Not Every Wheeze is Asthmatic: An Aspiration Pneumonia Case Report
Article Information
Gabriel Melo Alexandre Silva1, Herbert Iago Feitosa Fonseca1, Pablo André Brito de Souza1, Ana Cássia Silva Oliveira1, Luciana Lopes Albuquerque da Nobrega2*
1Medical School, Federal University of Roraima, Boa Vista, RR, Brazil
2Medial Doctor, Pediatric Pulmonologist, Professor in Pediatrics, Federal University of Roraima, Boa Vista, RR, Brazil
*Corresponding Author: Luciana Lopes Albuquerque da Nobrega, Medical School of Roraima, Federal University of Roraima, Av. Capitão Ene Garcez, 2413, Boa Vista, RR, 69310-000, Brazil
Received: 01 April 2021; Accepted: 16 April 2021; Published: 03 May 2021
Citation: Gabriel Melo Alexandre Silva, Herbert Iago Feitosa Fonseca, Pablo André Brito de Souza, Ana Cássia Silva Oliveira, Luciana Lopes Albuquerque da Nobrega. Not Every Wheeze is Asthmatic: An Aspiration Pneumonia Case Report. Archives of Clinical and Medical Case Reports 5 (2021): 368-372.
Share at FacebookAbstract
Introduction: Wheezing in infants is an extremely common complaint, being markedly frequent in emergency services. Nonetheless, such a complaint is part of a wide spectrum of pathologies thus, demanding deeper investigation over the differential diagnosis must be addressed in an appropriate manner, in order to implement the necessary therapy as early as possible, and excessive intervention avoided, as much as possible Therefore, this case-report seeks to serve as a reminder of the importance of keeping a high suspicion on aspiration pneumonia even in previously healthy patients.
The Case: HPDJ, male, date of birth (Dec, 30th of 2019), then 10 months and 10 days old, enters the medical emergency service of the pediatric hospital on November, 10th of 2020, with a report of flu-like symptoms that persisted for 10 days. The possibilities of bronchiolitis, pneumonia and SARS-COV 2 are questioned given the pandemic context, therefore being approached with salbutamol and prednisolone, chest x-ray and complementary exams. The patient is hospitalized, under regimen of ceftriaxone, salbutamol and general symptomatic medication. The patient is discharged 6 days after the first hospitalization with recovered general condition and without adventitious sounds or pathological findings on auscultation, being referred to the pulmonology outpatient clinic of the pediatric hospital. During outpatient follow-up, the patient complains of a feverish respiratory condition, and then the possibility of aspiration by a foreign body was questioned. On Dec, 09th, foreign body is removed, with subsequent improvement of symptoms in 48 hours.
Conclusion: The maintenance of high clinical suspicion and attention to anamnesis are extremely important factors for the early diagnosis of less common causes of common complaints, such as aspiration of a
Keywords
Case Report; Pneumonia; Aspiration Pneumonia; Wheezing; Pneumology
Article Details
1. Introduction and Objectives
Wheezing in infants is an extremely common complaint, being markedly frequent in emergency services. Nonetheless, such a complaint is part of a wide spectrum of pathologies thus, demanding deeper investigation over the differential diagnosis and, therefore, must be addressed in an appropriate manner, with due attention to the semiological propaedeutics in order to implement the necessary therapy as early as possible, and excessive intervention avoided, as much as possible [1, 2].
Wheezing are adventitious sounds resulting from the involvement of small airways, either due to edema or mucous obstruction, being sounds in musical tones, of high frequency and predominantly expiratory, although they may have an inspiratory or biphasic nature in particular cases depending on the individual constitution of the patient and its correlation with the pathology [3]. Amongst the various causes of wheezing, there are bronchiolitis, asthma and pneumonias in their most diverse etiologies. Moreover, one must not neglect the possibility of involvement due to SARS-VOC 2 in the current pandemic scenario [4-6]. Therefore, this case-report seeks to serve as a reminder of the importance of keeping a high suspicion on aspiration pneumonia even in previously healthy patients.
2. The Case
HPDJ, male, date of birth (Dec, 30th of 2019), then 10 months and 10 days old, enters the medical emergency service of the pediatric hospital on November, 10th of 2020, with a report of flu-like symptoms that persisted for 10 days (mother associates current symptoms with child choking on bread). Mother reports having treated the child autonomously with amoxicillin + clavulanate for 8 days. Physical examination at the entrance presents axillar temperature of 36.6 ° C, in good general condition, tearful on examination, in moderate tachypnea, groaning, with diffuse rhonchi and wheezing, detailed auscultation was impaired by the child's crying. The possibilities of bronchiolitis, pneumonia and SARS-COV 2 are questioned given the pandemic context, therefore being approached with salbutamol and prednisolone, chest x-ray and complementary exams. Chest x-ray shows diffuse nonspecific infiltration, altered complementary exams are: alkaline phosphatase 311.54 mg / dl (ref 27.0-100.0 mg / dl), AST 59.17 UI/ml (16.0 - 52.0 UI/ml), CRP 37.75 mg/l (0.0-8.0 mg/l), SARS-COV-2 IGG (+) and IGM (-); Leukocytosis pattern (13.62 x 10 ^ 3/ml) at the expense of neutrophils (73.20%), with no reaction in platelet or red blood cell levels.
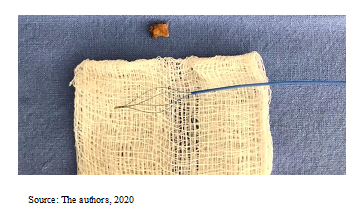
Given the situation, the patient is hospitalized, under regimen of ceftriaxone, salbutamol and general symptomatic medication. In the hospital bed, the pat.ient allows for a better examination, presenting slight rhonchi in left hemithorax. Patient thus progresses with emesis associated with feeding and the discharge of a greenish secretion. On the 12th, worsening of the general condition occurs, with the need for basal maintenance serum according to the Holiday-Segar rate, suspended on 14th. The patient is discharged 6 days after the first hospitalization with recovered general condition and without adventitious sounds or pathological findings on auscultation, being referred to the pulmonology outpatient clinic of the pediatric hospital. During outpatient follow-up, the patient complains of a feverish respiratory condition, and then the possibility of aspiration by a foreign body was questioned. Bronchoscopy performed on 12/02 reveals whitish aspirate in the left lower lobar bronchus, associated with edema aggravated by the presence of tweezers and aspiration, requiring a new clinical stabilization with antibiotic therapy corticosteroid pulse for 5 days. On reopening on Dec, 9th of 2020, a foreign body is removed (Figure 1), with subsequent improvement of symptoms in 48 hours
3. Discussion
Bronchial aspiration pneumonia is the pathology resulting from the invasion of the bronchoalveolar tree by solid or liquid foreign bodies, which can cause chemical damage or serve as a means of colonization and proliferation of infectious agents, with their mortality and morbidity strictly associated with the volume of aspirate, aggravating factors individual and evolution time [7]. Although it is much more incident and prevalent in hospitalized patients and with a comorbidity of a neurological nature, a previously healthy patient deserves this suspicion in the face of signs and symptoms of alarm such as: sudden onset dyspnea, crackles and wheezing located in a corresponding anatomical topography and fever without another suspicious focus, especially when you have gastroesophageal reflux disease, recent vomiting caused or not by food choking, alcoholism or seizure [8-10]. Several complications can be associated with the episode of aspiration pneumonia, such as pulmonary effusion, empyema, pulmonary atelectasis and in more severe cases, the development of respiratory failure. As a result of this potential complication, it is necessary to implement the appropriate therapy as early as possible, which often involves the removal of the foreign body whenever possible [7, 11-14].
4. Conclusion
The maintenance of high clinical suspicion and attention to anamnesis are extremely important factors for the early diagnosis of less common causes of common complaints, such as aspiration of a foreign body in the face of a wheezing complaint, thus avoiding prolonged and not fully effective treatments, which can put the child at risk for more severe complications and worse prognosis.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chong Neto H J, Rosário N A. Sibilância no lactente: Epidemiologia, investigação e tratamento. Jornal de Pediatria, 86 (2010): 171-178.
- Lustosa W A, Melo M L V, Isidório U de A, et al. Risk factors for recurrent wheezing in infants. Journal of Human Growth and Development 23 (2013): 203-208.
- Sarkar M, Madabhavi I, Niranjan N, et al. Auscultation of the respiratory system. Annals of Thoracic Medicine 10 (2015): 158-168.
- Al-Shamrani A, Bagais K, Alenazi A, et al. Wheezing in children: Approaches to diagnosis and management. International Journal of Pediatrics & Adolescent Medicine 6 (2019): 68-73.
- Parisi G F, Indolfi C, Decimo F, et al. COVID-19 Pneumonia in Children: From Etiology to Management. Frontiers in Pediatrics 8 (2020): 891.
- Sousa R B de, Medeiros D, Sarinho E, et al. Risk factors for recurrent wheezing in infants: A case-control study. Revista de Saúde Pública, 50 (2016).
- Toufen Junior C, Camargo F P de, Carvalho C R R. Pneumonia aspirativa associada a alterações da deglutição: Relato de caso. Revista Brasileira de Terapia Intensiva 19 (2007): 118-122.
- DeLegge M H. Aspiration pneumonia: Incidence, mortality, and at-risk populations. JPEN. Journal of Parenteral and Enteral Nutrition 26 (2002): S19-24.
- P-H, Wang K, Wang C-Y, et al. Risk of pneumonia in patients with gastroesophageal reflux disease: A population-based cohort study. PloS One 12 (2017): e0183808.
- Son Y G, Shin J, Ryu H G. Pneumonitis and pneumonia after aspiration. Journal of Dental Anesthesia and Pain Medicine 17 (2017): 1-12.
- Almirall J, Cabré M, Clavé P. Complications of oropharyngeal dysphagia: Aspiration pneumonia. Nestle Nutrition Institute Workshop Series 72 (2012): 67-76.
- Aspiration pneumonia. Respirology (Carlton, Vic.) 14 (2009): S59-S64.
- Lee H W, Min J, Park J, et al. Clinical impact of early bronchoscopy in mechanically ventilated patients with aspiration pneumonia. Respirology (Carlton, Vic.) 20 (2015): 1115-1122.
- Moore F A. Treatment of aspiration in intensive care unit patients. JPEN. Journal of Parenteral and Enteral Nutrition 26 (2002): S69-S74.