Mode of Delivery Among Women with a History of Prior Cesarean Birth at Mizan-Tepi University Teaching Hospital
Article Information
Margo S Harrison1*, Tewodros Liyew2, Ephrem Kirub2, Biruk Teshome2, Andrea Jimenez-Zambrano1, Margaret Muldrow3, Teklemariam Yarinbab2
1University of Colorado School of Medicine, Colorado, USA
2Mizan-Tepi University Teaching Hospital, Aman, Bench Maji Zone, Ethiopia
3Village Health Partnership, Colorado, USA
*Corresponding author: Margo S Harrison, University of Colorado School of Medicine, Mail Stop B198-2, Academic Office 1, 12631 E. 17th Avenue, Rm 4211, Aurora, Colorado 80045, USA
Received: 28 December 2020; Accepted: 06 January 2021; Published: 08 January 2021
Citation:
Margo S Harrison, Tewodros Liyew, Ephrem Kirub, Biruk Teshome, Andrea Jimenez-Zambrano, Margaret Muldrow, Teklemariam Yarinbab. Mode of Delivery Among Women with a History of Prior Cesarean Birth at Mizan-Tepi University Teaching Hospital. Journal of Women’s Health and Development 4 (2021): 001-009.
Share at FacebookAbstract
Objectives: The objective of this study was to observe mode of delivery among women with a history of prior cesarean birth.
Methods: After collecting data on a convenience sample of 1,000 women giving birth at 28 weeks gestation or greater at Mizan-Tepi University Teaching Hospital, we reduced the sample to only include women with a history of prior cesarean birth. We wanted to observe mode of delivery among this cohort and determine if any characteristics were associated with elective repeat cesarean birth, as compared to vaginal birth after cesarean.
Results: Of 1,000 women in our convenience sample, data on history of prior cesarean birth was missing on 2 women (0.2%). Of the remaining women, 49 (4.9%) reported a history of prior cesarean; 44 (89.8%) reported one prior cesarean and 5 (10.2%) women had two prior cesarean births. Repeat cesarean birth occurred in 65.1% (n = 29/44) of women with one prior cesarean and in 80.0% (n = 4/5) of women with two prior surgeries. Among the total cohort of women with a history of prior cesarean birth, of those who experienced repeat cesarean birth (n = 33), 27.3% (n = 9) occurred pre-labor, 69.7% (n = 23) occurred intrapartum after the onset of spontaneous labor, and 3.0% (n = 1) occurred intrapartum during the course of an induced or augmented labor. Labor onset and cervical exam on admission were statistically significantly different in bivariate comparisons of women who successfully achieved vaginal birth after cesarean as compared to those who gave birth by repeat cesarean birth, and postpartum maternal antibiotics were more common after repeat cesarean birth, p < 0.05. In a multivariable model of factors associated with successful vaginal birth after cesarean, the likelihood of successful vaginal birth was increased 15% for each increasing centimeter of dilation on a woman’s admission cervical exam (RR 1.15, p = 0.004).
C
Keywords
History of Cesarean Birth, Ethiopia
History of Cesarean Birth articles History of Cesarean Birth Research articles History of Cesarean Birth review articles History of Cesarean Birth PubMed articles History of Cesarean Birth PubMed Central articles History of Cesarean Birth 2023 articles History of Cesarean Birth 2024 articles History of Cesarean Birth Scopus articles History of Cesarean Birth impact factor journals History of Cesarean Birth Scopus journals History of Cesarean Birth PubMed journals History of Cesarean Birth medical journals History of Cesarean Birth free journals History of Cesarean Birth best journals History of Cesarean Birth top journals History of Cesarean Birth free medical journals History of Cesarean Birth famous journals History of Cesarean Birth Google Scholar indexed journals surgeries articles surgeries Research articles surgeries review articles surgeries PubMed articles surgeries PubMed Central articles surgeries 2023 articles surgeries 2024 articles surgeries Scopus articles surgeries impact factor journals surgeries Scopus journals surgeries PubMed journals surgeries medical journals surgeries free journals surgeries best journals surgeries top journals surgeries free medical journals surgeries famous journals surgeries Google Scholar indexed journals vaginal birth articles vaginal birth Research articles vaginal birth review articles vaginal birth PubMed articles vaginal birth PubMed Central articles vaginal birth 2023 articles vaginal birth 2024 articles vaginal birth Scopus articles vaginal birth impact factor journals vaginal birth Scopus journals vaginal birth PubMed journals vaginal birth medical journals vaginal birth free journals vaginal birth best journals vaginal birth top journals vaginal birth free medical journals vaginal birth famous journals vaginal birth Google Scholar indexed journals interpregnancy articles interpregnancy Research articles interpregnancy review articles interpregnancy PubMed articles interpregnancy PubMed Central articles interpregnancy 2023 articles interpregnancy 2024 articles interpregnancy Scopus articles interpregnancy impact factor journals interpregnancy Scopus journals interpregnancy PubMed journals interpregnancy medical journals interpregnancy free journals interpregnancy best journals interpregnancy top journals interpregnancy free medical journals interpregnancy famous journals interpregnancy Google Scholar indexed journals cervical articles cervical Research articles cervical review articles cervical PubMed articles cervical PubMed Central articles cervical 2023 articles cervical 2024 articles cervical Scopus articles cervical impact factor journals cervical Scopus journals cervical PubMed journals cervical medical journals cervical free journals cervical best journals cervical top journals cervical free medical journals cervical famous journals cervical Google Scholar indexed journals antibiotic articles antibiotic Research articles antibiotic review articles antibiotic PubMed articles antibiotic PubMed Central articles antibiotic 2023 articles antibiotic 2024 articles antibiotic Scopus articles antibiotic impact factor journals antibiotic Scopus journals antibiotic PubMed journals antibiotic medical journals antibiotic free journals antibiotic best journals antibiotic top journals antibiotic free medical journals antibiotic famous journals antibiotic Google Scholar indexed journals Medicine articles Medicine Research articles Medicine review articles Medicine PubMed articles Medicine PubMed Central articles Medicine 2023 articles Medicine 2024 articles Medicine Scopus articles Medicine impact factor journals Medicine Scopus journals Medicine PubMed journals Medicine medical journals Medicine free journals Medicine best journals Medicine top journals Medicine free medical journals Medicine famous journals Medicine Google Scholar indexed journals augmented labor articles augmented labor Research articles augmented labor review articles augmented labor PubMed articles augmented labor PubMed Central articles augmented labor 2023 articles augmented labor 2024 articles augmented labor Scopus articles augmented labor impact factor journals augmented labor Scopus journals augmented labor PubMed journals augmented labor medical journals augmented labor free journals augmented labor best journals augmented labor top journals augmented labor free medical journals augmented labor famous journals augmented labor Google Scholar indexed journals cervical exam articles cervical exam Research articles cervical exam review articles cervical exam PubMed articles cervical exam PubMed Central articles cervical exam 2023 articles cervical exam 2024 articles cervical exam Scopus articles cervical exam impact factor journals cervical exam Scopus journals cervical exam PubMed journals cervical exam medical journals cervical exam free journals cervical exam best journals cervical exam top journals cervical exam free medical journals cervical exam famous journals cervical exam Google Scholar indexed journals births rates articles births rates Research articles births rates review articles births rates PubMed articles births rates PubMed Central articles births rates 2023 articles births rates 2024 articles births rates Scopus articles births rates impact factor journals births rates Scopus journals births rates PubMed journals births rates medical journals births rates free journals births rates best journals births rates top journals births rates free medical journals births rates famous journals births rates Google Scholar indexed journals
Article Details
1. Introduction
Cesarean birth rates are increasing, globally [1]. As cesarean births rates increase, so does the global prevalence of women with a history of prior cesarean birth. There is equipoise between whether trial of labor after cesarean versus elective repeat cesarean birth should be recommended among this population as each mode of delivery is associated with a balance of risks and benefits for the mother, as well as for the fetus [2]. It is increasingly common to focus on informed decision making with women regarding their delivery options [2]. Decision aids and predictive models have been devised to assist with this process [3-5]. Little data on these practices in low- and middle-income countries are available. In order to determine the need for assistance with decision-making in low-resource settings, it is imperative to first understand what mode of delivery women with a history of prior cesarean birth are experiencing. We know from prior research that rates of vaginal birth after cesarean in sub-Saharan Africa are around 80.0%; thus, we hypothesized that among our convenience sample of women giving birth at a teaching and referral facility in the Southern Nations, Nationalities, and People’s Region of Ethiopia, we would expect to observe similar rates [6]. We wanted to determine if any characteristics were associated with mode of delivery (repeat cesarean birth versus vaginal birth after cesarean), and if any outcomes were more likely after one mode compared to the other.
2. Methodology
We conducted a hospital-based, prospective, cross-sectional quality improvement analysis at Mizan-Tepi University Teaching Hospital (MTUTH), in the Southern Nations, Nationalities, and People’s Region of Ethiopia. We observed a convenience sample of 1,000 women who gave birth (after 28 completed weeks of gestation) on labor and delivery at MTUTH between May 6 and October 21, 2019. Through a combination of chart review and structured interview at admission, delivery, and discharge, three physicians collected de-identified data, which was entered into REDCap [7]. Bivariate comparisons of sociodemographic, obstetric, birth, and pregnancy outcomes of women experiencing vaginal versus cesarean birth were performed using STATA software version 15.2 (StataCorp LP, College Station, TX, USA). Fisher’s exact, Chi-squared, and Kruskal-Wallis tests were performed depending on the variables. All covariates significant to p < 0.05 were included in a multivariable Poisson model with robust error variance (because vaginal birth after cesarean birth was prevalent) to determine which covariates were independently associated with cesarean birth. Despite the quality improvement nature of the work and the fact that only de-identified data was collected, oral consent was obtained from each woman before any of her data was recorded. This quality improvement survey was given an exempt from human subjects’ research approval (COMIRB # 18-2738) by the University of Colorado and approval.
3. Results
Figure 1 illustrates our study cohort. Of 1,000 women in our convenience sample, data on history of prior cesarean birth was missing on 2 women (0.2%). Of the remaining women, 49 (4.9%) reported a history of prior cesarean; 44 (89.8%) reported one prior cesarean and 5 (10.2%) women had two prior cesarean births. Table 1 shows mode of delivery (spontaneous vaginal birth, forceps-assisted or vacuum-assisted vaginal birth, and repeat cesarean birth) of the cohort of women with a history of prior cesarean birth. Repeat cesarean birth occurred in 65.1% (n = 29/44) of women with one prior cesarean and in 80.0% (n = 4/5) of women with two prior surgeries. Two of the women (4.6%) who achieved successful vaginal birth after a history of one prior cesarean did so with vacuum assistance, while there were no assisted vaginal births among women with a history of two prior cesareans. Table 2 illustrates when in the labor course birth occurred for women who delivered by repeat cesarean. Among the total cohort of women with a history of prior cesarean birth, of those who experienced repeat cesarean birth (n = 33), 27.3% (n = 9) occurred pre-labor, 69.7% (n = 23) occurred intrapartum after the onset of spontaneous labor, and 3.0% (n = 1) occurred intrapartum during the course of an induced or augmented labor. The table also shows the reported general indications for cesareans at the study site, which by order of prevalence were maternal (66.7%), fetal (24.2%), maternal and fetal (6.1%), and failed trial of labor (3.0%).
Table 3 compares women who experienced vaginal birth after cesarean to those who underwent repeat cesarean birth. Overall the women had a median age of 25 years (interquartile range [IQR] 22,29), 44.9% of them had a primary school education, 42.9% were Protestant, 100.0% were not single, 55.1% lived in an urban area, and the women experienced a median number of 4 prenatal visits (IQR 4,5). Almost two-thirds of the population was nulliparous, the median interpregnancy interval was 48 months (IQR 1.5,3], most were in labor less than twenty-four hours (78.5%), and antepartum hemorrhage and blood pressure elevations were prevalent in 5.4% and 6.1% of the cohort, respectively. The median gestational length was 39 weeks (IQR 38,42), only 2.0% of neonates weighed less than 2500 grams, and the sex imbalance was quite pronounced—males accounted for two-thirds of the population.
In bivariate comparisons, shown in columns 2 – 4 of Table 3, only onset of labor and cervical dilation on admission to the facility were found to be statistically significantly different between women experiencing repeat cesarean birth as compared to those experiencing vaginal birth after cesarean. All women (100.0%) who achieved vaginal birth after cesarean went into labor spontaneously, compared to 69.7% of those who underwent repeat cesarean birth. Women who delivered vaginally were admitted with a higher cervical dilation on admission (3 versus 2 centimeters) compared to those who were delivered by repeat cesarean. It was also notable that maternal postpartum antibiotic administration was higher in women who experienced repeat cesarean. The final rows of Table 3 shown multivariable modeling of characteristics associated with successful vaginal birth after cesarean. The only characteristic that was associated with a higher likelihood of vaginal birth was greater dilation on admission; each centimeter of increased dilation was associated with a 15% increase risk (chance) of vaginal birth (RR 1.15, p = 0.004).
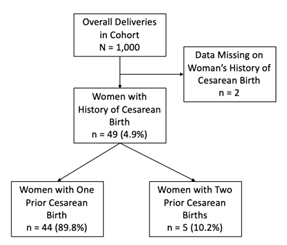
Figure 1: Population of women with history of prior cesarean birth at Mizan-Tepi University Teaching Hospital.
|
Method of Delivery |
Women with One Prior Cesarean (n = 44, 89.8%) |
Women with Two Prior Cesareans (n = 5, 10.2%) |
|
Spontaneous Vaginal Birth |
13 (29.5%) |
1 (20.0%) |
|
Forceps-Assisted Vaginal Birth |
0 (0.0%) |
0 (0.0%) |
|
Vacuum-Assisted Vaginal Birth |
2 (4.6%) |
0 (0.0%) |
|
Repeat Cesarean Birth |
29 (65.1%) |
4 (80.0%) |
Table 1: Mode of delivery among women with a history of prior cesarean birth, by number of prior cesareans.
|
Onset of Labor |
Women Delivered by Repeat Cesarean Birth (n = 33, 67.3%) |
|
Pre-Labor |
9 (27.3%) |
|
Intrapartum, after Spontaneous Labor Onset |
23 (69.7%) |
|
Intrapartum, after Induction/Augmentation of Labor |
1 (3.0%) |
|
Indication for Cesarean for Women Delivered by Repeat Cesarean Birth (n = 33) |
|
|
Maternal Indication, Only |
22 (66.7%) |
|
Maternal & Fetal Indication |
2 (6.1%) |
|
Fetal Indication, Only |
8 (24.2%) |
|
Failed Labor |
1 (3.0%) |
Table 2: Onset of labor and indication for cesarean birth among women delivered by repeat cesarean birth.
|
Characteristic |
Total N = 49 |
Vaginal Birth After Ce-sarean (n = 16, 32.7%) |
Repeat Cesarean Bi-rth (n = 33, 67.4%) |
P-Value |
|||
|
Sociodemographic |
|||||||
|
Age in years, Median (IQR) Missing |
25 [22, 29] 0 (0.0%) |
21 [24.5, 29] 0 (0.0%) |
27 [23, 29] 0 (0.0%) |
0.54a |
|||
|
Education Unable to read & write Read & write only Primary school Secondary school Higher education Missing |
7 (14.3%) 4 (8.2%) 22 (44.9%) 5 (10.2%) 11 (22.5%) 0 (0.0%) |
1 (6.3%) 3 (18.7%) 7 (43.7%) 0 (0.0%) 5 (31.3%) 0 (0.0%) |
6 (18.2%) 1 (3.0%) 15 (45.5%) 5 (15.2%) 6 (18.2%) 0 (0.0%) |
0.12b |
|||
|
Religion Muslim Orthodox Christian Catholic Christian Protestant Jehovah’s Witness Missing |
8 (16.3%) 19 (38.8%) 0 (0.0%) 21 (42.9%) 1 (2.0%) 0 (0.0%) |
1 (6.3%) 5 (31.2%) 0 (0.0%) 9 (56.2%) 1 (6.3%) 0 (0.0%) |
7 (21.2%) 14 (42.4%) 0 (0.0%) 12 (36.4%) 0 (0.0%) 0 (0.0%) |
0.17b |
|||
|
Relationship Status Single Not single Missing |
0 (0.0%) 49 (100.0%) 0 (0.0%) |
0 (0.0%) 16 (100.0%) 0 (0.0%) |
0 (0.0%) 33 (100.0%) 0 (0.0%) |
- |
|||
|
Woreda Urban Rural Missing |
27 (55.1%) 22 (44.9%) 0 (0.0%) |
10 (62.5%) 6 (37.5%) 0 (0.0%) |
17 (51.5%) 16 (48.5%) 0 (0.0%) |
0.47c |
|||
|
Number of Prenatal Visits Median (IQR) Missing |
4 [4, 5] 0 (0.0%) |
4 [3.5, 5.5] 0 (0.0%) |
4 [4, 5] 0 (0.0%) |
0.83a |
|||
|
Antepartum, Labor, and Delivery |
|||||||
|
Parity One Two Three+ Missing |
31 (63.3%) 12 (24.5%) 6 (12.2%) 0 (0.0%) |
8 (50.0%) 6 (37.5%) 2 (12.5%) 0 (0.0%) |
23 (69.7%) 6 (18.2%) 4 (12.1%) 0 (0.0%) |
0.29b |
|||
|
Number of Prior Cesarean Births One Two Missing |
44 (89.8%) 5 (10.2%) 0 (0.0%) |
15 (98.7%) 1 (6.3%) 0 (0.0%) |
29 (87.9%) 4 (12.1%) 0 (0.0%) |
1.0b |
|||
|
Interpregnancy Interval, Months (IQR) Missing |
48 [36, 60] 0 (0.0%) |
48 [42, 54] 0 (0.0%) |
48 [36,72] 0 (0.0%) |
1.0b |
|||
|
Labor Onset Not Applicable Spontaneous Induced/Augmented Missing |
9 (18.4%) 39 (79.6%) 1 (2.0%) 0 (0.0%) |
0 (0.0%) 16 (100.0%) 0 (0.0%) 0 (0.0%) |
9 (27.8%) 23 (69.7%) 1 (3.0%) 0 (0.0%) |
0.03b |
|||
|
Cervical Exam on Admission Median (IQR) Missing |
3 [1.5, 3] 0 (0.0%) |
3 [2.5, 7] 0 (0.0%) |
2 [0.5,3] 0 (0.0%) |
0.009a |
|||
|
Duration of Labor Not Applicable < 12 hours 12 – 24 hours 24+ hours Missing |
5 (8.9%) 26 (46.4%) 18 (32.1%) 7 (12.5%) 0 (0.0%) |
0 (0.0%) 18 (51.4%) 14 (40.0%) 3 (8.6%) 0 (0.0%) |
5 (23.8%) 8 (38.1%) 4 (19.1%) 4 (19.1%) 0 (0.0%) |
0.12b |
|||
|
Antepartum Hemorrhage No Yes Missing |
53 (94.6%) 3 (5.4%) 0 (0.0%) |
34 (97.1%) 1 (2.9%) 0 (0.0%) |
19 (90.5%) 2 (9.5%) 0 (0.0%) |
0.55b |
|||
|
Antepartum Pre-eclampsia/Eclampsia/Chronic Hypertension No Yes Missing |
46 (93.9%) 3 (6.1%) 0 (0.0%) |
16 (100.0%) 0 (0.0%) 0 (0.0%) |
30 (90.9%) 3 (9.1%) 0 (0.0%) |
0.54b |
|||
|
Gestational Age in Weeks, Median (IQR) Missing |
39 [38, 42] 0 (0.0%) |
40 [38.5, 41] 0 (0.0%) |
39 [38, 42] 0 (0.0%) |
0.74a |
|||
|
Birthweight (grams) <2500 2500 Missing |
1 (2.0%) 48 (98.0%) 0 (0.0%) |
1 (6.3%) 15 (93.7%) 0 (0.0%) |
0 (0.0%) 33 (100.0%) 0 (0.0%) |
0.33b |
|||
|
Baby Sex Male Female Missing |
32 (66.6%) 16 (33.3%) 0 (0.0%) |
9 (56.3%) 7 (43.7%) 0 (0.0%) |
23 (71.9%) 9 (28.1%) 0 (0.0%) |
0.28c |
|||
|
Postpartum Complications |
|||||||
|
Maternal |
|||||||
|
Postpartum Antibiotics No Yes Missing |
39 (79.6%) 10 (20.4%) 0 (0.0%) |
16 (100.0%) 0 (0.0%) 0 (0.0%) |
23 (69.7%) 10 (30.3%) 0 (0.0%) |
0.02b |
|||
|
Neonatal |
|||||||
|
Five-Minute Apgar Score Median (IQR) Missing |
8 [8, 9] 0 (0.0%) |
8 [8, 9] 0 (0.0%) |
9 [8, 9] 0 (0.0%) |
0.49a |
|||
|
Multivariable Model of Characteristics Associated with Vaginal Birth After Cesareand |
|||||||
|
Characteristic |
RR |
CI |
P-Value |
||||
|
Onset of Labor Centimeters of Cervical Dilation on Admission |
1.7 1.15 |
0.5,5.2 1.1,1.3 |
0.37 0.004 |
||||
a: Kruskal-Wallis test
b: Fisher’s Exact test
c: Chi-squared test
d: Multivariable Poisson Model with Robust Error Variance of Characteristics Associated with Cesarean Birth
Table 3: Bivariate comparisons of patient characteristics and outcomes between women undergoing repeat cesarean birth as compared to vaginal birth after cesarean, and multivariable model of factors associated with vaginal birth after cesarean.
4. Discussion
Our analysis showed that almost one-third of women with a history of prior cesarean birth are attempting a trial of labor after cesarean at MTUTH, including women requiring induction or augmentation. We have conducted a number of other analyses with this dataset on characteristics associated with cesarean birth among subgroups of women and have found that generally, there are clear obstetric complications associated with cesarean birth, such as prolonged labor. In this analysis, however, the characteristic associated with cesarean birth was how dilated (Bishop’s score) the woman was on admission—the more dilated she was, the lower her risk of cesarean birth. Reported indications were maternal, fetal, or a combination of the two, with one woman identified as undergoing repeat cesarean birth for failed trial of labor.
According to our analysis, there was no difference in the prevalence of intrapartum or postpartum complications between the study groups. We did test a number of antepartum, intrapartum, and postpartum maternal and neonatal complications, but there was no difference in outcomes between the groups (data not shown). Prior research has found that pre-labor elective research cesarean birth is associated with reduced postpartum hemorrhage and improved neonatal outcomes as compared to vaginal birth after cesarean [8]. Though the data are not shown, we did compare all pre-labor to intrapartum cesarean births (leaving out vaginal births after cesarean) and found no bivariate differences in antepartum, intrapartum, or postpartum characteristics or outcomes, either (data not shown). This suggests, along with the fact that 100.0% of women achieving vaginal birth after cesarean were in labor spontaneously, that women and/or providers may be selecting women for mode of delivery, appropriately. Those that are admitted in labor with a favorable exam may be allowed to labor, as compared to those who are not dilated and showing no signs of labor.
When we discussed these findings with coauthors and colleagues at MTUTH, the way these women are currently managed is that providers currently screen for any contraindications to vaginal birth after cesarean using a protocol based on national recommendations. If, according to the protocol, the woman qualifies for a safe trial of labor, she will then be offered the option of cesarean birth versus trial of labor after cesarean. She is usually counseled by a physician during her antenatal care in the outpatient setting and given time to consider the choice. No specific protocol is currently used for counseling. If she chooses to labor, she is monitored with electronic fetal monitoring or managed one-on-one by a midwife on service. MTUTH also has a blood bank on site. The current practices at MTUTH appear to be resulting in the safe management of trial of labor after cesarean. An area of research might be into the standardization of the vaginal birth after cesarean counseling women are receiving or use of a decision aid to ensure that all women are receiving similar information under similar circumstances. The one-to-one attention during trial of labor would also be an area of potential research. This analysis is limited by the lack of contextual data surrounding counseling of women and the method women use to decide on mode of delivery after a prior cesarean birth. Further qualitative research on this topic would add richness to the data and assist with disseminating the success that MTUTH has achieved regarding safe trial of labor after cesarean and vaginal birth after cesarean. Prospective research on the process used by MTUTH regarding mode of delivery decision-making and intrapartum management would enable further research on best methods to implement and disseminate these evidence-based practices, elsewhere.
Conflict of Interest
The authors have no relationships to disclose that may be deemed to influence the objectivity of this paper and its review. The authors report no commercial associations, either directly or through immediate family, in areas such as expert testimony, consulting, honoraria, stock holdings, equity interest, ownership, patent-licensing situations or employment that might pose a conflict of interest to this analysis. Additionally, the authors have no conflicts such as personal relationships or academic competition to disclose. The findings presented in this paper represent the views of the named authors only, and not the views of their institutions or organizations.
Acknowledgements
We appreciate the significant time and effort involved with data collection for this project. We would also like to thank all the women who volunteered to participate in this study and provided evidence of their birth experience.
Funding
Funding for this project comes primarily from the Doris Duke Charitable Foundation with additional support from the Eunice Kennedy Shriver National Institutes of Child Health and Human Development Women’s Reproductive Health Research K12 award of the primary author (5K12HD001271).
References
- Betran AP, Ye J, Moller AB, et al. The Increasing Trend in Caesarean Section Rates: Global, Regional and National Estimates: 1990-2014. PLoS One 11 (2016): e0148343.
- ACOG Practice Bulletin No. 205: Vaginal Birth After Cesarean Delivery. Obstet Gynecol 133 (2019): e110-e127.
- ACOG Committee Opinion No. 761: Cesarean Delivery on Maternal Request. Obstetrics and gynecology 133 (2019): e73-e77.
- Grobman W, Lai Y, Landon M, et al. Does Information Available at Admission for Delivery Improve Prediction of Vaginal Birth after Cesarean? American Journal of Perinatology 26 (2009): 693-701.
- Grobman WA. Vaginal Birth After Cesarean (2007).
- Margo S Harrison, Ana L Garces, Shivaprasad S Goudar, et al. Cesarean birth in the Global Network for Women’s and Children’s Health Research: trends in utilization, risk factors, and subgroups with high cesarean birth rates. Reproductive Health 17 (2020).
- REDCap (2019).
- Young CB, Liu S, Muraca GM, et al. Mode of delivery after a previous cesarean birth, and associated maternal and neonatal morbidity. Canadian Medical Association Journal 190 (2018): E556-E564.
