family members (n=10), and nursing home staff (n=9) |
One session of a single virtual image |
Mixed-method study |
Virtual experience improved the awareness and mood of people with dementia |
Setting up the machine was time consuming and needed clutter free space. Keeping participants engaged more than 10 minutes was challenging |
|
Martinez-Pernia et al., [20] |
Clinician-patient dyad (n=16) |
A simulated game (making tea) |
Case study |
Users accepted the technology |
The technology can be used as a neuropsychological assessment tool |
|
McEwen, Taillon-Hobson, Bilodeau, Sveistrup, & Finestone, [21] |
A person with dementia and his caregiver |
1 hour driving simulation, 5 days a week for 2 weeks provided with a headset |
Case study |
Caregiver reported the user being attentive to his daily activities. However, the headset agitated the user |
People with dementia may tolerate this technology |
Table 1: Available qualitative research on virtual reality and dementia published in English.
The objective of the current study was to explore the experiences of observers positioned to witness the pilot participants’ behaviour during the pilot study. The qualitative inquiry was conducted three months (April 2019) after the pilot study. We refer to the participants with moderate to severe dementia who completed the pilot study of VR intervention as “residents”.
2. Materials and Method
2.1 Design and theoretical framework
While social sciences capitalize on health phenomena to answer elemental questions related to core features of human experiences, health sciences pay attention to solving everyday health and wellness issues of individuals or to understanding the effect of a particular health intervention [22]. We realize that the interpretation of our observers’ observations/experiences was subjective and was open to multiple meanings co-constructed by us and the observers. Our knowledge was generated through a logical relationship and accommodation of multiple perspectives of various people relating to a single phenomenon (VR intervention). We did not bracket our thoughts and perceptions, rather participated actively to co-construct knowledge. Our observers did not experience VR, rather they observed the VR study participants (i.e., residents). Their accounts were based on their observations, experiences, and perceptions shaped by their relationship with the residents, their professional stances, and their subjective values. Our study was based on an actual real-world question (what are the experiences/observations/perceptions of individuals with VR intervention positioned to observe pilot participants?). Therefore, we declare our approach to be interpretive description in congruence with health sciences. Interpretive description is a constructivist qualitative research approach adapting available design techniques suitable to answer a practical health research question regardless of methodological eclecticism [23]. During a post-pilot meeting, study site personnel (administrative staff and pilot researchers) shared their own observations of residents' behaviour changes, previously not identified as a possible outcome. Despite our belief in the objective reality of VR effect, we acknowledge the existence of multiple realities. With this in mind, we wanted to conduct a qualitative inquiry into this pilot study.
2.2 Sample and setting
Any sample size is acceptable to conduct interpretive description [23]. The purposive sample size for this study was 15. We recruited family members, nursing home staff (personal support workers and registered nurses), and pilot researchers as observers for this study because we were interested to understand the phenomenon from multiple opposing/endorsing accounts. We were cognizant of the concept of epistemic injustice, conversations and dementia [24], thus reflected carefully on including in the interviews residents who completed the pilot VR intervention study. However, the residents’ moderate to severe cognitive status prevented their ability to provide a direct account of their observations/experiences with VR.
2.3 Recruitment
We approached the principal investigator of the pilot study to identify possible observers following the protocol approved by local ethics board. The eligibility criteria we used to identify possible observers were 1) family members who visited the participating residents either before, during, or after VR intervention sessions; 2) staff members (personal support workers and registered nurses) who were included in participating residents’ circle of care before, during, or after VR intervention sessions; and 3) researchers who implemented the pilot study and had opportunity to observe the residents experiencing VR intervention. After receiving the contact information of the possible observers (family members [n=24], staff [n=7], researchers [n=3]), one of us (MS) contacted the observers by telephone calls, e-mail, or in-person. We did not, however, contact family members of deceased residents (n=3) to avoid causing any pain while remembering their loved ones or their responses to the VR intervention. Five of the twenty-four family members agreed to participate in an interview. The study site had restrictions on sharing their staff’s personal contact information. The staff observers were recruited at their workstation during their lunch break. Five out of seven staff’s work schedule was busy. The nursing home administration agreed to cover one hour of their work schedule with another staff. Thus, all contacted staff (n=7; personal support workers n=6, registered nurse n=1) participated in this qualitative inquiry. Three VR pilot researchers agreed to participate, two of them were registered nurses and one of them worked as an administrator at the nursing home.
2.4 Data collection: Interviews
We interviewed the observers during the month of May (7-27) of 2019. They provided written consent for the interviews. Since this study was an amendment to the earlier pilot, we applied to the same ethics board for approval. The author (MS) disclosed her constructivist position and her affiliation prior to each interview. The interviews were conducted in a manner that was open and where questions did not lead the observers to provide specific types of information. The interviews were conducted in a quiet room away from the residents’ living area inside the nursing home. Each interview was approximately one-hour duration. The author (MS) acknowledges that she is not a native speaker of English and that she is not in the position to understand the full spectrum of contextual Canadian vocabulary. Therefore, she (MS) requested that the observers repeat their words and to clarify what they meant in cases where they used phrases, idioms and culturally dependent words during the interviews. No observer was interrupted while he/she was speaking and larger gaps were left for them to continue speaking following Green and Thorogood’s [25] recommendations. All interviews were recorded to optimize the accuracy of data collection. Two audio-recorders (TASCAM digital voice recorder, DR-05V2 170620 and Sony Digital Voice Recorder, ICDUX560BLK) were used at the same time to avoid accidental loss of interview data from any unforeseen technical difficulties. The interview started with an open-ended question enquiring about the observer’s perception on residents’ experiences with the VR intervention. The author (MS) engaged with the observers using prompts where necessary (e.g., please explain with an example). The audio files were saved with a unique code and stored in an encrypted Google Drive folder in keeping with the approved ethics protocol for data security. A professional transcriptionist transcribed orthographically and verbatim each interview. Only the transcriptionist and the author (MS) had access to the audio files. The author (MS) reviewed the transcript data against the audio data word-for-word. No revisions were required.
2.5 Data collection: Observations
To understand the contextual environment of a nursing home, we paid attention to the surrounding physical, cultural, and emotional settings. The author (MS) recorded in writing in the field notes her interpretations of the nursing home environments (i.e., physical and social), and social interactions among the staff members. She also recorded aspects of non-verbal communication (e.g. nodding, gesturing, frowning, and facial expression during the interviews) and observers’ comments related to VR experience outside the interview recording period (e.g. conversation during recruitment period, before and after recording of the interviews) in the field notes. She constantly checked her field notes against the interview data to reflect on any other possible interpretation of her initial understanding.
2.6 Quality of data
According to Thorne [23], the evaluative criteria for data quality typical in interpretive description are 1) epistemological integrity, 2) representative credibility, 3) analytic logic, and 4) interpretive authority.
2.7 Epistemological integrity
To achieve epistemological integrity, the research question must be consistent with the stated epistemological standpoint and the interpretation of data sources must follow that question [23]. Our research question invited multiple co-constructed reality. The data interpretations were rooted in the constructivist stance to attain epistemological integrity.
2.8 Representative credibility
Representative credibility can be achieved by sampling individuals positioned to observe/experience a phenomenon from multiple angles of vision [23]. We invited three groups (family, staff, researchers) for interviews who were positioned to observe the residents who participated in the VR pilot study from multiple perspectives to achieve representative credibility.
2.9 Analytic logic
A qualitative investigator can never assure the reader of an exhaustive inductive reasoning [26]. Instead, evidence of a sufficiently visible inductive reasoning throughout the work enabling the reader either to confirm or to reject its credibility can be labelled as analytic logic [23, 26]. In health sciences, intellectual audit trails (i.e., investigator reflects on how his/her thinking evolved throughout the work) and/or thick description (i.e., grounding interpretive claims in verbatim accounts/illustrative material visualizing the context) often are used to achieve analytic logic [27-30]. We described our reflections throughout the work to acquire intellectual audit trails and presented relevant verbatims to capture thick description, ultimately to achieve analytic logic.
2.10 Interpretive authority
Reflexive accounts of the investigator revealing his/her own biases or experiences to help the reader separate the subjective truth from the shared truth can achieve the interpretive authority [31-33]. We attempted to achieve sufficient clarity by aiding the readers to distinguish the author’s constructs from co-constructs which, in turn, helped attain interpretive authority.
2.11 Data analysis
In interpretive description, the investigator must see beyond the obvious, rigorously deconstruct his/her own understanding of data, and take ownership over the potential meaning and impact of the interpretation of subjective constructs [23]. What we consider meaningful is based on our personality, experiences, disciplinary orientation, biases, and curiosities. Therefore, co-author (MJ) from another disciplinary orientation (Physiotherapy) analyzed independently the transcript data. Authors (MS, MJ) discussed their interpretations to understand if one of them was missing any construct or interpreting any construct differently. The co-author (MJ), however, did not use author (MS)’s field notes when analyzing the transcript data to avoid being biased from her reflections and to help the readers see beyond author’s perceptions following Thorne’s [23] work. According to Bailey (2008), relying entirely on transcript data is a potential risk of losing insight arising from the nuances, pauses, tone and deliverance of informants’ discourse. We used the recorded interviews, transcripts, and field notes when analyzing the data to avoid this potential pitfall. We used NVivo© software (QSR International Incorporation [34]) to help us organize the data. We used thematic content analysis approach defined as “a method for identifying, analyzing and reporting patterns within data” [35]. Thematic content analysis allows a rich, detailed and complex description of data without following a certain theoretical framework [35], applicable for the current study. This type of analysis is a useful method for examining the perspectives of different research informants, generating unanticipated insights, and summarizing key features of a large data set [35] and is frequently used in interpretive description approach [23].
2.12 Sorting and organizing data
Thorne [23] cautions against overenthusiasm for data management software as these software programs may overshadow an investigator’s intelligence and inductive thinking. We initially coded the texts as a single unified data set. (i.e., sentences/paragraphs instead of words) based on their relatedness to an idea. We used NVivo© software to select sentences or sections of the text data as codes. After coding the texts, we organized the relevant codes into nodes based on their relatedness with each other, our interpretation of those utterances, and emotional/cultural/behavioural constructs attached to them recorded in the field notes. NVivo© software permits a user to create a separate file called nodes (a collection of codes) (QSR International Incorporation, [34]). The author (MS) also recorded her reflexive accounts from her field notes in marginal memos connected to the nodes.
2.13 Making sense of patterns
Thematic analysis in health sciences involves an iterative reasoning process to gradually come to understand the implications of constructs and to align investigator’s own ideas with those constructs [36]. Keeping in mind the objective of this inquiry, we identified which nodes addressed similar ideas and aligned our reflexive notes with those nodes to create “parent nodes” using NVivo©. The authors (MS, MJ) read the “parent nodes” identified by each other to help themselves perceive the pattern of ideas in a different perspective and re-evaluated the “parent nodes”.
2.14 Transforming pattern into themes
A theme gives meaning to data and helps to understand the "big picture" as per the investigator's judgement [36]. Themes in interpretive description are rigorously thought-through conceptualization of data patterns focused to the objective of the study [23]. The entire dataset was read and re-read to understand whether the pattern of ideas identified reflected the larger dataset and whether they were related to the study objectives. The iterative process of transforming patterns into themes is presented in Figure 2 (Data analysis process). The co-author (MJ) reviewed critically the themes the author (MS) identified against the themes she identified. Their (MS, MJ) interpretations were comparable. The relationships of the themes were re-evaluated and revised accordingly.
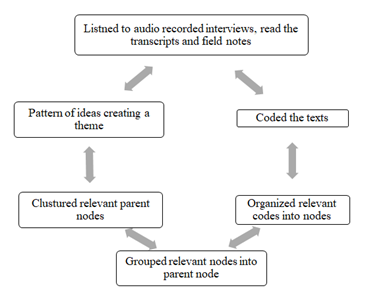
Figure 2: Data analysis process.
3. Results
After critically sorting and organizing data, we identified 56 nodes and 19 parent nodes (Table 2: Sorting and organizing coded data) before collapsing them into four themes focused to the objective of this inquiry (experience with VR intervention).
|
Themes (n=4) |
Parent nodes (n=19) (Sub-themes) |
Nodes (n=56) |
|
A noticeable change in the residents |
Communication |
Interacting with other residents and staff, finding words, showing caring side of their personality, spoke in a positive way, able to carry on conversation longer, listens to the conversation, responds better |
|
Demeanour |
Stopped rubbing hands, calling out less, smiling more, more understanding, listening to radio again, played with grandson again, started noticing her stuffs brought from home |
|
|
Being relaxed |
Completing 30-minute session, less restless, falling less, sleeping during the intervention |
|
|
Attention |
Paying attention to virtual reality (VR) images, paying attention to surrounding environment, paying attention to the researcher |
|
|
Being active |
Willingly dressing themselves in nicer outfits, not resisting baths, taking care of their personal belongings, coming out of the room more often |
|
|
Eating behaviour |
Eating better, not eating while wandering, eating being seated |
|
|
Implementation challenges of VR in a nursing home setting |
Library items |
Responded to familiar images, specific images brought back negative memories, tailoring library item, confusion regarding space and time |
|
Duration of intervention |
Duration of intervention needs to be longer, effect depended on duration of intervention, can be a regular intervention |
|
|
Flexibility |
Schedule needed to account for regular activities, intervention schedule needed to account for residents’ mood |
|
|
Staff dependency |
Staff education on VR intervention, staff are overwhelmed, staff involvement in measuring pilot outcomes |
|
|
Staff commitment |
Willingness to maintain VR machine, willingness to learn how to operate VR machine, time commitment to conduct VR intervention |
|
|
Intervention area |
A dedicated intervention area, setting VR machine at residents’ room is impractical, VR machine setting time upset residents, background noise interrupted resident’s attention |
|
|
Technical issues |
Use of a headset was impractical, disinfecting protocol for headset was time consuming, interrupted internet (Wi-Fi) connection, VR app control |
|
|
Uniqueness of the VR intervention |
Almost real, suggestions for future |
Feels so real, treated patients as a person, can be a recreational activity |
|
Duration of VR effect |
Is there a long-term effect? |
A lingering effect for months, reverted back to old self after intervention stopped, not sure if the effect was due to VR |
Table 2: Sorting and organizing coded data.
The four themes identified in our interpretive description are: 1) a noticeable change in the residents, 2) implementation challenges of VR intervention in a nursing home setting, 3) uniqueness of the VR intervention, and 4) duration of VR effect. A selection of supporting quotes for each theme are outlined in Table 3.
|
Theme |
Key supporting quote |
|
A noticeable change in the residents |
“Resident X’s son really noticed a difference with his mom because he was able to sit and have a conversation with her. Before she wouldn’t sit. She would not sit for five seconds and now she’s sitting and she’s talking about cows.” (Staff) |
|
Implementation challenges of VR in a nursing home setting |
“The other challenge that we had was all the paperwork and questionnaires… it was a lot of paper trail and expectations for the staff or one of the behaviour mod staff to assist us with those questionnaires.” (Researcher implementing the intervention) |
|
Uniqueness of the VR intervention |
“It was individual, it was about them, it was special.” (Staff) |
|
Duration of VR effect |
“There was sort of an after effect, a lingering effect, that occurred. People were calmer and more focused. The dietician commented on somebody we would feed sandwich to while they were wandering, … She said when the VR stopped that resident continued to be able to sit at the table and eat.... so that’s a big difference there and it didn’t just stop when the VR stopped.” (Staff) |
Table 3: Themes with supporting quotes.
3.1 Theme 1: A noticeable change in the residents
All observers mentioned noticing at least one behavioural change in residents who completed the VR intervention.
Sub-theme 1: Communication
Observers mentioned that the residents started to speak, to make gestures attracting attention or to respond to verbal communication, and to show interest in initiating and continuing a conversation. We spotted at least nine residents in common from the accounts of the observers who were communicating better after receiving the VR intervention. The following quote shows how striking this “change” was: We had a resident who hadn’t been verbal in over a year. All of a sudden, started talking about the cows and her family called me because when the family would come to visit, they said my mother hasn’t talked in over a year and why is she talking about cows, where are these cows? I said, well you know you consented your mother to be in our VR study and she has been having daily VR sessions with the farm scene and it clicked with the family right away (Researcher implementing the intervention).
Sub-theme 2: Demeanour
Many observers mentioned a change in residents’ typical demeanour during and after (more or less two months) the pilot. A family member experienced an emotional turmoil when describing her mother. She asked the author (MS) if family members in her culture send their parents to nursing homes. Our understanding was that she felt somewhat guilty for not being able to take care of her mother at home. She was upset, crying at times during the interview. The family member mentioned that her mother used to rub her own hands during a conversation whenever she visited her, sensing that something was bothering her mother. She reported that when she was a little girl, she remembered that her mother used to rub her own hands if there was a tension in the relationship between her parents. The family member stated that her father was an alcoholic and abusive towards her mother. She used to think that her mother was not happy being away from her. She stated that she felt that rubbing hands was her mother’s way of showing being upset. She noticed that her mother stopped rubbing her hands while she participated in the pilot. She reported, however, that her mother started massaging her own hands again two months after the VR pilot ended.
Sub-theme 3: Being relaxed
Observers described a change in residents’ anxious behaviours/uneasiness. Staff observers noted to the author (MS) that the residents with moderate to severe dementia usually do not sit in a place for long. They either wander or simply lose interest in any conversation/audio-visual experience. For example, when one of us (MS) was waiting in a TV area near the nursing station to recruit a staff informant for this study, she noticed that there were only four residents sitting in front of the TV. Two of them were fast asleep and two of them were immobile. Those not sleeping were not watching TV. One resident was looking out the window and another was looking at people passing by. When observers mentioned residents being relaxed, being seated in a chair, and actually watching VR images for 30 minutes, we took these remarks seriously. In our interpretation, being relaxed is a noticeable change. We didn’t expect that they would sit for 30 minutes through a VR session and a lot of residents did. Not everyone but a lot of residents did and that was kind of surprising (Researcher implementing the intervention).
Sub-theme 4: Attention Observers mentioned residents being attentive to their surrounding environment, to their activities of daily living, and to their conversations.
Sub-theme 5: Being active
We learned from several observers that residents were active during VR intervention in terms of willingly dressing themselves, not resisting baths, and taking care of their personal belongings.
Sub-theme 6: Eating behavior
Observers described a single resident showing a considerable change in her eating behaviour. According to the observers, the resident used to wander around the facility, did not sit in the dining area long enough to finish her meal, and did not sit down while eating in her own room prior to being enrolled in and completing the pilot VR study. When the same resident was in the pilot study, she actually ate meals while seated in the dining area and gained weight. However, the calm demeanour reverted to restlessness after the pilot ended.
3.2 Theme 2: Implementation of VR in a nursing home setting.
Sub-theme 1: Library items
In our judgement, a majority of the observers believed a tailored VR library based on family members’ feedback was useful in drawing residents’ attention to the VR experience. For example, residents having experience in farming responded better with the library item, “Farm”, whereas, residents passionate about driving repeatedly watched the library item, “Truck driving”. Notably, library items revealed some aspects of residents’ memory/reaction to a memory previously unknown/forgotten over time. For example, a family member mentioned that a staff (personal support worker) asked her whether her mother had any traumatic memory related to the image of an Alpine meadow. She could not think of anything that might frighten her mother watching a peaceful image of a meadow. The family had immigrated to Canada from England after World War II. She discussed this incident with her older sister living in England. Her older sister remembered that her mother used to work as a nurse during World War II near the Bavarian Alps. Her older sister also remembered that her mother used to tell stories about people being killed in the meadows of Bavaria. She discovered a possible reason for her mother’s reaction to a seemingly peaceful image of the library item, “Bavaria”. We believe such experience is a lesson for those interested in implementing VR intervention for older adults with dementia.
Sub-theme 2: Duration of VR intervention
We acknowledge a consensus among the observers regarding the duration of VR intervention. According to the observers, a two-week long duration of VR intervention is not sufficient to affect residents’ responsive behaviours, let alone have a sustained effect.
Sub-theme 3: Flexibility in scheduling VR intervention
We realized from the two months observation of the environment and workplace culture at the study site and the interviews that any intervention concerning older adults with dementia in nursing home setting needs flexible scheduling. In our understanding, an individual with dementia may be overwhelmed cognitively, physically or sensorially on a particular day to complete a visit. Therefore, someone interested in implementing similar intervention for people with dementia must follow a flexible schedule.
Sub-theme 4: Staff dependency
We sensed a tension between the staff members (personal support workers and registered nurses) at the study site and the researchers who implemented the VR pilot study from day 1 of our qualitative study. Staff observers mentioned that they were not paid enough to support a research study at the nursing home. Our understanding was that the VR pilot study incremented the stress of the staffs as the study related activities tightened their work schedule.
Sub-theme 5: Staff commitment
We realized that staff involvement is vital in implementing VR intervention in a nursing home setting during the interviews. Observers’ accounts revealed that they were well-positioned to motivate the residents to attend the intervention, to transfer residents to and from the intervention area, and to set up, to maintain, and to operate the VR machine.
Sub-theme 6: Intervention area
Observers mentioned the importance of a dedicated area for VR intervention in order to optimize a successful implementation. The VR machine (BroomX©) were often transported to residents’ rooms to avoid conflict with their daily schedule at the beginning of the pilot. Observers mentioned that setting BroomX© in residents’ room was impractical because (1) the VR image projection was often obstructed by wall decorations, (2) the VR sound was often interrupted by conversation among staff and residents in the hallway, (3) the VR experience was invariably shortened for machine set up time, and (4) the internet signal was often interrupted inside the living area of the residents. Further, the interrupted VR image and sound agitated the residents. According to observers, once a dedicated VR intervention area was established, the residents’ agitation was reduced.
Sub-theme 7: Technical issues
Observers mentioned several technical issues such as the use of a headset, disinfecting protocol before and after using the headset, interrupted internet (Wi-Fi) connection, and the VR app control. However, they solved all of those issues when they started using a projector, a land line for internet, and a dedicated space for intervention.
3.3 Theme 3: Uniqueness of the VR intervention
One concept that surfaced repeatedly during the interviews was that the VR experience is a unique intervention and the nursing home should offer the intervention to all the residents on a regular basis. Observers also mentioned that a tailored VR library was the key to the unique VR experience. The following quote is an example of this perspective:
It is very individual, someone might be back in their childhood, someone might be back in their married life in their home, with their children, so that’s the piece for us is to figure out where people are and to connect with them at that level with the VR and so if that’s where people are, they are fighting the current environment, they fight today because they think they are living in 1940 or 1950 or wherever and so you remove that with the VR, put them where they are comfortable. So, they are calm, they are relaxed (Researcher implementing the intervention)
3.4 Theme 4: Duration of VR effect
Observers’ accounts revealed that the change in residents’ behaviours with VR intervention did not last long. The general consensus among the observers was that the VR effect lasted at least a week. Even though the observers mentioned that they noticed a change in residents for a week to months after pilot ended, they were not sure if that change was related to VR intervention or something else.
4. Discussion
Our position is simply to describe our interpretation of various subjective accounts on the same phenomenon (VR intervention). We recognize that observers positioned in various levels (some directly caring for the residents, some met residents only during the pilot study, and some are familiar with the residents long before living in a nursing home) interpret their perception based on their own mindset, their own professional stance, and their own cultural/spiritual beliefs. However, we recognize a probable truth amidst existing multiple truths that the intervention brought some kind of “change” in residents’ behaviour, their participation in daily activities, their mood, and their attention. We are not in the position to judge whether those “changes” were beneficial or detrimental for the residents.
The following section attempts to compare our interpretation with different studies having similar construct to aid the reader conceptualize how our findings are similar to or different from others. Similar to our interpretation, studies noted that individuals with dementia were engaged to VR technology [16-18, 20], were more relaxed during virtual experience [15], were aware of their surrounding environment [19], and were attentive to their daily activities [21]. Studies also echoed the informants’ perception related to the use of headset being uncomfortable [16, 17, 21] VR machine set-up being time consuming [19] and VR experience in a space with clutters, background noise, and bright light being challenging to keep the residents engaged [19]. Unlike this inquiry, they reported that the residents excitement declined after the first session as they lost interest over time watching the same image [18, 19], picture quality being not satisfactory [15], and lack of an accompanying audio file [15]
5. Translational Significance
Given the infancy of the research area, this interpretive description may ignite interest in someone involved in caring people with moderate to severe dementia to implement VR intervention. Although our findings applied to this particular study setting, the thick description related to VR experience, its implementation, and its effect on older adults with dementia represent an important first step in studying the effects of VR intervention in older adults with dementia.
6. Limitations
Achieving reflexivity was a challenge for the author (MS) because she is trained to explore reality with positivist lens. She adapted techniques such as referring back to her fieldnotes, involving two investigators in evaluating audio recorded interviews and transcript data to overcome this challenge. We realize that a video recorded interview instead of an audio recorded interview might have produced rich data in terms of capturing emotional aspects of informants’ accounts. Therefore, we declare thematic analysis based on audio recorded interview data and field notes (possible introduction of my preconceptions) as a limitation of this work.
Acknowledgements
Authors would like to acknowledge primacare Living Solutions Inc. ™ for allowing access to study protocol and data.
Declaration of interest
Ethics approval and consent to participate
The study was ethically approved by ADVARRA Canada Ethics board. The protocol number of this study is Pro00032743. The protocol can be accessed on https://www.cirbi.net with permission from the sponsor (primacare Living Solutions Inc. TM).
Consent for publication: All authors consent for publication and declare no conflict of interest.
Availability of data and material: Data are available from the authors upon reasonable request and with permission of primacare Living Solutions Inc. TM.
Funding
The study was funded by nonprofit external grant from the Centre for Aging and Brain Health Innovation as part of the Industry Innovation Partnership Program (I2P2) to the partners primacare Living Solutions Inc. ™ and Crosswater Digital Media, LLC. The funders supplied Broomx© (hardware and software) and paid the research staff for their time; the partner, primacare Living Solutions Inc. ™, provided space for the therapy, access to residents’ medical charts, and their staff in communicating, transferring, accompanying the residents and completing the outcome measures; and the other partner, Crosswater Digital Media, LLC., created library items for this study.
Authors’ Contributions
MS contributed in the conception, design, day-to day conduction, analysis, interpretation of data for the work, drafting the manuscript, and revising it critically for important intellectual content. MJ contributed in analysis, interpretation of data, and critical revision for the work. GT contributed in revising the work critically for important intellectual contents. DB, KC, MMO, AGS and JK contributed in critical revision of the work. JBO contributed in supervising MS in designing and analyzing of data for the work. JBO revised the work critically for important intellectual contents. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- O'Donnell BF, Drachman DA, Barnes HJ, et al. Incontinence and troublesome behaviors predict institutionalization in dementia. Journal of Geriatric Psychiatry and Neurology 5 (1992): 45-52.
- Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. British Medical Journal (2015).
- Onyike CU, Diehl-Schmid J. The epidemiology of frontotemporal dementia. International review of psychiatry (Abingdon, England). 25 (2013): 130-137.
- Stern Y, Mayeux R, Sano M, et al. Predictors of disease course in patients with probable Alzheimer's disease. Neurology 37 (1987): 1649-1653.
- Allegri RF, Sarasola D, Serrano CM, et al. Neuropsychiatric symptoms as a predictor of caregiver burden in Alzheimer's disease. Neuropsychiatric Disease and Treatment 2 (2006): 105-110.
- Steele C, Rovner B, Chase G A. et al. Psychiatric symptoms and nursing home placement of patients with Alzheimer's disease. The American Journal of Psychiatry 147 (1990): 1049-1051.
- Caspi, E. Aggressive behaviors between residents with dementia in an assisted living residence. Dementia 14 (2015): 528-546.
- Caspi E. Deaths as a result of resident-to-resident altercations in dementia in long-term care homes: A need for research, policy, and prevention. Journal of the American Medical Directors Association 17 (2016): 7-11.
- Shinoda-Tagawa T, Leonard R, Pontikas J, et al. Resident-to-resident violent incidents in nursing homes. The Journal of the American Medical Association, 291 (2004): 591-598.
- Lachs MS, Rosen T, Teresi JA, et al. Verbal and physical aggression directed at nursing home staff by residents. Journal of General Internal Medicine 28 (2013): 660-667.
- Morgan DG, Cammer A, Stewart NJ, et al. Nursing aide reports of combative behavior by residents with dementia: results from a detailed prospective incident diary. The Journal of the American Medical Association 13 (2012): 220-227.
- Registered Nurses’ Association of Ontario. Delirium, Dementia, and Depression in Older Adults: Assessment and Care (2nd ed.) Toronto, ON: Registered Nurses’ Association of Ontario (2016).
- D’Cunha NM, Nguyen D, Naumovski N, et al. A mini-review of virtual reality-based interventions to promote well-being for people living with dementia and mild cognitive impairment. Gerontology 65 (2019): 430-440.
- Sultana M, Campbell K, Jennings M, et al. Virtual Reality Experience Intervention May Reduce Responsive Behaviors in Nursing Home Residents with Dementia: A Case Series. Journal of Alzheimer's Disease (JAD) 84 (2021): 883–893.
- Appel L, Appel E, Bogler O, et al. Older adults with cognitive and/or physical impairments can benefit from immersive virtual reality experiences: A feasibility study. Frontiers in Medicine 6 (2020).
- Baker S, Waycott J, Robertson E, et al. Evaluating the use of interactive virtual reality technology with older adults living in residential aged care. Information Processing & Management 57 (2020).
- Ferguson C, Shade M, Boron BJ, et al. Virtual reality for therapeutic recreation in dementia hospice care: A feasibility study. American Journal of Hospice and Palliative Medicine (2020).
- Rose V, Stewart I, Jenkins KG, et al. Bringing the outside in: The feasibility of virtual reality with people with dementia in an inpatient psychiatric care setting. Dementia (London, England) (2019).
- Moyle W, Jones C, Dwan T, et al. Effectiveness of a virtual reality forest on people with dementia: A mixed methods pilot study. The Gerontologist 58 (2018): 478-487.
- Martinez-Pernia D, Nunez-Huasaf J, Del Blanco A, et al. Using game authoring platforms to develop screen-based simulated functional assessments in persons with executive dysfunction following traumatic brain injury. Journal of Biomedical Informatics 74 (2017): 71-84.
- McEwen D, Taillon-Hobson A, Bilodeau M, et al. Two-week virtual reality training for dementia: Single case feasibility study. Journal of Rehabilitation Research and Development. 51 (2014): 1069-1076.
- Alasuutari P. The rise and relevance of qualitative research. International Journal of Social Research Methodology 13 (2010): 139-55.
- Thorne S. Interpretive description: Qualitative research for applied practice 2nd ed. S. Thorne. (Ed.). New York, NY: Routledge (2016).
- Young JA, Lind C, Orange JB, et al. Expanding current understandings of epistemic injustice and dementia: Learning from stigma theory. Journal of Aging Studies 48 (2019): 76-84.
- Green J, Thorogood N. Qualitative methods for health research (4th ed). J. Green & N. Thorogood. (Eds). London: SAGE (2018).
- Morse JM. “Emerging from the data”: The cognitive process of analysis in qualitative inquiry. In J M Morse (Ed.) Critical issues in qualitative research methods Thousand Oaks, CA: Sage (1994): 23-43.
- Carcary M. The research audit trail: Enhancing trustworthiness in qualitative inquiry. The Electronic Journal of Business Research Methods 7 (2009): 11-24.
- Koch T. Establishing rigour in qualitative research: The decision trail. Journal of Advanced Nursing 53 (2006): 91-103.
- Ponterotto JG. Brief notes on the origins, evolution, and meaning of the qualitative research concept “thick description.” The Qualitative Report 11 (2006): 538-549.
- Sandelowski M. The problem of rigour in qualitative research. Advancing in Nursing Science 8 (1986).
- Altheide DL, Johnson JM. Criteria for assessing validity in qualitative research. In N. K. Denzin & Y. S. Lincoln (Eds.), Handbook of qualitative research. Thousand Oaks, CA: Sage (1994): 485-499.
- Paterson BL. A framework to identify reactivity in qualitative research. Western Journal of Nursing Research 16 (1994): 301-316.
- Schwandt TA. Farewell to criteriology. Qualitative Inquiry 2 (1996): 58-72.
- QSR International Incorporation. NVivo 12 Plus for Windows (2019).
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 3 (2006): 77-101.
- Miles MB, Huberman AM. Qualitative data analysis (2nd ed). Thousand Oaks, CA: Sage (1994).
- Bailey J. First steps in qualitative data analysis: Transcribing. Family Practice 25 (2008): 127-131.
