Low Serum Magnesium Level is Associated with Hypertension in Bangladeshi Adults
Article Information
Shihab Md. Rezoyanur Rahman1*, A. K. M Shahidur Rahman2, Amit Kumar Pramanik3, Rokshana Begum4, Khandoker Abdur Rahim5, Mst. Shaila Yesmin4, Mohammad Monzurul Alam Bhuiyan4, Mohammad Tanvir Islam6, Mahfuja Rahman7, Md. Saiful Islam4, Tuhin Sultana4
1Department of Pathology and Blood Transfusion, Gaibandha General Hospital, Gaibandha, Bangladesh
2Department of Nephrology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
3Department of Transfusion Medicine, Rajshahi Medical College Hospital, Rajshahi, Bangladesh
4Department of Laboratory Medicine, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
5Department of Orthopaedic surgery, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
6Department of Internal Medicine, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
7Department of Biochemistry, Bangladesh Medical College, Dhaka, Bangladesh
*Corresponding author: Shihab Md. Rezoyanur Rahman, Department of Pathology and Blood Transfusion, Gaibandha General Hospital, Gaibandha, Bangladesh.
Received: 19 January 2023; Accepted: 27 January 2023; Published: 02 February 2023
Citation: Rahman SMR, Rahman AS, Pramanik AK, Begum R, Rahim KA, Yesmin MS, Bhuiyan MMA, Islam MT, Rahman M, Islam MS, Sultana T. Low Serum Magnesium Level is Associated with Hypertension in Bangladeshi Adults. Fortune Journal of Health Sciences 6 (2023): 31-37.
Share at FacebookAbstract
Background: Hypertension is a global health epidemic which is the leading cause of mortality and morbidity in adult population. Trace element deficiencies are linked to the development of hypertension and its complications. Serum magnesium is a potential biomarker for prediction of magnesium status in body. One of the major homeostatic functions of magnesium is to regulate blood pressure (BP). Objective: This study was aimed to evaluate the association of serum magnesium with hypertension in Bangladeshi adult population.
Methods: This cross-sectional study was conducted at Department of Laboratory Medicine, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh from March 2020 to February 2021. A total of 100 adults (age ≥18 years) were enrolled purposively following selection criteria. Of them, 50 were diagnosed cases of hypertensive patients and rest 50 were normotensive healthy subjects as control group. Both hypertensive and normotensive group were selected according to blood pressure (BP) measurement and history taking. Their anthropometric measurements were done and body mass index (BMI) was calculated accordingly. Estimation of serum magnesium was done by automated biochemistry analyzer (BECKMAN COULTER, AU680), using the principle of photometric technique. All data were analyzed and compared by statistical tests.
Results: The mean(±SD) age was found 46.9±12.7 years in hypertensive individuals and that was 43.1±8.5 years in normotensive individuals. Male were predominant in both groups. Majority of the hypertensive patients were found over-weight. Mean(±SD) serum magnesium level was 1.73±0.24 mg/dl in hypertensive group and that was 2.02±0.19 mg/dl in normotensive group. It was observed that, mean(±SD) serum magnesium level was significantly lower in hypertensive group compared to control group (p<0.001). In hyperten
Keywords
Adult Population; Blood Pressure; Hypertension; Serum Magnesium
Adult Population Articles; Blood Pressure Articles; Hypertension Articles; Serum Magnesium Articles
Article Details
1. Introduction
Hypertension is a condition characterized by persistently elevated pressure in the blood vessels [1]. Hypertension is defined as having a systolic blood pressure ≥140 mmHg and/or a diastolic blood pressure ≥90 mmHg on two separate occasions [2]. According to World Health Organization (WHO), about 1.13 billion adult people worldwide have hypertension [3]. In South Asia, prevalence of hypertension was ranged from 17.9% to 33.8% in adult population [4]. Hypertension is divided into two classes: primary or essential hypertension and secondary hypertension [1]. Majority of the patients suffer from primary or essential hypertension of unknown etiology [1]. High salt intake, lack of trace elements (zinc, magnesium, and potassium) in diet, lack of physical activity, smoking and stress are the risk factors for primary or essential hypertension [5]. Only 5-10% patients have secondary hypertension which is influenced by pre-existing chronic diseases [6]. Hypertension is a significant risk factor for a variety of cardiovascular diseases, cerebrovascular disease, and chronic kidney disease [7].
Trace elements are recognized as necessary for optimal human health and well-being [5, 7, 8]. Trace elements have an impact on fluid and electrolyte balance, as well as acid-base balance and neuromuscular functions [8]. Magnesium (Mg) is the fourth most abundant mineral in human and plays an important physiological role in the body [9]. Magnesium contributes to the synthesis of numerous proteins in our body and functions as a cofactor in a number of body's enzymes [9]. Magnesium plays a key role in homeostasis by regulating blood pressure (BP) [9]. Magnesium has modulating effects on vascular tone and reactivity, acts as a calcium channel antagonist to stimulate production of prostacyclin and nitric oxides [9]. These vasodilator substances then cause endothelin dependent and independent vasodilation [10]. Magnesium deficiency is associated with altered glucose homeostasis, atherosclerotic vascular disease, myocardial infarction, osteoporosis, migraine, asthma [11, 12]. Serum magnesium concentrations can predict an increased cardiovascular mortality [13]. Low serum magnesium level results in vasoconstriction, increased peripheral resistance and finally progress to hypertension [14, 15, 16]. Magnesium deficiency is associated with development of essential hypertension and dyslipidemia [5, 7, 11-15]. Prospective cohort studies and clinical trials found magnesium supplementation has blood pressure lowering effects [5]. Magnesium reduces blood pressure by improving vascular stiffness, reducing vascular resistance and lowering circulatory volume [5, 7]. It was reported that, magnesium supplementation may be beneficial as a therapeutic strategy in hypertensive individuals to reduce complications [5, 7, 17, 18]. This study was aimed to evaluate possible association of serum magnesium with hypertension in Bangladeshi adults.
2. Materials and Methods
2.1 Study design
This cross-sectional study was conducted at Department of Laboratory Medicine, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh from March 2020 to February 2021. This research protocol was approved by the institutional review board (IRB), BSMMU, Dhaka, Bangladesh.
2.2 Study population
A total of 100 Bangladeshi adults (age ≥18 years) of both sexes were enrolled by purposive sampling method following selection criteria. Of them, 50 were diagnosed cases of hypertensive patients (group I) and rests 50 were age matched normotensive healthy subjects as control group (group II). In this study, newly diagnosed hypertensive patients and old cases of hypertension with or without drugs were included. Hypertensive patients with any co-morbidity (like- diabetes mellitus, heart disease, cerebrovascular disease, renal/hepatic impairment, malignancy etc), patients having obesity, patients with recent infection, pregnant and lactating women, subjects receiving magnesium supplements and patients receiving medication influencing serum magnesium level (such as- thiazide and loop diuretics, aminoglycosides, amphotericin B, long term use of proton pump inhibitors, cyclosporine, cisplatin etc) were excluded from this study.
2.3 Study procedure
All the study populations were selected from out-patients department (OPD), Department of Medicine, BSMMU, Dhaka, Bangladesh. Informed written consent was taken from each study subject prior to enrollment. Both hypertensive and normotensive group were selected according to blood pressure measurement and careful history taking. Their anthropometric measurements were done and body mass index (BMI) was calculated accordingly. Then their baseline investigations such as- serum lipid profile, fasting plasma glucose, HbA1C, serum creatinine and serum ALT were done.
2.4 Blood pressure (BP) measurement
In case of new patients, two readings from separate day or home reading for three consecutive days with average reading helped us in the diagnosis of the patients. For blood pressure (BP) measurement, the subjects were asked to sit relaxed in an armed chair for 15 minutes in a quiet room with comfortable room temperature. The mercury manometer was set at his/her heart level. It was necessary that abstinence from caffeine ingestion before 30 minutes of measurement of BP. Then blood pressure (BP) was recorded in all subjects using a standard sphygmomanometer having a cuff size of 25 cm × 12.5 cm. The BP was recorded 2 times by auscultatory method, and the mean value was taken for analysis. Those who were already diagnosed previously as a case of hypertension were included with present BP measuring along with elaborative drugs and lifestyle history (exercise, calorie intake etc).
2.5 Blood sample collection, processing and analysis
With all aseptic precaution 6 ml venous blood was collected from each study subjects. About 2.0 ml venous blood was collected into plastic red colour screw-capped plain tube without anticoagulant for serum, 2.0 ml into EDTA tube for whole blood and 2.0 ml into ash colour screw capped tube containing sodium fluoride anticoagulant for plasma. Vial was labeled with the patient’s identification number, name of investigations, date and time of collection. Collected blood sample was kept in upright position for 30 minutes. Blood was centrifuged at 3000 rpm for 5 minutes. Then serum and plasma sample was collected in a sample cup or eppendorf and marked accordingly. Separated serum was stored in -20°C temperature until analysis was done in Department of Biochemistry and Molecular Biology, BSMMU. Serum magnesium was measured in automated biochemistry analyzer (BECKMAN COULTER, AU680) by using the principle of photometric technique.
2.6 Reference value
The normal reference value for serum magnesium level (1.82-2.43 mg/dl) used in this study was according to the Biochemistry Laboratory, Department of Biochemistry and Molecular Biology, BSMMU, Dhaka, Bangladesh.
2.7 Statistical analysis
All collected data were checked and verified thoroughly to reduce inconsistency. Then data were edited, coded and entered into computer. Data was analyzed by computer-based software program Statistical Package for Social Sciences (SPSS) for windows version 26. Results of the analysis were expressed as mean ± standard deviation (SD) and frequency with percentage. Unpaired t-test, Chi-squared Test (c2) and Pearson’s correlation coefficient test were performed for the statistical analysis of data. A p value <0.05 was considered as the statistically significant value.
3. Results
This cross-sectional study was intended to evaluate the association of serum magnesium with hypertension among Bangladeshi adult population. The sample size was 100. Among them 50 individuals were in hypertensive group (Group I) and 50 healthy normotensive individuals were in control group (Group II). Both groups were selected according to clinical history, blood pressure measurement and laboratory reports. Data were collected through a pre-designed data collection sheet.
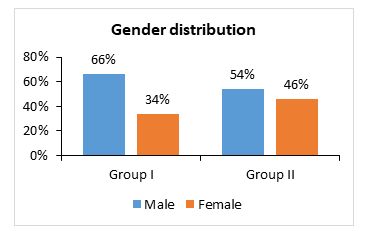
The mean(±SD) age was 46.9±12.7 years for hypertensive group and that was 43.1±8.5 years in control group (p= 0.080). In both groups maximum participants were in 31-40 years age group (Table- 1). In group I; 33(66%) patients were male and 17(34%) patients were female, in group II; 27(54%) patients were male and 23(46%) patients were female (Figure- 1).
Table- 1: Comparison of age among the study groups (N=100)
|
Age (years) |
Group I |
Group II |
p value |
|
(n= 50) |
(n= 50) |
||
|
No. (%) |
No. (%) |
||
|
20-30 |
2(4) |
0(0) |
|
|
31-40 |
20(40) |
24(48) |
|
|
41-50 |
12(24) |
17(34) |
|
|
51-60 |
7(14) |
7(14) |
|
|
>60 |
9(18) |
2(4) |
|
|
Total |
50(100) |
50(100) |
|
|
Mean±SD |
46.9±12.7 |
43.1±8.5 |
0.080 ns |
|
Range |
20 – 65 |
20 - 65 |
Figures in the parentheses indicate the corresponding percentage,
Unpaired student t-test was performed to obtain the p value, ns= not significant
In this study, patients in hypertensive group had significant overweight compared to control group (p=0.017). But, obese individuals (BMI ≥25 kg/m2) were excluded from the study (Table- 2).
Table- 2: Distribution of the study population by body mass index (BMI) (N=100)
|
BMI (kg/m2) |
Group I |
Group II |
p value |
|
(n=50) |
(n=50) |
||
|
No. (%) |
No. (%) |
||
|
Normal BMI (18.5-22.9 kg/m2) |
10(20) |
21(42) |
0.017s |
|
Overweight (23.0-24.9 kg/m2) |
40(80) |
29(58) |
|
|
Total |
50(100) |
50(100) |
Figures in the parentheses indicate corresponding percentage,
Chi-squared Test (c2) was performed to obtain the p value, s = significant
It was observed that, mean(±SD) systolic blood pressure (SBP) [139.6±16.9 mmHg versus 115.1±8.8 mmHg] and mean(±SD) diastolic blood pressure (DBP) [96.2±12.7 mmHg versus 76.7±7.1 mmHg] were significantly higher in hypertensive group compared to control group (p<0.001) (Table- 3).
Table-3: Comparison of blood pressures between the groups (N=100)
|
Blood pressures (BP) |
Group I |
Group II |
p value |
|
(n= 50) |
(n= 50) |
||
|
Mean±SD |
Mean±SD |
||
|
Systolic blood pressure (mmHg) |
139.6±16.9 |
115.1±8.8 |
<0.001s |
|
Diastolic blood pressure (mmHg) |
96.2±12.7 |
76.7±7.1 |
Data were expressed as mean±SD, Unpaired student t-test was performed to obtain the p value, s= significant
Data analysis revealed that, the mean(±SD) serum magnesium level was 1.73±0.24 mg/dl in hypertensive group and that was 2.02±0.19 mg/dl in control group. Mean serum magnesium level was found significantly low in hypertensive group (p<0.001) (Table- 4).
Table-4: Comparison of serum magnesium level between the groups (N=100)
|
Variable |
Group I |
Group II |
p value |
|
(n= 50) |
(n= 50) |
||
|
Mean±SD |
Mean±SD |
||
|
Serum magnesium level (mg/dl) |
1.73±0.24 |
2.02±0.19 |
<0.001s |
Data were expressed as mean±SD, Unpaired student t-test was performed to obtain the p value, s= significant
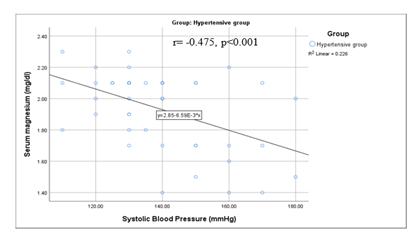
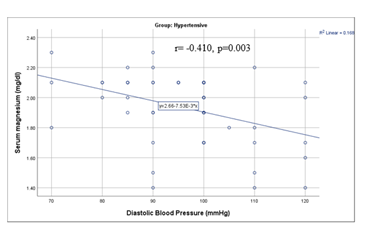
We found that serum magnesium level (S. Mg) had significant moderate negative correlation with systolic blood pressure (SBP) (r= -0.475, p<0.001) and diastolic blood pressure (DBP) (r= -0.410, p= 0.003) in hypertensive group (Table- 5).
Table-5: Correlation of serum magnesium and with blood pressures [systolic blood pressure (SBP) and diastolic blood pressure (DBP)] in hypertensive group (N=50)
|
Variable |
SBP (mmHg) |
DBP (mmHg) |
|
|
Serum magnesium (mg/dl) |
r-value |
-0.475 |
-0.41 |
|
p-value |
<0.001* |
0.003* |
|
SBP= systolic blood pressure, DBP= diastolic blood pressure, *significant
Figure- 2 showing that serum magnesium had significant moderate negative correlation with systolic blood pressure (SBP) in hypertensive group (r= -0.475, p<0.001) (Figure- 2).
Figure- 3 displaying that serum magnesium had significant moderate negative correlation with diastolic blood pressure (DBP) in hypertensive group (r= -0.410, p= 0.003) (Figure- 3).
4. Discussion
Hypertension is a complex condition in which multiple factors and mechanisms interact to cause cardiovascular and cerebrovascular complications [1, 19]. Hypertension is a global health epidemic that is the leading cause of mortality and morbidity worldwide [2-3, 19]. It was reported that, deficiencies of trace elements are closely related with development of hypertension and associated complications [19, 20]. Magnesium is the most abundant divalent intracellular cation in the human body and the second most abundant intracellular ion after potassium [19]. Magnesium deficiency is associated with development and adverse clinical outcome of essential hypertension [17, 19-20]. Serum magnesium is a potential biomarker for prediction of magnesium status in the body [17]. Estimation of serum magnesium in hypertensive patients may be helpful for management of hypertension. In this background current study was aimed to evaluate the association of serum magnesium with hypertension among Bangladeshi adult population. A total of 100 adults (age ≥18 years) were enrolled in this study. Of them, 50 were diagnosed cases of hypertensive patients and rests 50 were age matched normotensive healthy subjects as control group. Both hypertensive and normotensive/control group were selected according to blood pressure measurement and history taking along with relevant investigations. Mean(±SD) age in hypertensive group (Group I) was 46.9±12.7 years and that was 43.1±8.5 years in control group (Group II) (p= 0.080). In this study, male patients were predominant in both groups and this finding was consistent with previous studies [16, 18, 21]. It was observed that, 80% individuals were overweight in Group I and that was 58% in Group II. Overweight individuals were significantly higher in hypertensive group compared to normotensive group (p=0.017). In this context several reports revealed that there is significant relationship between BMI with hypertension [19-21,22, 23]. They found respondents with BMI more than normal (overweight or obese) had a higher risk of developing hypertension compared with respondents who had a normal BMI [19-23]. Some studies found micronutrient deficiencies were associated with obesity [20, 22].
The blood pressures of the study population were calculated separately as systolic blood pressure (SBP) and diastolic blood pressure (DBP). Mean(±SD) systolic blood pressure (SBP) was 139.6±16.9 mmHg in hypertensive group and that was 115.1±8.8 mmHg in control group; on the other hand, mean(±SD) diastolic blood pressure (DBP) was 96.2±12.7 mmHg in hypertensive group and that was 76.7±7.1 mmHg in control group. The mean blood pressures (both SBP and DBP) of the hypertensive cases were significantly higher than controls (p<0.001). This finding was comparable with similar previous studies [6, 17, 24, 25]
In this current study, it was observed that mean(±SD) serum magnesium level was 1.73±0.24 mg/dl in hypertensive group and that was 2.02±0.19 mg/dl in normotensive group. Mean serum magnesium level was found significantly lower in hypertensive group than control group (p<0.001). Rekha et al. found that, the mean serum magnesium level in normotensive controls was 2.068±0.4515 mg/dl but it was 1.5560±0.40320 mg/dl in stage 1 hypertensive patients and 1.3920±0.4081 mg/dl in stage 2 hypertensive patients, there was a significant low serum magnesium levels between these hypertensive groups (p<0.05) [26]. Touyz et al. found that mean serum magnesium level in normotensive controls was 2.28±0.17 mg/dl while it was 1.97±0.17 mg/dl in hypertensive patients, the difference was statistically significant (p<0.001) [27]. In accordance, Han et al. in a metanalysis also found similar findings [28]. Results of these previous studies were consistent with this current study [26-28].
Pearson’s correlation coefficient test was done to observe the correlation of serum magnesium with blood pressures (SBP and DBP) in hypertensive group in present study. Serum magnesium had significant moderate negative correlation with SBP (r= -.475, p<0.001) and DBP (r= -.410, p=0.003). In this series, Rekha et al. found a similar negative correlation of serum magnesium with systolic blood pressure (r= -.615, p<0.001) and diastolic blood pressure (r= -.553, p<0.001) among hypertensive patients [26]. Similarly, Ohira et al. also found an inverse relationship between serum magnesium with systolic blood pressure (p<0.001) [29]. Therefore, finding of this current study was supported by couple of related previous studies [26, 29, 30].
This study documented that the mean serum magnesium level was significantly lower in hypertensive group than normotensive/control group. Pearson’s correlation coefficient test revealed that serum magnesium had significant moderate negative correlation with systolic blood pressure (SBP) and diastolic blood pressure (DBP). Therefore, low serum magnesium level was associated with hypertension in Bangladeshi adult population.
5. Conclusion
This study concluded that serum magnesium level is significantly low in hypertensive Bangladeshi adults. Low serum magnesium level has an inverse relationship with hypertension among adult Bangladeshi population. Estimation of serum magnesium may be considered for better management of hypertension.
Limitations of the study
It was a single center study with a relatively small sample size. In this study detailed dietary habit of the study population was not noted. Besides, longitudinal follow-up study to observe the effect of magnesium supplementation in hypertensive individuals was not done.
Recommendations
Further multicenter study with large sample size should be done to identify the optimum cut off value for serum magnesium in hypertensive patients. Long-term follow up studies are recommended for the evaluation of serum magnesium in hypertensive individuals.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the research, authorship, or publication of this article.
References
- Oparil S, Acelajado MC, Bakris GL, Berlowitz DR, Cífková R, Dominiczak AF, et al. Hypertension. Nature reviews. Disease primers 4: 18014.
- Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nature Reviews Nephrology16(2020):223-37.
- World Health Organization. Global Health Observatory (GHO) Data. Blood pressure (2018).
- Neupane D, McLachlan CS, Sharma R, Gyawali B, Khanal V, Mishra SR, et al. Prevalence of hypertension in member countries of South Asian Association for Regional Cooperation (SAARC): systematic review and meta-analysis. Medicine 93(2014).
- Schutten JC, Joosten MM, de Borst MH, Bakker SJ. Magnesium and blood pressure: a physiology-based approach. Advances in chronic kidney disease25(2018):244-50.
- Whelton PK, He J, Muntner P. Prevalence, awareness, treatment and control of hypertension in North America, North Africa and Asia. Journal of human hypertension 18(2004):545-51.
- Rodríguez-Ramírez M, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Madero A, Brito-Zurita O, et al. Prevalence of prehypertension in Mexico and its association with hypomagnesemia. American journal of hypertension 28(2015):1024-30.
- Carpenter WE, Lam D, Toney GM, Weintraub NL, Qin Z. Zinc, copper, and blood pressure: Human population studies. Medical science monitor: international medical journal of experimental and clinical research 19 (2013):1.
- Yogi A, Callera GE, Antunes TT, Tostes RC, Touyz RM. Vascular biology of magnesium and its transporters in hypertension. Magnesium Research 23 (2010):207-15.
- Northcott CA, Watts SW. Low [Mg2+] e enhances arterial spontaneous tone via phosphatidylinositol 3-kinase in DOCA-salt hypertension. Hypertension 43 (2004):125-9.
- Puig JM, Serrallach CP, Vázquez JM. Magnesium metabolism and its disorders. Medicinaclinica87 (1986):159-68.
- Swaminathan R. Magnesium metabolism and its disorders. The Clinical Biochemist Reviews 24 (2003):47.
- Reffelmann T, Ittermann T, Dörr M, Völzke H, Reinthaler M, Petersmann A, et al. Low serum magnesium concentrations predict cardiovascular and all-cause mortality. Atherosclerosis 219 (2011):280-4.
- De Baaij JH, Hoenderop JG, Bindels RJ. Magnesium in man: implications for health and disease. Physiological reviews 95 (2015): 1-46.
- Guerrero-Romero F, Rodríguez-Morán M, Hernández-Ronquillo G, Gómez-Díaz R, Pizano-Zarate ML, Wacher NH, et al. Low serum magnesium levels and its association with high blood pressure in children. The Journal of pediatrics 168 (2016):93-8.
- Pham PC, Pham PM, Pham SV, Miller JM, Pham PT. Hypomagnesemia in patients with type 2 diabetes. Clinical journal of the American Society of Nephrology 2 (2007):366-73.
- Tiwari D, Islam SS, Khan MM. Correlation of serum copper, magnesium and zinc in essential hypertension. Biochem. Cell. Arch 19 (2019):1051-6.
- Dickinson HO, Nicolson D, Campbell F, Cook JV, Beyer FR, Ford GA, Mason J. Magnesium supplementation for the management of primary hypertension in adults. Cochrane Database of Systematic Reviews (2006).
- Dominguez LJ, Veronese N, Barbagallo M. Magnesium and hypertension in old age. Nutrients 13 (2020):139.
- García OP, Long KZ, Rosado JL. Impact of micronutrient deficiencies on obesity. Nutrition reviews 67 (2009):559-72.
- Rahman M, Zaman MM, Islam JY, Chowdhury J, Ahsan HA, Rahman R, et al. Prevalence, treatment patterns, and risk factors of hypertension and pre-hypertension among Bangladeshi adults. Journal of human hypertension 32 (2018):334-48.
- Momtaz M, Mughal N, Siddique A, Mahboob T. Changes in Blood Levels of Trace Elements and Electrolytes In Hypertensive Patients. Medical Journal of The Islamic Republic of Iran (MJIRI) 14 (2000):115-8.
- Bays HE, Chapman RH, Grandy S, SHIELD Investigators’ Group. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: comparison of data from two national surveys. International journal of clinical practice 61 (2007):737-47.
- Alam DS, Chowdhury MA, Siddiquee AT, Ahmed S, Niessen LW. Awareness and control of hypertension in Bangladesh: follow-up of a hypertensive cohort. BMJ open 4 (2014):e004983.
- Dewan Shamsul AL, Chowdhury MA, Siddiquee AT, Ahmed S, Niessen LW. Awareness and Control of Hypertension in Bangladesh–Follow up of a Stroke 36 (2005):1859-63.
- Rekha S, Murugiah J, Raajaseharan SR. Correlation of serum magnesium levels with blood pressure in normotensives and hypertensives. National Journal of Physiology, Pharmacy and Pharmacology 9 (2019):1017.
- Touyz, RM, Milne, FJ, Seftel, HC &Reinach S. Magnesium, calcium, sodium and potassium status in normotensive and hypertensive Johannesburg residents. South African Medical Journal 72 (1987):377-81.
- Han H, Fang X, Wei X, Liu Y, Jin Z, Chen Q, et al. Dose-response relationship between dietary magnesium intake, serum magnesium concentration and risk of hypertension: a systematic review and meta-analysis of prospective cohort studies. Nutrition journal 16 (2017):1-2.
- Ohira T, Peacock JM, Iso H, Chambless LE, Rosamond WD, Folsom AR. Serum and dietary magnesium and risk of ischemic stroke: the Atherosclerosis Risk in Communities Study. American journal of epidemiology 169 (2009):1437-44.
- Resnick LM, Laragh JH, Sealey JE, Alderman MH. Divalent cations in essential hypertension: relations between serum ionized calcium, magnesium, and plasma renin activity. New England Journal of Medicine 309 (1983):888-91.