Newly Described Eosinophilic, Solid and Cystic Renal Cell Carcinoma: A Case Report and Review of the Literature
Article Information
Aaron Yunker, MD1*, Luke Holder, MD2, Joshua Nething, MD3
1Cleveland Clinic Akron General, Department of Urology, Akron, OH, USA
2SUMMA Akron City Hospital, Department of Pathology, Akron, OH, USA
3SUMMA Akron City Hospital, Department Urologic Oncology, Akron OH, USA
*Corresponding Author: Dr. Aaron Yunker, MD, Cleveland Clinic Akron General, Department of Urology, Akron, OH, USA
Received: 19 May 2020; Accepted: 16 June 2020; Published: 25 June 2020
Citation: Aaron Yunker, Luke Holder, Joshua Nething. Newly Described Eosinophilic, Solid and Cystic Renal Cell Carcinoma: A Case Report and Review of the Literature. Archives of Nephrology and Urology 3 (2020): 038-045.
Share at FacebookAbstract
Introduction: Renal cell carcinoma accounts for 2-3% of adult malignant neoplasms and has the worst prognosis of the common urologic malignancies. According to the 2016 WHO classification there are 16 distinct histologic subtypes for renal cell carcinoma. Recently, an eosinophilic, solid and cystic renal cell carcinoma histologic subtype has been described and proposed as a separate entity. There are only 60 cases reported in the literature, here we report the 61st case and review the literature.
Case Report: A 59-year-old woman presented in December 2018 with a renal mass found incidentally on a screening Computed Tomography. Magnetic Resonance Imaging of the Abdomen with and without contrast revealed an enhancing 2cm right lower pole renal mass. The patient elected to undergo laparoscopic with robotic assistance right retroperitoneal partial nephrectomy in March of 2019. Pathology was consistent with eosinophilic, solid and cystic renal cell carcinoma.
Discussion: ESC RCC is an emerging entity whose incidence will continue to rise as it is better recognized. To our knowledge, this is the 61st reported case. After reviewing the literature, we compiled a table comparing the available data for each of the 61 cases. We found that It predominantly affects females at a younger age than other forms of RCC. It appears to be more indolent than clear cell RCC with higher rates of organ-confined disease and lower rates of stage IV disease. There is limited data regarding imaging findings and only one article that looked at this specifically. There were only 3 cases of metastasis.
Keywords
Renal Cell Carcinoma (RCC); Eosinophilic; solid and cystic renal cell carcinoma (ESC RCC); Histologic subtype; Tuberous Sclerosis; Emerging entity; Kidney
Renal Cell Carcinoma (RCC) articles, Eosinophilic articles, solid and cystic renal cell carcinoma (ESC RCC) articles, Histologic subtype articles, Tuberous Sclerosis articles, Emerging entity articles, Kidney articles
Renal Cell Carcinoma articles Renal Cell Carcinoma Research articles Renal Cell Carcinoma review articles Renal Cell Carcinoma PubMed articles Renal Cell Carcinoma PubMed Central articles Renal Cell Carcinoma 2023 articles Renal Cell Carcinoma 2024 articles Renal Cell Carcinoma Scopus articles Renal Cell Carcinoma impact factor journals Renal Cell Carcinoma Scopus journals Renal Cell Carcinoma PubMed journals Renal Cell Carcinoma medical journals Renal Cell Carcinoma free journals Renal Cell Carcinoma best journals Renal Cell Carcinoma top journals Renal Cell Carcinoma free medical journals Renal Cell Carcinoma famous journals Renal Cell Carcinoma Google Scholar indexed journals Eosinophilic articles Eosinophilic Research articles Eosinophilic review articles Eosinophilic PubMed articles Eosinophilic PubMed Central articles Eosinophilic 2023 articles Eosinophilic 2024 articles Eosinophilic Scopus articles Eosinophilic impact factor journals Eosinophilic Scopus journals Eosinophilic PubMed journals Eosinophilic medical journals Eosinophilic free journals Eosinophilic best journals Eosinophilic top journals Eosinophilic free medical journals Eosinophilic famous journals Eosinophilic Google Scholar indexed journals solid and cystic renal cell carcinoma articles solid and cystic renal cell carcinoma Research articles solid and cystic renal cell carcinoma review articles solid and cystic renal cell carcinoma PubMed articles solid and cystic renal cell carcinoma PubMed Central articles solid and cystic renal cell carcinoma 2023 articles solid and cystic renal cell carcinoma 2024 articles solid and cystic renal cell carcinoma Scopus articles solid and cystic renal cell carcinoma impact factor journals solid and cystic renal cell carcinoma Scopus journals solid and cystic renal cell carcinoma PubMed journals solid and cystic renal cell carcinoma medical journals solid and cystic renal cell carcinoma free journals solid and cystic renal cell carcinoma best journals solid and cystic renal cell carcinoma top journals solid and cystic renal cell carcinoma free medical journals solid and cystic renal cell carcinoma famous journals solid and cystic renal cell carcinoma Google Scholar indexed journals Histologic subtype articles Histologic subtype Research articles Histologic subtype review articles Histologic subtype PubMed articles Histologic subtype PubMed Central articles Histologic subtype 2023 articles Histologic subtype 2024 articles Histologic subtype Scopus articles Histologic subtype impact factor journals Histologic subtype Scopus journals Histologic subtype PubMed journals Histologic subtype medical journals Histologic subtype free journals Histologic subtype best journals Histologic subtype top journals Histologic subtype free medical journals Histologic subtype famous journals Histologic subtype Google Scholar indexed journals Tuberous Sclerosis articles Tuberous Sclerosis Research articles Tuberous Sclerosis review articles Tuberous Sclerosis PubMed articles Tuberous Sclerosis PubMed Central articles Tuberous Sclerosis 2023 articles Tuberous Sclerosis 2024 articles Tuberous Sclerosis Scopus articles Tuberous Sclerosis impact factor journals Tuberous Sclerosis Scopus journals Tuberous Sclerosis PubMed journals Tuberous Sclerosis medical journals Tuberous Sclerosis free journals Tuberous Sclerosis best journals Tuberous Sclerosis top journals Tuberous Sclerosis free medical journals Tuberous Sclerosis famous journals Tuberous Sclerosis Google Scholar indexed journals Emerging entity articles Emerging entity Research articles Emerging entity review articles Emerging entity PubMed articles Emerging entity PubMed Central articles Emerging entity 2023 articles Emerging entity 2024 articles Emerging entity Scopus articles Emerging entity impact factor journals Emerging entity Scopus journals Emerging entity PubMed journals Emerging entity medical journals Emerging entity free journals Emerging entity best journals Emerging entity top journals Emerging entity free medical journals Emerging entity famous journals Emerging entity Google Scholar indexed journals Kidney articles Kidney Research articles Kidney review articles Kidney PubMed articles Kidney PubMed Central articles Kidney 2023 articles Kidney 2024 articles Kidney Scopus articles Kidney impact factor journals Kidney Scopus journals Kidney PubMed journals Kidney medical journals Kidney free journals Kidney best journals Kidney top journals Kidney free medical journals Kidney famous journals Kidney Google Scholar indexed journals metastasis articles metastasis Research articles metastasis review articles metastasis PubMed articles metastasis PubMed Central articles metastasis 2023 articles metastasis 2024 articles metastasis Scopus articles metastasis impact factor journals metastasis Scopus journals metastasis PubMed journals metastasis medical journals metastasis free journals metastasis best journals metastasis top journals metastasis free medical journals metastasis famous journals metastasis Google Scholar indexed journals Positron Emission Tomography articles Positron Emission Tomography Research articles Positron Emission Tomography review articles Positron Emission Tomography PubMed articles Positron Emission Tomography PubMed Central articles Positron Emission Tomography 2023 articles Positron Emission Tomography 2024 articles Positron Emission Tomography Scopus articles Positron Emission Tomography impact factor journals Positron Emission Tomography Scopus journals Positron Emission Tomography PubMed journals Positron Emission Tomography medical journals Positron Emission Tomography free journals Positron Emission Tomography best journals Positron Emission Tomography top journals Positron Emission Tomography free medical journals Positron Emission Tomography famous journals Positron Emission Tomography Google Scholar indexed journals Computed Tomography articles Computed Tomography Research articles Computed Tomography review articles Computed Tomography PubMed articles Computed Tomography PubMed Central articles Computed Tomography 2023 articles Computed Tomography 2024 articles Computed Tomography Scopus articles Computed Tomography impact factor journals Computed Tomography Scopus journals Computed Tomography PubMed journals Computed Tomography medical journals Computed Tomography free journals Computed Tomography best journals Computed Tomography top journals Computed Tomography free medical journals Computed Tomography famous journals Computed Tomography Google Scholar indexed journals
Article Details
1. Introduction
Renal cell carcinoma (RCC) has an incidence of 65,000 new cases a year in the United States accounting for 2-3% of adult malignant neoplasms. It also has the worst prognosis of the common urologic malignancies [1]. According to the 2016 World Health Organization classification, there are 16 distinct histologic subtypes for renal cell carcinoma with clear cell, papillary, and chromophobe being the most common types respectively [2]. This classification is important for both prognosis and for therapeutic recommendations. Recently, an eosinophilic, solid and cystic renal cell carcinoma (ESC RCC) histologic subtype has been described and proposed as a separate entity [3-5]. As of this paper, only 60 cases have been described in the literature [6]. Here we describe the 61st case of this newly described variant and review the literature.
2. Case Report
A 59-year-old woman underwent a Positron Emission Tomography (PET)/Computed Tomography (CT) in December 2018 as a part of a work up for a lung nodule. The PET scan was negative except for an incidental renal mass that was moderately FDG avid. The patient underwent subsequent Magnetic Resonance Imaging of the Abdomen with and without contrast revealing an enhancing 2 cm right lower pole renal mass. The patient denied urologic complaints or gross hematuria. The patient was a former smoker with a 20-pack year history. No history of tuberous sclerosis. The patient elected to undergo a retroperitoneal robotic right partial nephrectomy in March of 2019. Pathology revealed an oncocytic lesion with macro and microcystic change as well as some hobnail like areas. Immunohistochemical stains performed at our institution revealed the tumor being negative for CK7, CD117, S100, and Ki67. Immunohistochemical stains performed at a second institution demonstrated staining with SDHB, positive staining CK20 and focal CK7 staining consistent with eosinophilic, solid and cystic renal cell carcinoma. The patient did well post-operatively. Retroperitoneal ultrasound three months post-operatively showed normal post-operative change. Her pulmonary nodule did not meet criteria for malignancy on PET CT and was stable on follow up CT chest in March of 2019. The patient’s final pathologic stage was pT1a.
3. Discussion
Though ESC RCC was first described by Schreiner and colleagues in 2010, it is not new, just newly recognized. The literature has subsequently expanded to include 61 patients including the patient presented in this study. This number will continue to rise as many of these cases came from reviewing previously unclassified cases of RCC. Because of this, the current incidence is unknown but has been estimated to be ~ 0.2% [6]. Sections of the mass show a partially encapsulated lesion made up of solid areas admixed with cystic spaces with both areas composed of oncocytic cells. The tumor shows multiple areas where it invades through the capsule (Figure 1). The cells are arranged in an acinar pattern within the solid component and the cells lining the cysts show a hobnail appearance (Figure 2). The malignant cells in both the solid and cystic components show a similar morphology (besides the hobnail appearance within the cyst lining): malignant appearing nuclei with atypical nuclear membranes, prominent nucleoli, fine chromatin, and granular eosinophilic cytoplasm with a portion of the cells showing a defined cytoplasmic outline (Figure 3). On H&E, the tumor shows a low mitotic count.
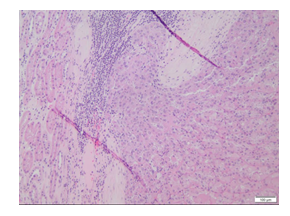
Figure 1: Capsular invasion.
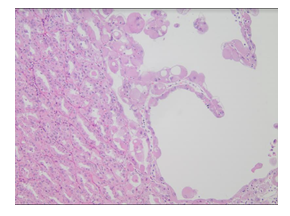
Figure 2: Higher power showing the hobnail appearance of the cyst lining next to solid areas.
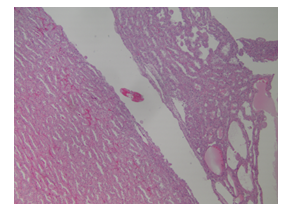
Figure 3: Low power showing solid and cystic appearance
Most of the cases so far have been reported in pathology literature but the clinical utility in recognizing this histologic variant as a separate entity lies in predicting its clinical course and by changing practice recommendations. We attempted to view the data so far from the lens of a urology clinician and its application in the clinical setting. In order to do so, we compiled a table of the best available data for the 61 reported cases in the literature (Table 1). To our knowledge, this is the most comprehensive review of the literature to date, and the only one attempting to compile data for all 61 patients.
Table 1: Best available data for all 61 reported cases of ESC RCC.
We found the median age at diagnosis to be 48.5 years with a range of 14-85 years. This is younger than the median age at diagnosis of all RCC of 64 years old [7]. ESC RCC preferentially affects females with 87% (48 vs 7) occurring in females compared to males. Though, initially reported in patients with tuberous sclerosis, the majority occur in non-TSC patients (79%, 31 vs 8). The laterality of the lesion was split evenly between left and right kidney.
An important area to consider is how ESC RCC presents radiographically and if there are certain findings on imaging that may alert a clinician that a tumor might be ESC RCC prior to having specimen for pathologic review. Unfortunately, data on imaging of ESC RCC is extremely limited in the literature. Fenelon et al published the only article to date focusing specifically on imaging findings of ESC RCC [8]. They described the imaging features of two patients at their institution. The first was a 49-year-old female with an incidental 4cm well defined nodule with small cystic areas in the medullary aspect of the upper pole of the right kidney. The second was a 30-year-old female with an incidental 3 cm cystic renal lesion with thickened irregular walls and septa (Bosniak III). Our patient had a 20 × 19 × 19 mm enhancing right lower pole renal mass with a few small internal cystic foci that demonstrated diffusion restriction and washout characteristics during delayed phases of contrast enhancement on MRI (Figure 4). All three of these patients had a cystic component to their mass. Much more data will need to be compiled in order to make any kind of inferences or predict ESC RCC based on imaging alone. We encourage future case reports to include more detailed descriptions of the masses on imaging.
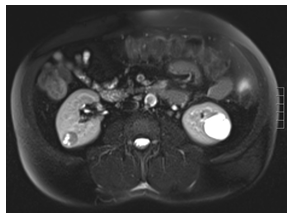
Figure 4: 20 × 19 × 19 mm enhancing right lower pole renal mass with a few small internal cystic foci that demonstrate diffusion restriction and washout characteristics during delayed phases of contrast enhancement.
The pathologic stage and prognosis are particularly important in order to help guide clinical practice. ESC RCC has previously been suggested to have a more indolent course than clear cell RCC [6]. The data collected so far certainly agrees with that. The vast majority of tumors were small and organ-confined with 80% being stage pT1 (32 of 55 (58%) pT1a and 12 (22%) pT1b). Over 90% (50 of 55) patients had organ confined disease defined as stage I or II. This is considerably higher than the roughly two-thirds organ-confined disease for all RCC [7]. The median size was 41.5 mm with a broad range of 5-150 mm.
Not all ESC RCC have followed this indolent course; there have been reports of ESC RCC with locally advanced disease and metastasis. There have been 3 reported cases of metastasis and 2 cases of locally advanced disease.
The first case was a 15-year-old female that presented with a multifocal 9 cm and 4 cm renal masses with inferior vena cava involvement and pulmonary emboli. She developed liver metastasis 2 years later and was treated with salvage chemotherapy. We are unsure what agent was used. She was noted to be alive with disease at 72 months of follow up [9]. The second case was a 69-year-old female with a 15 cm renal mass and 1 of 3 hilar lymph nodes found to have metastasis with ESC RCC [10]. The third case was 50-year-old female that underwent a radical nephrectomy for a pT1a renal mass followed by sunitinib and palliative radiation to a discovered left pubic bone and iliac crest metastasis. Patient was considering immunotherapy with nivolumab as well as hospice at last follow up.
There were 2 cases representing advanced pathology. The first of these was a 50-year-old male with a 20.5 cm tumor and extension into the adrenal gland and left retroperitoneum. The second was a patient with pT3a disease. With 3 cases of metastasis to date, that accounts for less than 5% of reported cases. This is again below the reported rate of stage IV RCC based on the national cancer database which ranged from 13.5-14.6% from 2007-2016 [11]. Follow up data was available for 34 patients. 29 showed no evidence of disease, 4 died of other causes, and 1 patient was alive with disease.
4. Conclusion
ESC RCC is an emerging entity whose incidence will continue to rise as it is better recognized. It predominantly affects females at a younger age than other forms of RCC. It appears to be more indolent than clear cell RCC with higher rates of organ-confined disease and lower rates of stage IV disease. With only 61 cases in the literature to date, much more data is needed to confirm these conclusions, but the table we constructed should build the foundation for future research.
References
- Hon, W. Scott McDougal, et al. Campbell-Walsh Urology 11th Edition Review. Elsevier Health Sciences (2015): 1320.
- Moch H, Cubilla AL, Humphrey PA, et al. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs-Part A: Renal, Penile, and Testicular Tumours. Eur Urol 70 (2016): 93-105.
- Guo J, Tretiakova MS, Troxell ML, et al. Tuberous sclerosis-associated renal cell carcinoma: a clinicopathologic study of 57 separate carcinomas in 18 patients. Am. J. Surg. Pathol 38 (2014): 1457-1467.
- Trpkov K, Hes O, Bonert M, et al. Eosinophilic, solid, and cystic renal cell carcinoma: clinicopathologic study of 16 unique, sporadic neoplasms occurring in women. Am. J. Surg. Pathol 40 (2016): 60-71.
- Trpkov K, Abou-Ouf H, Hes O, et al. Eosinophilic solid and cystic renal cell carcinoma (ESC RCC): further morphologic and molecular characterization of ESC RCC as a distinct entity. Am. J. Surg. Pathol 41 (2017): 1299- 1308.
- Trpkov K, Hes O. New and emerging renal entities: a perspective post-WHO 2016 classification. Histopathology 74 (2019): 31-59.
- Kidney Cancer: Statistics|Cancer.Net. Cancer. https://www.cancer.net/cancer-types/kidney-cancer/statistics (2012).
- Fenelon SS, Santos J, Faraj SF, et al. Eosinophilic solid and cystic renal cell carcinoma: imaging features of a novel neoplasm. Urology 114 (2018): e9-e10.
- Li Y, Reuter VE, Matoso A, et al. Re-evaluation of 33 ‘unclassified’ eosinophilic renal cell carcinomas in young patients. Histopathology 72 (2018): 588-600.
- McKenney JK, Przybycin C, Trpkov K, et al. Eosinophilic solid and cystic (ESC) renal cell carcinomas have metastatic potential. Histopathology 72 (2018): 1066-1067.
- American College of Surgeons. National Cancer Database, https://www.facs.org/-/media/files/quality-programs/cancer/ncdb/cancer-cases-reported-to-the-ncdb-by-tumor-type-and-ajcc-stage.ashx. (2019).
- Schreiner A, Daneshmand S, Bayne A, et al. Distinctive morphology of renal cell carcinomas in tuberous sclerosis. Int J Surg Pathol 18 (2010): 409-418.
- Parilla M, Kadri S, Patil SA, et al. Are sporadic eosinophilic solid and cystic renal cell carcinomas characterized by somatic tuberous sclerosis gene mutations? Am. J. Surg. Pathol 42 (2018): 911-917.
- Tretiakova MS. Eosinophilic solid and cystic renal cell carcinoma mimicking epithelioid angiomyolipoma: series of 4 primary tumors and 2 metastases. Hum. Pathol pii (2018): S0046-8177/li>
- Mehra R, Vats P, Cao X, et al. Somatic bi-allelic loss of tsc genes in eosinophilic solid and cystic renal cell carcinoma. Eur. Urol pii (2018): S0302
- Cho WC, Collins K, Mnayer L, et al. Concurrent Eosinophilic Solid and Cystic Renal Cell Carcinoma and Angiomyolipoma With Epithelial Cysts in the Setting of Tuberous Sclerosis Complex: A Rare Synchronous Occurrence of 2 Distinct Entities. Int J Surg Pathol 27 (2019): 804-811.
