Lipofilling in Burn Scars: Our Experience
Article Information
Raymond CHALLITA1*, Ziad SLEIMAN1, Ronald CHALLITA2, Elie YAACOUB1, George GHANIME3,4
1Department of Plastic & Reconstructive Surgery, Faculty of Medical Sciences, Lebanese University, Lebanon
2Faculty of Medical Sciences, Lebanese University, Lebanon
3Head Division, Department of Plastic & Reconstructive Surgery, Faculty of Medical Sciences, Lebanese University, Lebanon
4Chair, Department of Surgery, Faculty of Medical Sciences, Lebanese University, Lebanon
*Corresponding Author: Raymond CHALLITA, Department of Plastic & Reconstructive Surgery, Faculty of Medical Sciences, Lebanese University, Lebanon
Received: 12 June 2020; Accepted: 22 June 2020; Published: 26 June 2020
Citation: Raymond CHALLITA, Ziad SLEIMAN, Ronald CHALLITA, Elie YAACOUB, George GHANIME. Lipofilling in Burn Scars: Our Experience. Journal of Surgery and Research 3 (2020): 177-185.
Share at FacebookAbstract
Introduction: Management of burn scars is a challenging and a complex topic. Various surgical and non-surgical options are present. Recently, a minimally invasive procedure known as autologous fat transfer is being used as an alternative technique to surgical excision for scar management. Although fat grafting may be a promising modality for scar management, there is a limited numbers of studies about their use in burn scars.
Methods: We conducted an observational retrospective study for patients referred to our private clinic for the treatment of burn scars and contractures using autologous fat grafts between February 2009 and May 2018. All patients were surgical candidates for burn reconstruction. The end result was the patients’ level of satisfaction and plastic surgeons’ evaluation at 1 year.
Results: 20% (n=40) were mildly satisfied with the results, 50% (n=100) were moderately satisfied, and 30% (n=60) were extremely satisfied. Only 40% of the moderately satisfied patients were willing to undergo more procedures for scar improvement. 45% (n=90) of the patients had a clinical improvement greater than 50%.
Conclusion: Lipofilling can be considered a safe, simple, minimally invasive, and autologous technique for plastic surgeons to benefit from in burn reconstruction before trying more invasive surgical procedures.
Keywords
Burn scars; Burn reconstruction; Lipofilling; Fat filling; Adipocytes derived stem cells; Regenerative medicine
Burn scars articles, Burn reconstruction articles, Lipofilling articles, Fat filling articles, Adipocytes derived stem cells articles, Regenerative medicine articles
Burn scars articles Burn scars Research articles Burn scars review articles Burn scars PubMed articles Burn scars PubMed Central articles Burn scars 2023 articles Burn scars 2024 articles Burn scars Scopus articles Burn scars impact factor journals Burn scars Scopus journals Burn scars PubMed journals Burn scars medical journals Burn scars free journals Burn scars best journals Burn scars top journals Burn scars free medical journals Burn scars famous journals Burn scars Google Scholar indexed journals Burn reconstruction articles Burn reconstruction Research articles Burn reconstruction review articles Burn reconstruction PubMed articles Burn reconstruction PubMed Central articles Burn reconstruction 2023 articles Burn reconstruction 2024 articles Burn reconstruction Scopus articles Burn reconstruction impact factor journals Burn reconstruction Scopus journals Burn reconstruction PubMed journals Burn reconstruction medical journals Burn reconstruction free journals Burn reconstruction best journals Burn reconstruction top journals Burn reconstruction free medical journals Burn reconstruction famous journals Burn reconstruction Google Scholar indexed journals Lipofilling articles Lipofilling Research articles Lipofilling review articles Lipofilling PubMed articles Lipofilling PubMed Central articles Lipofilling 2023 articles Lipofilling 2024 articles Lipofilling Scopus articles Lipofilling impact factor journals Lipofilling Scopus journals Lipofilling PubMed journals Lipofilling medical journals Lipofilling free journals Lipofilling best journals Lipofilling top journals Lipofilling free medical journals Lipofilling famous journals Lipofilling Google Scholar indexed journals Fat filling articles Fat filling Research articles Fat filling review articles Fat filling PubMed articles Fat filling PubMed Central articles Fat filling 2023 articles Fat filling 2024 articles Fat filling Scopus articles Fat filling impact factor journals Fat filling Scopus journals Fat filling PubMed journals Fat filling medical journals Fat filling free journals Fat filling best journals Fat filling top journals Fat filling free medical journals Fat filling famous journals Fat filling Google Scholar indexed journals Adipocytes derived stem cells articles Adipocytes derived stem cells Research articles Adipocytes derived stem cells review articles Adipocytes derived stem cells PubMed articles Adipocytes derived stem cells PubMed Central articles Adipocytes derived stem cells 2023 articles Adipocytes derived stem cells 2024 articles Adipocytes derived stem cells Scopus articles Adipocytes derived stem cells impact factor journals Adipocytes derived stem cells Scopus journals Adipocytes derived stem cells PubMed journals Adipocytes derived stem cells medical journals Adipocytes derived stem cells free journals Adipocytes derived stem cells best journals Adipocytes derived stem cells top journals Adipocytes derived stem cells free medical journals Adipocytes derived stem cells famous journals Adipocytes derived stem cells Google Scholar indexed journals Regenerative medicine articles Regenerative medicine Research articles Regenerative medicine review articles Regenerative medicine PubMed articles Regenerative medicine PubMed Central articles Regenerative medicine 2023 articles Regenerative medicine 2024 articles Regenerative medicine Scopus articles Regenerative medicine impact factor journals Regenerative medicine Scopus journals Regenerative medicine PubMed journals Regenerative medicine medical journals Regenerative medicine free journals Regenerative medicine best journals Regenerative medicine top journals Regenerative medicine free medical journals Regenerative medicine famous journals Regenerative medicine Google Scholar indexed journals non-surgical options articles non-surgical options Research articles non-surgical options review articles non-surgical options PubMed articles non-surgical options PubMed Central articles non-surgical options 2023 articles non-surgical options 2024 articles non-surgical options Scopus articles non-surgical options impact factor journals non-surgical options Scopus journals non-surgical options PubMed journals non-surgical options medical journals non-surgical options free journals non-surgical options best journals non-surgical options top journals non-surgical options free medical journals non-surgical options famous journals non-surgical options Google Scholar indexed journals surgical options articles surgical options Research articles surgical options review articles surgical options PubMed articles surgical options PubMed Central articles surgical options 2023 articles surgical options 2024 articles surgical options Scopus articles surgical options impact factor journals surgical options Scopus journals surgical options PubMed journals surgical options medical journals surgical options free journals surgical options best journals surgical options top journals surgical options free medical journals surgical options famous journals surgical options Google Scholar indexed journals bone marrow stem cells articles bone marrow stem cells Research articles bone marrow stem cells review articles bone marrow stem cells PubMed articles bone marrow stem cells PubMed Central articles bone marrow stem cells 2023 articles bone marrow stem cells 2024 articles bone marrow stem cells Scopus articles bone marrow stem cells impact factor journals bone marrow stem cells Scopus journals bone marrow stem cells PubMed journals bone marrow stem cells medical journals bone marrow stem cells free journals bone marrow stem cells best journals bone marrow stem cells top journals bone marrow stem cells free medical journals bone marrow stem cells famous journals bone marrow stem cells Google Scholar indexed journals
Article Details
Introduction
The practice of an early burn wound excision, the use of silver impregnated dressings, and the improvement in the acute burn care decreased mortality in burn patients [1]. This shifted physicians’ attention to scar contracture management post burn [2]. Management of burn scars is a challenging and a complex topic. Various surgical and non-surgical options are present. Pressure garments, splinting, silicones, laser therapy, massages, and corticosteroids injections are among the non-surgical options [3]. Recently, a minimally invasive procedure known as autologous fat transfer is being used as an alternative technique to surgical excision for scar management with promising results [4]. These fat grafts are said to have a regenerative potential on the damaged tissue [5].
Regenerative medicine is gaining popularity in medicine especially in plastic surgery. It may be one of the greatest advances in plastic surgery in the coming years. It mainly focuses on improving the healing process and promoting the regrowth of soft tissue [6]. Various techniques were used for this purpose [6]. Stem cells play an important role in this process [6]. Embryonic and adult stem cells are present, and they have the ability to differentiate into various cell types [7]. Adult stem cells are present mainly in the bone marrow, but Adipocytes derived stem cells (ADSC) are gaining popularity due to their ease of harvest and their greater regenerative potential when compared to the bone marrow stem cells [5]. This made ADSC an important tool for plastic surgeons to benefit from in scar management [8]. As shown by a literature review done by Riyat et al. various studies have talked about the important role of autologous fat grafting in improving the functional and the cosmetic characteristics of various scars including those occurring post deep burns [4].
Although fat grafting may be a promising modality for scar management, there is a limited numbers of studies about their use in burn scars. To the best of our knowledge, no large epidemiological study showed the impact of fat filling in burn patients. So we conducted this review to evaluate the role of lipofilling in burn scars.
Materials and Methods
We conducted an observational retrospective study for the patients referred to our private clinic for the treatment of burn scars and contractures using autologous fat grafts between February 2009 and May 2018. This clinic is the referral clinic for burn patients in Lebanon and is led by the founder and the responsible of the Lebanese University Hospital Burn Unit in Beirut, the only Burn unit in Lebanon.
The inclusion criteria consisted of patients presenting with cosmetically unpleasant scars post burn and decreased function due to scar contracture. All of the patients were surgical candidates for burn reconstruction using standard surgical techniques. To note that all of the patients were operated at least one year after their initial wound healed.
Exclusion criteria included a previous surgical procedure in the past 6 months.
Patients did not receive any special post-operative treatment and were followed up for 1 year with regular post op visits at 1 week, 1 months, 3 months, 6 months, and 1 year. All of the patients were informed that their images might be anonymously used for scientific purposes at a later stage and their consent was obtained. Moreover, the principles outlined in the Declaration of Helsinki have been followed and respected.
The author’s fat preparation was as follows. Fat cells were harvested from areas of fat excess. These included mainly the abdominal area, the flanks, the thighs, and the knees. A 2 mm incision was made. The area was infiltrated with normal saline, xylocaine, and epinephrine. Fat was harvested by manual suction using a 3mm diameter Coleman cannula attached to a 10cc luer lock syringe. Fat cells were then prepared and filtrated using a funnel. Then the pure fat cells were inserted into multiple 1 cc syringes and injected with Coleman cannulas or sharp needles to overcome the fibrosis post burn.
The entry points were made with a Number 11 blade after applying local anesthesia (xylocaine 1% with adrenaline 1:100,000). Fat cells were then deposited at the deep dermal-hypodermal junction of the scar in small aliquots (0.1 cc each), in a retrograde manner, and in various directions. This small deposition of fat is thought to increase the vascular supply and the survival rate of fat grafts. This procedure is painful and is done with patient sedation.
The end result was the patients’ level of satisfaction and the plastic surgeons’ evaluation at 1 year. Patients noted at 1 year their level of satisfaction (mildly, moderately, or extremely satisfied). Those who were moderately satisfied were asked if they are willing to do further interventions to improve their burn scars.
Two Board certified Plastic Surgeons with an experience in burn care for more than 10 years assessed and reviewed the patients’ charts and pictures pre and post lipofilling. The two surgeons assessed the patients pictures pre op and at one year post op. Moreover, information about the appearance, the vascularization, the pigmentation, the thickness, and the pliability of the scar were also retrieved. Then each surgeon noted the percentage of improvement and the mean value was used. Then these values were then divided into three groups (10% to 20%, 20% to 50%, and >50%).
Results
A total of 215 patients presenting with burn scars were operated using autologous fat grafting. Only 200 patients were included in this study. 15 patients were lost in the follow up at 1 year. The mean patients’ age was 32 years with an age range between 15 and 65 years. Our sample included 110 female (55%) and 90 male patients (45%).
Concerning the areas treated, 47 patients (23.5%) were operated for facial scars, 54 patients (27%) were operated for neck and chest scars, 37 patients (18.5%) were operated for breast scars, and 62 patients (31%) were operated for upper and lower limbs scars.122 patients (61%) required only one lipofilling session, 68 patients (34%) required 2 sessions after 3 months, and only 10 patients (5%) benefited from a third session 3 months after the last procedure.
At 1 year patients’ level of satisfaction was noted by the patients. 20% (n=40) were mildly satisfied with the results, 50% (n=100) were moderately satisfied, and 30% (n=60) were extremely satisfied. For the patients moderately satisfied, only 40% of those patients were willing to undergo more procedures for scar improvement.
Concerning the clinical improvement as judged by the two surgeons, 30% (n=60) of the patients had an improvement of 10% to 20%, 25% (n=50) had an improvement between 20% and 50%, while the other 45% (n=90) had an improvement greater than 50%. The improvement was noted as an improvement in skin texture, softness, thickness, elasticity, and pigmentation (Figures 1,2,3,4).

Figure 1: Patient presenting 1 year after facial Burn. Patient was operated with 1 session of lipofilling. a: preoperative photo. b: post lipofilling results at 1 year with improvement in scar appearance, texture, and mimic features.
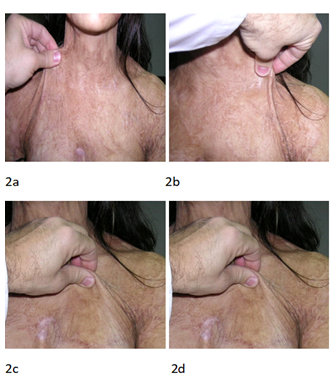
Figure 2: Patient presenting for hypertrophic scarring post neck and chest Burn. a and b: preop, c and d: 1 year post 1 session of lipofilling with improvement in skin texture, elasticity, and pigmentation.
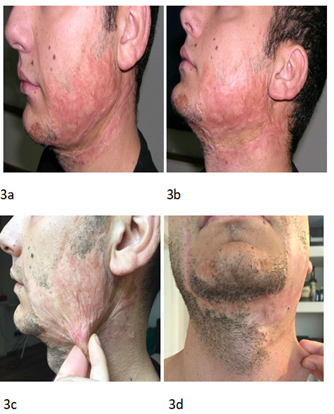
Figure 3: Patient presenting to our clinic seeking improvement in esthetic appearance and function of a facial scar. a and b : preoperative pictures. c and d: postoperative pictures 1 year post two sessions of lipofilling with improvement in scar appearance, elasticity, pigmentation, and thickness.
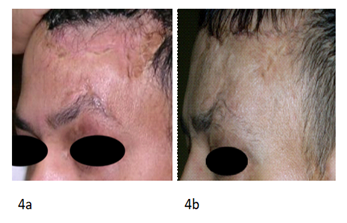
Figure 4: Patient presenting for forehead scar 1 year post burn. a:preoperative picture. b: postoperative picture 1 year post two sessions of lipofilling with improvement in skin texture and decrease in pigmentation.
Moreover, 60% of all the patients noted an improvement in function. Also an improvement in facial mimic features was observed in some patients with facial scars. To note that a number of patients reported an improvement or even the disappearance of their neuropathic pain that occurred post burn.
Finally we did not observe any complication except for mild edema, swelling, and ecchymosis.
Discussion
The use of fat grafts in reconstructive surgery dates back to 1893 by Neuber [5]. Fat grafting techniques were constantly evolving during the years until 1987 where Coleman proposed a new technique to decrease the traumatic handling of the fat cells [9]. Nowadays lipofilling is used in various reconstructive and esthetic procedures. It is used in breast reconstruction, in scar management, in the treatment of radiodermatitis, in lipodystrophy, in facial rejuvenation, in hand rejuvenation, in rhinoplasty, and in breast and gluteal augmentation [5]. Fat grafts have gained a lot of interest recently not only due to its volumetric effect, but also due to its regenerative properties despite the fact that some of the injected fat can be lost over time [10]. These regenerative properties are mainly due to the ADSC that have the potential to differentiate into various cell types [5]. These cells have the ability to secrete various growth factors which can promote wound healing and regeneration [11]. To add to this its important role in scar remodeling by reducing the inflammatory process, by coordinating the immune response, and by secreting the growth factors in a physiologic way [8].
The decline in burn mortality led to an increased prevalence of burn scars and contractures [12]. Burn scar reconstruction is a challenging and continuously evolving concept. Multiple surgical and non-surgical techniques have been described in the literature [12]. Most of these treatments especially surgical once possess a high rate of relapse with the need of further therapies [13]. Various studies talked about the improvement of scar tissue of various causes post autologous fat grafts. Not only esthetic improvement was noted but also functional improvement with decreased pain sensation [4]. An improvement was also noted on the anatomopathological level by increasing keratinocytes regenerative potential [14]. Moreover, Immunohistochemical studies showed that all burn scars even chronic once are always present in a hypervascularized and a hyperinflamatory status [15]. Here comes the role of the ADSC in lipofilling which can reverse this process rendering the tissue more similar to the healthy one and can stimulate the regenerative process [15].
Lipofilling showed promising results in various fields in reconstructive and aesthetic surgery. In scars, this procedure improved the quality of scars both esthetically and functionally [5]. Klinger et al. were the first to talk about lipofilling in burn scars. The huge functional, psychological, and social burden of burn scars led him to study the effect of lipofilling on three patients with burn scars. The preliminary results showed a marked improvement in burn scars quality [16]. Since then multiple studies talked about the role of autologous fat grafts for the treatment of burn scars in small case series [17, 18]. In our large series, however, 215 patients were studied for burn reconstruction using autologous fat grafts. Different levels of patients’ satisfaction and clinical improvement were noted. This improvement was noted on various levels. Skin elasticity, color, texture, thickness, and appearance were improved with various degrees. This improvement obviated the need for more invasive reconstructive surgical procedures. Similarly, brongo et al. mentioned that lipofilling can replace or improve standard surgical techniques for burn reconstruction [17]. Moreover, Khouri et al. suggested that this technique would replace flap reconstruction [19]. In our study, 60% of the patients were satisfied from the cosmetic and functional improvement without expressing the need for further surgeries. This percentage included the patients extremely satisfied and the patients moderately satisfied and that were not willing to do more surgical procedures. To note that all our patients included in the study were surgical candidates for standard surgical treatments, but were treated with lipofilling instead. Thus lipofilling may replace more invasive surgical procedures as noticed in our series.
Recently, autologous fat grafting can be combined with CO2 laser to improve facial scar appearance [20]. This paves the way for the probability of combining fat filling with various noninvasive techniques to improve scaring. More studies are needed to study the association of lipofilling and various dermatological techniques in improving scaring.
These regenerative characteristics of ADSC post fat grafts may improve outcome when combined with standard surgical techniques [21]. Even in cases where surgical treatment would be necessary later on, the improvement in wound characteristics and scar quality might improve and increase the success rate of future surgeries. This improvement in skin texture might render tissue handling in future surgeries easier. Thus, the integration of burn lipofilling in the reconstructive ladder for burn reconstruction might be an effective, simple, and long lasting option.
Although significant improvement was observed in the scars treated by lipofilling in our series, some limitations are present. Our study is a qualitative study with the absence of an objective scoring system for scar assessment and functional assessment. Moreover, the volume injected per area was not constantly recorded with missing data. To add that the study design does not allow the possibility to make evidence based conclusions. No control group is present that allows the comparison between patients undergoing lipofilling and patients undergoing standard surgical procedures. Thus our primary observed results may pave the way for future studies to confirm our hypothesis and try to set the indications, the limitations, and the ideal candidates for fat filling in burn patients.
Conclusion
Autologous fat grafting can be used in various areas of plastic surgery, however, information about its use in burn care is scarce. We presented our experience with fat filling in patients with burn scars. Improvement in the aesthetic and functional outcome was observed which obviated the need for further surgeries in many cases. Although fat resorption rates are variable, in our series, lipofilling was a safe, simple, minimally invasive, and autologous technique to benefit from in burn reconstruction before trying more invasive surgical procedures. Thus future multicentric randomized controlled trials are needed to confirm these findings and try to standardize the role of fat filling in burn reconstruction.
Financial Disclosure
The authors have no conflict of interest to declare.
References
- Sheppard NN, Hemington-Gorse S, Shelley OP, Philp B, Dziewulski P. Prognostic scoring systems in burns: a review. Burns 37 (2011): 1288-95.
- Van Baar ME, Essink-Bot ML, Oen IM, Dokter J, Boxma H, van Beeck EF. Functional outcome after burns: a review. Burns 32 (2006): 1–9.
- Hop MJ, Langenberg LC, Hiddingh J, Stekelenburg CM, van der Wal MB, Hoogewerf CJ, van Koppen ML, Polinder S, van Zuijlen PP, van Baar ME, Middelkoop E. Reconstructive surgery after burns: a 10-year follow-up study. Burns 40 (2014): 1544-51.
- Riyat H, Touil LL, Briggs M, Shokrollahi K. Autologous fat grafting for scars, healing and pain: a review. Scars, burns & healing 3 (2017): 2059513117728200.
- Simonacci F, Bertozzi N, Grieco MP, Grignaffini E, Raposio E. Procedure, applications, and outcomes of autologous fat grafting. Ann Med Surg 20 (2017): 49–60.
- Miller MQ, Dighe A, Cui Q, Park SS, Christophel JJ. Regenerative medicine in facial plastic and reconstructive surgery: a review. JAMA facial plastic surgery 18 (2016): 391-4.
- Zakrzewski W, Dobrzynski M, Szymonowicz M, Rybak Z. Stem cells: past, present, and future. Stem cell research & therapy 10 (2019): 1-22.
- Xu J, Jiang B, Shen Y. Effectiveness of Autologous Fat Grafting in Scaring After Augmentation Rhinoplasty. Journal of Craniofacial Surgery 30 (2019): 914-7.
- Coleman S.R. Structural fat grafting. Aesthet Surg J 18 (1998): 386–388.
- di Santolo MS, Sagnelli M, Tortora G, Santoro MA, Canta PL, Molea G, Schonauer F, Imbriaco M. The utility of the high-resolution ultrasound technique in the evaluation of autologous adipose tissue lipofilling, used for the correction of post-surgical, post-traumatic and post-burn scars. La radiologia medica 121 (2016): 521-7.
- Salgado AJ, Reis RL, Sousa NJ, Gimble JM. Adipose tissue derived stem cells secretome: soluble factors and their roles in regenerative medicine. Curr. Stem Cell Res. Ther 5 (2010): 103–110.
- Goel A, Shrivastava P. Post-burn scars and scar contractures. Indian journal of plastic surgery: official publication of the Association of Plastic Surgeons of India 43 (2010): S63.
- Klinger M, Klinger F, Caviggioli F, et al. Fat Grafting for Treatment of Facial Scars. Clin Plastic Surg 47 (2020): 131–138.
- Kim BS, Gaul C, Paul NE, Dewor M, Stromps JP, Hwang SS, Nourbakhsh M, Bernhagen J, Rennekampff HO, Pallua N. The effect of lipoaspirates on human keratinocytes. Aesthetic surgery journal 36 (2016): 941-51.
- Bruno A, delli Santi G, Fasciani L, Cempanari M, Palombo M, Palombo P. Burn scar lipofilling: immunohistochemical and clinical outcomes. Journal of Craniofacial Surgery 24 (2013): 1806-14.
- Klinger M, Marazzi M, Vigo D, Torre M. Fat injection for cases of severe burn outcomes: a new perspective of scar remodeling and reduction. Aesthetic Plastic Surgery 32 (2008): 465-9.
- Brongo S, Nicoletti GF, La Padula S, Mele CM, D'Andrea F. Use of lipofilling for the treatment of severe burn outcomes. Plastic and reconstructive surgery 130 (2012): 374e-6e.
- Byrne M, O’Donnell M, Fitzgerald L, Shelley OP. Early experience with fat grafting as an adjunct for secondary burn reconstruction in the hand: Technique, hand function assessment and aesthetic outcomes. Burns 42 (2016): 356-65.
- Khouri RK, Smit JM, Cardoso E, Pallua N, Lantieri L, Mathijssen IM, Khouri Jr RK, Rigotti G. Percutaneous aponeurotomy and lipofilling: a regenerative alternative to flap reconstruction?. Plastic and reconstructive surgery 132 (2013): 1280-90.
- La Padula S, Hersant B, Meningaud JP, D’Andrea F. Use of Autologous Fat Graft and Fractiononal Co2 laser to optimize the aesthetic and functional results in patients with severe burn outcomes of the face. Journal of stomatology, oral and maxillofacial surgery 119 (2018): 279-83.
- Al-Hayder S, Gramkow C, Trojahn Kølle SF. Use of autologous fat grafting for the correction of burn scar contracture in the hand: a case report. Case Reports in Plastic Surgery and Hand Surgery 4 (2017): 81-3.
