Knowledge and Associated Factors of Pelvic Organ Prolapse among Women in Ebonyi State, Nigeria
Article Information
Anozie Okechukwu B1,2*, Nwafor Johnbosco I1, Esike Chidi U1,2, Ewah Richard L3,4, Edegbe Felix O5, Obuna Johnson A1,2, Ukaegbe Chukwuemeka I1,2
1Department of Obstetrics and Gynaecology, Alex Ekwueme Federal University Teaching Hospital, Abakaliki, Ebonyi State, Nigeria
2Department of Obstetrics and Gynaecology, Ebonyi State University, Abakaliki, Nigeria
3Department of Anasthesia, Alex Ekwueme Federal University Teaching Hospital, Abakaliki, Ebonyi State, Nigeria
4Department of Anasthesia, Ebonyi State University, Abakaliki, Nigeria
5Department of Morbid Anatomy, Ebonyi State University, Abakaliki, Nigeria
*Corresponding Author: Anozie Okechukwu B, Department of Obstetrics and Gynaecology, Alex Ekwueme Federal University Teaching Hospital, Abakaliki, Ebonyi State, Nigeria
Received: 22 April 2020; Accepted: 30 April 2020; Published: 04 May 2020
Citation:
Anozie Okechukwu B, Nwafor Johnbosco I, Esike Chidi U, Ewah Richard L, Edegbe Felix O, Obuna Johnson A, Ukaegbe Chukwuemeka I. Knowledge and Associated Factors of Pelvic Organ Prolapse among Women in Ebonyi State, Nigeria. Journal of Women’s Health and Development 3 (2020): 101-113.
Share at FacebookAbstract
Introduction: Despite high prevalence of pelvic organ prolapse in low-resource settings and its negative effect on the quality of life of women affected by the condition, women in resource-constrained settings often have limited knowledge about the condition which limits their ability to seek medical treatment.
Aim: To assess the knowledge and associated factors of pelvic organ prolapse among women in Ebonyi State, Nigeria.
Materials and Methods: This was an interviewer-administered questionnaire-based cross-sectional study conducted among 302 women from 13th to 17th January, 2020 in Abakaliki, Ebonyi State. The participants were randomly selected and Pelvic organ prolapse knowledge questionnaire and incontinence knowledge questionnaire (PIKQ) was used to collect the data. SPSS version 22 was used for data processing and analysis. Descriptive statistics were calculated for most variables. Multivariable logistic regression was used to identify the associated factors. A variable was considered significant at p-value<0.05.
Results: A total of 302 women participated in this study with a mean age of 56.5 ± 9.8 years. Of these participants, 286 (94.7%) had awareness of pelvic organ prolapse and 47 (19.7%) had good knowledge of the condition. Age between 46 and 50 years (AOR = 7.165, 95%CI = 1.749 - 29.357, P = 0.006), occupation such as farming (AOR = 16.812, 95%CI = 9.749 - 55.620, P < 0.0001) and civil service (AOR = 18.691, 95%CI = 6.825 - 86.094, P < 0.0001), having primary education (AOR = 8.098, 95%CI = 7.773 - 8.907, P < 0.0001) or secondary education (AOR = 12.34, 95%CI = 1.654 - 6.342, P = 0.01) were associated with good knowledge of pelvic organ prolapse.
Conclusion: The level of knowledge regarding pelvic organ prolapse was low among study participants which indicates a
Keywords
Knowledge; Associated factors; Pelvic organ prolapse; Postmenopausal women
Knowledge articles Knowledge Research articles Knowledge review articles Knowledge PubMed articles Knowledge PubMed Central articles Knowledge 2023 articles Knowledge 2024 articles Knowledge Scopus articles Knowledge impact factor journals Knowledge Scopus journals Knowledge PubMed journals Knowledge medical journals Knowledge free journals Knowledge best journals Knowledge top journals Knowledge free medical journals Knowledge famous journals Knowledge Google Scholar indexed journals Associated factors articles Associated factors Research articles Associated factors review articles Associated factors PubMed articles Associated factors PubMed Central articles Associated factors 2023 articles Associated factors 2024 articles Associated factors Scopus articles Associated factors impact factor journals Associated factors Scopus journals Associated factors PubMed journals Associated factors medical journals Associated factors free journals Associated factors best journals Associated factors top journals Associated factors free medical journals Associated factors famous journals Associated factors Google Scholar indexed journals Pelvic organ prolapse articles Pelvic organ prolapse Research articles Pelvic organ prolapse review articles Pelvic organ prolapse PubMed articles Pelvic organ prolapse PubMed Central articles Pelvic organ prolapse 2023 articles Pelvic organ prolapse 2024 articles Pelvic organ prolapse Scopus articles Pelvic organ prolapse impact factor journals Pelvic organ prolapse Scopus journals Pelvic organ prolapse PubMed journals Pelvic organ prolapse medical journals Pelvic organ prolapse free journals Pelvic organ prolapse best journals Pelvic organ prolapse top journals Pelvic organ prolapse free medical journals Pelvic organ prolapse famous journals Pelvic organ prolapse Google Scholar indexed journals Postmenopausal women articles Postmenopausal women Research articles Postmenopausal women review articles Postmenopausal women PubMed articles Postmenopausal women PubMed Central articles Postmenopausal women 2023 articles Postmenopausal women 2024 articles Postmenopausal women Scopus articles Postmenopausal women impact factor journals Postmenopausal women Scopus journals Postmenopausal women PubMed journals Postmenopausal women medical journals Postmenopausal women free journals Postmenopausal women best journals Postmenopausal women top journals Postmenopausal women free medical journals Postmenopausal women famous journals Postmenopausal women Google Scholar indexed journals anatomical articles anatomical Research articles anatomical review articles anatomical PubMed articles anatomical PubMed Central articles anatomical 2023 articles anatomical 2024 articles anatomical Scopus articles anatomical impact factor journals anatomical Scopus journals anatomical PubMed journals anatomical medical journals anatomical free journals anatomical best journals anatomical top journals anatomical free medical journals anatomical famous journals anatomical Google Scholar indexed journals uterine prolapse articles uterine prolapse Research articles uterine prolapse review articles uterine prolapse PubMed articles uterine prolapse PubMed Central articles uterine prolapse 2023 articles uterine prolapse 2024 articles uterine prolapse Scopus articles uterine prolapse impact factor journals uterine prolapse Scopus journals uterine prolapse PubMed journals uterine prolapse medical journals uterine prolapse free journals uterine prolapse best journals uterine prolapse top journals uterine prolapse free medical journals uterine prolapse famous journals uterine prolapse Google Scholar indexed journals physician articles physician Research articles physician review articles physician PubMed articles physician PubMed Central articles physician 2023 articles physician 2024 articles physician Scopus articles physician impact factor journals physician Scopus journals physician PubMed journals physician medical journals physician free journals physician best journals physician top journals physician free medical journals physician famous journals physician Google Scholar indexed journals sensitization articles sensitization Research articles sensitization review articles sensitization PubMed articles sensitization PubMed Central articles sensitization 2023 articles sensitization 2024 articles sensitization Scopus articles sensitization impact factor journals sensitization Scopus journals sensitization PubMed journals sensitization medical journals sensitization free journals sensitization best journals sensitization top journals sensitization free medical journals sensitization famous journals sensitization Google Scholar indexed journals sociodemographic articles sociodemographic Research articles sociodemographic review articles sociodemographic PubMed articles sociodemographic PubMed Central articles sociodemographic 2023 articles sociodemographic 2024 articles sociodemographic Scopus articles sociodemographic impact factor journals sociodemographic Scopus journals sociodemographic PubMed journals sociodemographic medical journals sociodemographic free journals sociodemographic best journals sociodemographic top journals sociodemographic free medical journals sociodemographic famous journals sociodemographic Google Scholar indexed journals uterovaginal articles uterovaginal Research articles uterovaginal review articles uterovaginal PubMed articles uterovaginal PubMed Central articles uterovaginal 2023 articles uterovaginal 2024 articles uterovaginal Scopus articles uterovaginal impact factor journals uterovaginal Scopus journals uterovaginal PubMed journals uterovaginal medical journals uterovaginal free journals uterovaginal best journals uterovaginal top journals uterovaginal free medical journals uterovaginal famous journals uterovaginal Google Scholar indexed journals
Article Details
1. Introduction
Pelvic Organ Prolapse is the descent of the pelvic organs from their normal position in the pelvis into the vagina, accompanied by urinary, bowel, sexual or local symptoms [1]. It is a very common gynaecological condition especially in multiparous and postmenopausal women [2]. It is due to defects in the support structures of the uterus and vagina namely the uterosacral ligaments, the cardinal ligaments complex and connective tissue of the urogenital membrane [2]. The true incidence of this disorder is not known because many of the cases are asymptomatic and many women feel shy to complain of pelvic organ prolapse [1, 3]. The global prevalence of uterine prolapse was estimated to be 2-20% [2]. The incidence of prolapse in African society is difficult to determine with accuracy as most of the women do not seek medical attention unless symptoms are pronounced and disturbing [3]. This is even more so in the rural areas. In Nigeria, majority of studies on prevalence of uterovaginal prolapse are institutional and none were carried out in the community [3]. A rural community survey revealed a prevalence of uterovaginal prolapse of 14% in Gambia, West Africa [4].
The development of pelvic organ prolapse is multifactorial [5]. The leading process for the uterovaginal prolapse is the childbirth trauma, which causes weakness of the ligaments, muscular and fascial structures, which were entrusted with the maintenance of anatomical support of pelvic organs [6]. It is commonly due to unsupervised and quick succession of child birth which gives rise to trauma to these vital supports [7], and in due course of time it gets worsen with the setting of menopause [8]. Some of the additional causes are poor socioeconomic status, malnutrition, early marriage, multiparity, and lack of puerperal rehabilitation [9]. This is further complicated by chronic illness like chronic obstructive pulmonary disease, chest tuberculosis, and obesity [9].
In Nigeria, uterine prolapse appeared to be widespread, but little or no published evidence exists to know the level of knowledge of uterovaginal prolapse among women [10]; hence the need for this study. Pelvic organ prolapse is a reproductive health condition that has not received sufficient attention despite its high prevalence in Nigeria [11]. Uterovaginal prolapse has been unsatisfactorily addressed and is a sensitive topic among women, families, and communities. Most women hide the condition due to embarrassment, leading to personal problems such as domestic violence [10, 11]. Lack of knowledge of pelvic floor disorders can make patients reluctant to seek professional care so that they remain dissatisfied [12]. Patients may not discuss their problems with a physician because of lack of understanding and a belief that pelvic floor disorders are a normal consequence of age [13]. Studies had found that a low level of knowledge of pelvic floor disorders is associated with a high prevalence of pelvic floor dysfunction, and that health education is associated with an increase in quality of life and a decrease in pelvic floor symptoms [14]. Some authors have suggested that the level of knowledge and patient perception of pelvic organ prolapse are important predictors of treatment seeking or nonseeking behavior [15]. Therefore, this study aimed to assess the level of knowledge and the associated factors of uterovaginal prolapse among women in Ebonyi State. Findings of this study could be useful in the development of strategic health promotion programs for the prevention of pelvic organ prolapse that target the general population of women and encourage women with the condition to seek medical care.
2. Materials and Methods
2.1 Study design, period and area
This is a cross-sectional study that was conducted among rural women that gathered at the National Obstetric Fistula Centre (NOFIC), Abakaliki from 13th to 17th January, 2020. Each year, Ebonyi state government conducts sensitization exercise to educate rural women on the prevention of obstetric fistula. The women were drawn from the 13 local government area of Ebonyi state and were gathered at the NOFIC for the sensitization program. Ebonyi state is one of the five states in the South-east geopolitical zone of Nigeria. Abakaliki is a semi-urban area and the capital of Ebonyi State, Nigeria. The population comprises mainly of subsistence farmers and petty traders. Christianity forms their major religion and the inhabitants are predominantly Igbo speaking. There are several government owned institutions in the town including Alex Ekwueme Federal University Teaching Hospital and National Obstetric Fistula Centre.
2.2 Study population
All consenting women who participated at the obstetric fistula sensitization program at the National Obstetric Fistula Centre, Abakaliki.
2.3 Study criteria
All women who gave informed consent to participate in the study were included in the study. Participants who had a verbal communication problem and complete loss of hearing were excluded.
2.4 Sample size determination
The sample size was calculated by taking variability of proportion from a similar study which was 14% for knowledge of uterovaginal prolapse [15]. Taking 480 women who participated in the sensitization program as source population and using Open Epi software package for the determination of sample size, the final minimum sample size was calculated as 260. After considering 10% non-response rate for any unpredictable events and design effect of 1.5, the final required sample size was 286. However, 302 women were recruited for the study.
2.5 Sampling technique
The study participants were selected by using simple random sampling method and the first participant was selected by using lottery method.
2.6 Study variables
The study variables were divided into three areas: 1) knowledge about UV prolapse (i.e., ever heard about UV prolapse, multiple variables regarding symptoms and preventive measures of UV prolapse, proportion of the number of variables on knowledge assessment questions, and average or more knowledge about UV prolapse); 2) media exposure to access information about UV prolapse; and 3) sociodemographic characteristics (i.e., age, ethnic group, parity, marital status, occupation, level of education, and husband’s level of education). The variables used to assess the knowledge on UV prolapse for symptoms of UV prolapse were 1) difficulty lifting loads, 2) experiencing lower abdominal pain, 3) having a sagging uterus, 4) feeling pain during sexual activity, 5) difficulty controlling urine and to take preventive measures for UV prolapse, 6) not lifting heavy loads during the post-natal period, 7) eating nutritious foods during pregnancy and the post-natal period, 8) taking adequate rest during the post-natal period, 9) practicing family planning and birth spacing, 10) avoiding early pregnancy, 11) using institutional delivery, and 12) using safe abortion services.
2.7 Operational definition
2.7.1 Good knowledge: Participants who scored ≥ 60% (score 21 - 34) of Pelvic organ Prolapse knowledge (POPK) questionnaire.
2.7.2 Poor knowledge: Women who scored < 60% (score up to 20) on POPK questionnaire.
2.7.3 Awareness: Participants were classified as being aware of pelvic organ prolapse if a positive response (‘Yes’) is obtained to the question ‘have you ever heard of pelvic organ prolapse?’
2.7.4 Data collection tools and procedures: A structured interviewer-administered Pelvic organ prolapse knowledge questionnaire (POPKQ), a 17-item scale was used to assess patient knowledge of POP. The questionnaire was derived from the knowledge of pelvic organ prolapse part of Prolapse and incontinence knowledge questionnaire (PIKQ) [12]. The questionnaire was modified to include socio-demographic characteristics of the participants. The scoring system of women’s knowledge of uterovaginal prolapse was either 2 (for correct answer) or 0 (for incorrect answer). The minimum score was 0 whereas the maximum score was 34. Previous study was used for the classification of study participants’ knowledge level [16].
The reliability of the questionnaire was checked by conducting a pretest among women in Abakaliki town, by taking 5% of the sample size. From the pretest, understandability, clarity, and organization of the questionnaire were checked. From the reliability test of knowledge questions, 0.896 Cronbach’s alpha value was found. The questionnaire was prepared in English language and then translated to Igbo (local language in Abakaliki) that was used for data collection and re-translated back to English to check its consistencies. The questionnaire was then refined accordingly for final use. Five trained house officers participated in data collection. The data collectors were trained for 2 days on the techniques of data collections. The training also included the importance of disclosing the possible benefit and purpose of the study to the study participants before the start of data collection.
2.7.5 Data quality control and analysis: The principal researcher checked completeness and consistency of questionnaires filled by the data collectors to ensure the quality of data. The collected data were entered and analyzed using SPSS version 22 (IBM Corp. Amork, New York, U.S.A). Proportions, rates and summary statistics such as mean, the standard deviation were calculated for most variables. Chi-square test or Fisher’s exact test was used for comparison of categorical variables where appropriate. Independent samples t-test was used for comparison of continuous variables. Multivariable logistic regression was used to determine the factors associated with knowledge of pelvic organ prolapse by entering selected independent variables into the model. The variables with a p-value of less than 0.05 were considered statistically significant.
2.7.6 Ethical considerations: This study was approved by the Research and Ethics Review Committee (RERC) of the National Obstetric Fistula Centre, Abakaliki. Informed consent was taken from the study participants after informing the study subjects on study objectives, expected outcomes, and benefits associated with it. Confidentiality of responses was maintained throughout the study.
3. Results
A total of 302 women took part in the study. About 5.3% (16) were not aware of uterovaginal prolapse. Therefore, the analysis was done for the remaining 94.7% (286) of participants who were aware of uterovaginal prolapse. The mean age of the study participants was 56.5 ± 9.8 years with a range of 35 to 75 years. Most of the participants were married (68.9%), grandmultiparous (60.5%), farmers (52.1%) and belong to Igbo tribe (95.1%). Ninety-five participants (33.2%) and their husbands had no formal education (Table 1).
|
Variables |
Total (n=286) n (%) |
Knowledge of UV polapse |
p value |
|
|
Good (n=47) n (%) |
Poor(n=239) n (%) |
|||
|
Age (years) |
||||
|
35-40 |
16 (5.6) |
6 (12.8) |
10 (4.2) |
< 0.0001 |
|
41-45 |
22 (7.7) |
7 (14.9) |
15 (6.3) |
|
|
46-50 |
57 (19.9) |
4 (8.5) |
53 (22.2) |
|
|
51-55 |
46 (16.1) |
16 (34.0) |
30 (12.6) |
|
|
56-75 |
145 (50.7) |
14 (29.8) |
131 (54.7) |
|
|
Mean age ± SD |
56.5 ± 9.8 |
53.9 ± 12.6 |
56.9 ± 9.2 |
0.06 |
|
Parity |
||||
|
0 |
8 (2.8) |
3 (6.4) |
5 (2.2) |
< 0.0001 |
|
1 |
16 (5.6) |
9 (19.1) |
7 (2.9) |
|
|
2-4 |
89 (31.1) |
15 (31.9) |
74 (30.9) |
|
|
≥ 5 |
173 (60.5) |
20 (42.6) |
153 (64.0) |
|
|
Marital status |
||||
|
Married |
197 (68.9) |
36 (76.6) |
161 (67.4) |
< 0.0001 |
|
Single |
9 (3.1) |
6 (12.8) |
3 (1.3) |
|
|
Divorced |
40 (14.0) |
4 (8.5) |
36 (15.1) |
|
|
Widowed |
40 (14.0) |
1 (2.1) |
39 (16.2) |
|
|
Tribe |
||||
|
Igbo |
272 (95.1) |
46 (97.9) |
226 (94.6) |
0.96 |
|
Hausa |
4 (1.4) |
0 (0) |
4 (1.7) |
|
|
Others |
10 (3.5) |
1 (2.1) |
9 (3.7) |
|
|
Occupation |
||||
|
Farming |
149 (52.1) |
12 (25.5) |
137 (57.3) |
0.871 |
|
Artisan |
16 (5.6) |
3 (6.4) |
13 (5.4) |
|
|
Trading |
88 (30.8) |
14 (29.8) |
74 (30.9) |
|
|
Civil servant |
25 (8.7) |
16 (34.0) |
9 (3.8) |
|
|
Unemployed |
8 (2.8) |
2 (4.3) |
6 (2.6) |
|
|
Level of education |
||||
|
No formal education |
95 (33.2) |
4 (8.5) |
91 (38.1) |
< 0.0001 |
|
Primary |
79 (27.6) |
12 (25.5) |
67 (28.0) |
|
|
Secondary |
73 (25.5) |
12 (25.5) |
61 (25.5) |
|
|
Tertiary |
39 (13.7) |
19 (40.5) |
20 (8.4) |
|
|
Husband’s level of education |
||||
|
No formal education |
95 (33.2) |
5 (10.6) |
90 (37.7) |
< 0.0001 |
|
Primary |
53 (18.5) |
10 (21.2) |
43 (17.9) |
|
|
Secondary |
87 (30.4) |
14 (29.8) |
73 (30.5) |
|
|
Tertiary |
51 (17.9) |
18 (38.4) |
33 (13.9) |
|
Table 1: Sociodemographic characteristics of the study participants.
Figure 1 shows the depth of knowledge of uterovaginal prolapse among the participants. Majority (80.3%) of the participants had poor knowledge of uterovaginal prolapse and only 47 (19.7%) women were classified as having good knowledge of the condition.
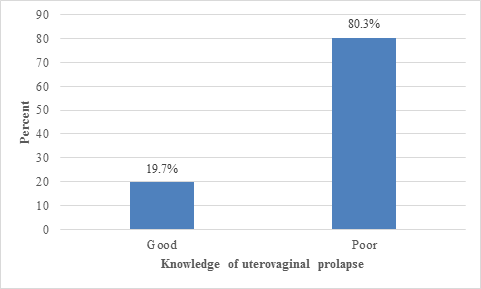
Figure 1: Chart shows the depth of knowledge of uterovaginal prolapse among the participants.
The sources of information on uterovaginal prolapse for the study participants are shown in Figure 2. The commonest source of information for the participants was the health workers (83%), followed by female community health volunteers (8.5%).
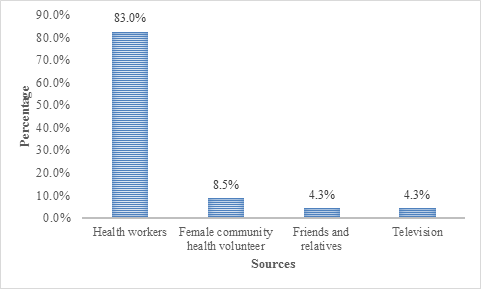
Figure 2: Figure shows the sources of information on uterovaginal prolapse.
Table 2 shows the knowledge of risk factors and symptoms of uterovaginal prolapse. Majority (78%) of the participants reported that menopause increases the risk of uterovaginal prolapse. Other common risk factors reported by the participants were carrying heavy load (19.6%), home delivery (17.1%), chronic cough (14%), and increasing number of vaginal deliveries (45.5%). On symptoms of uterovaginal prolapse, 22.4% of participants mentioned difficulty controlling urine as a symptom of uterovaginal prolapse. Other symptoms known by the participants were dragging sensation (11.1%) and lower abdominal pain (6.9%).
|
Variables |
Total (n=286) n (%) |
Knowledge of UV prolapse |
p value |
|
|
Good (n=47) n (%) |
Poor (n=239) n (%) |
|||
|
Risk factor |
||||
|
Menopausal |
223 (78.0) |
30 (63.8) |
190 (79.5) |
< 0.0001 |
|
Tobacco use |
14 (4.9) |
9 (19.1) |
5 (2.1) |
|
|
Mean age at first pregnancy ± SD |
19.0 ± 2.9 |
22.5 ± 3.4 |
18.4 ± 2.3 |
< 0.0001 |
|
Number of vaginal deliveries |
||||
|
≤ 3 |
30 (10.5) |
4 (8.5) |
26 (10.9) |
0.001 |
|
4-6 |
114 (39.9) |
24 (51.1) |
90 (37.7) |
|
|
7-9 |
130 (45.5) |
12 (25.5) |
118 (49.4) |
|
|
≥ 10 |
12 (4.1) |
7 (14.9) |
5 (2.0) |
|
|
Mean birth spacing interval ± SD |
1.2 ± 0.5 |
1.5 ± 0.5 |
1.2 ± 0.5 |
0.0002 |
|
Home delivery |
49 (17.1) |
7(14.9) |
42 (17.6) |
0.014 |
|
Carry heavy load |
56 (19.6) |
6 (12.7) |
50 (20.9) |
|
|
History of chronic cough |
40 (14.0) |
6 (12.7) |
34 (14.2) |
|
|
History of fibroid |
24 (8.4) |
6 (12.7) |
18 (7.5) |
|
|
History of abortion |
19 (6.6) |
4 (8.5) |
15 (6.3) |
|
|
Experienced malnutrition |
22 (7.7) |
0 (0) |
22 (9.2) |
|
|
Pelvic/abdominal surgery |
16 (5.6) |
8 (17.0) |
8 (3.3) |
|
|
Symptoms |
||||
|
Difficulty lifting loads |
4 (1.4) |
4 (8.5) |
0 (0) |
< 0.0001 |
|
Lower abdominal pain |
20 (6.9) |
18 (38.3) |
2 (0.8) |
|
|
Dragging sensation |
32 (11.1) |
22 (46.8) |
10 (4.2) |
|
|
Pain during intercourse |
4 (1.4) |
2 (4.3) |
2 (0.8) |
|
|
Difficulty controlling urine |
64 (22.4) |
14 (29.8) |
50 (20.9) |
|
Table 2: Knowledge of risk factors and symptoms of uterovaginal prolapse of the study participants.
Knowledge of preventive measures and treatment modalities of uterovaginal prolapse by the study participants are shown in Table 3. Most (60.1%) study participants knew that family planning and birth spacing is a preventive method for the condition. Avoiding early pregnancy (14.3%) and adequate rest during postnatal period (13.3%) were common method of prevention known by the participants. Knowledge of other preventive measures was low. Two hundred and two (70.6%) participants were aware that conservative treatment could be a modality of treatment of uterovaginal prolapse whereas 29.4% of the cohorts mentioned surgery as a form of treatment for the condition.
|
Variable |
Total (n=286) n (%) |
Knowledge of UV prolapse |
p value |
|
|
Good (n=47%) n (%) |
Poor (n=239) n (%) |
|||
|
Preventive measure |
||||
|
Not lifting heavy loads |
2 (0.7) |
1 (2.1) |
1 (0.4) |
0.67 |
|
Eating balanced diet |
2 (0.7) |
0 (0) |
2 (0.8) |
|
|
Adequate rest during postnatal period |
38 (13.3) |
21 (44.6) |
17 (7.1) |
|
|
Family planning and birth spacing |
172 (60.1) |
35 (74.4) |
137 (57.3) |
|
|
Avoiding early pregnancy |
41 (14.3) |
29 (61.7) |
12 (5.0) |
|
|
Hospital delivery |
8 (2.8) |
2 (4.3) |
5 (2.1) |
|
|
Safe abortion practices |
4 (1.4) |
2 (4.3) |
2 (0.8) |
|
|
Adequate treatment of medical conditions (e.g. Chronic cough, uterine fibroid) |
21 (7.3) |
13 (27.7) |
8 (3.3) |
|
|
Method of treatment |
||||
|
Surgery |
84 (29.4) |
35 (74.4) |
49 (20.5) |
0.0001 |
|
Conservative |
202 (70.6) |
40 (85.1) |
162 (67.8) |
|
Table 3: Knowledge of preventive measures and treatment modalities of uterovaginal prolapse among participants (n=286).
Multivariable logistic regression analysis showing predictors of knowledge of uterovaginal prolapse among the study cohorts are shown in table 4. Among the socio demographic variables assessed, age group 46 - 50 years (AOR = 7.165, 95%CI = 1.749 - 29.357, P = 0.006), occupation such farming (AOR = 16.812, 95%CI = 9.749 - 55.620, P < 0.0001) and civil servant (AOR = 18.691, 95%CI = 6.825 - 86.094, P < 0.0001), having primary education (AOR = 8.098, 95%CI = 7.773 - 8.907, P < 0.0001) or secondary education (AOR = 12.34, 95%CI = 1.654 - 6.342, P = 0.01) were associated with good knowledge of uterovaginal prolapse among the study participants.
|
Variable |
Coefficient(B) |
Std. error |
p value |
AOR |
95% CI |
|
Age (years) |
|||||
|
35 - 40 |
0..518 |
1.643 |
0.752 |
1.679 |
0.067 - 42.002 |
|
41 - 45 |
16.125 |
8.760 |
0.995 |
6.903 |
0.876 - 12.320 |
|
46 - 50 |
1.969 |
0.720 |
0.006 |
7.165 |
1.749 - 29.357 |
|
51 - 55 |
-0.236 |
0.657 |
0.719 |
0.790 |
0.218 - 2.862 |
|
56 - 75 |
- |
- |
- |
1.00 |
- |
|
Marital status |
|||||
|
Married |
17.714 |
5.920 |
0.998 |
0.749 |
0.546 - 4.980 |
|
Widowed |
-0.569 |
0.902 |
0.528 |
0.566 |
0.097 - 3.316 |
|
Single |
- |
- |
- |
1.00 |
- |
|
Occupation |
|||||
|
Farming |
16.979 |
1.195 |
< 0.0001 |
16.812 |
9.749 - 55.620 |
|
Trading |
33.029 |
6.106 |
0..984 |
8.030 |
0.876 - 6.991 |
|
Civil servant |
18.085 |
0.988 |
< 0.0001 |
18.691 |
6.825 - 86.094 |
|
Unemployed |
- |
- |
- |
1.00 |
- |
|
Level of education |
|||||
|
No formal education |
-2.576 |
2.368 |
0.998 |
0.076 |
1.118 - 3.196 |
|
Primary |
-19.426 |
0.605 |
< 0.0001 |
8.098 |
7.773 - 8.907 |
|
Secondary |
-18.673 |
0.901 |
0.01 |
12.340 |
1.654 - 6.342 |
|
Tertiary |
- |
- |
- |
1.00 |
- |
|
Husband’s education level |
|||||
|
No formal education |
4.174 |
1.324 |
0.872 |
4.946 |
0.850 - 6.743 |
|
Primary |
2.359 |
1.070 |
0.527 |
1.578 |
0.332 - 8.081 |
|
Secondary |
2.770 |
0.977 |
0.605 |
5.951 |
0.352 - 8.173 |
|
Tertiary |
- |
- |
- |
1.00 |
- |
|
Number of vaginal deliveries |
|||||
|
≥ 10 |
1.126 |
9.878 |
0.542 |
3.082 |
0.435 - 1.210 |
|
7 - 9 |
0.597 |
6.091 |
0.096 |
1.817 |
0.786 - 0.564 |
|
4 - 6 |
1.878 |
5.564 |
0.199 |
6.540 |
0.619 - 1.578 |
|
≤ 3 |
- |
- |
- |
1.00 |
- |
1.00 = Reference category, AOR = Adjusted odd ratio
Table 4: Multivariable logistic regression showing predictors of knowledge of uterovaginal prolapse.
4. Discussion
This study revealed that the proportion of study participants having adequate knowledge of uterovaginal prolapse was 19.7%, which is almost similar with the findings in Egypt (20%) [13] and Nepal (26.8%) [14]. Differently, this finding is lower than the studies in Central Nepal (55%) [15], Moscow (66.7%) [16], Vienna (63.9%) [16] and Connecticut (51.9%) [17]. On the other hand, knowledge of the study participants in this study is slightly higher compared with studies in India (11.1%) [18]. These might be due to variation in the nature of the study settings as some of the studies were hospital-based.
Regarding source of information related to uterovaginal prolapse, 83% of the participants had health workers as the major source of information about the condition. Friends and relatives, and television accounted for 4.3% of information source for the participants. This result is similar to the findings in Moscow and Vienna where participants got information about pelvic organ prolapse from medical specialists (72% and 82%, respectively; p >0.05), followed by friends and family for patients in Vienna (25%), and the internet for patients in Moscow (23%) [16]. Of the patients in Vienna and Moscow, 21% and 14%, respectively, were informed about pelvic organ prolapse by their general practitioner (p > 0.05). Radio and television did not provide enough information in either country (6% and 6% respectively; p>0.05) [16]. In contrast to the findings of this study, a study done in Nepal showed that majority of the participants source of information was radio (53.3%) and television (47.2%), and health workers accounted for 19.5% of information source for the study cohorts [18]. These studies show differences in media preference and availability. These differences may be due to unsatisfactory or nonexistent strategic health communication programs in the media. In addition, most of the study participants in this study resides in the villages which limit their access to media on pelvic organ prolapse-related health information. Therefore, participants in this study preferred to obtain their information from healthcare providers given that the women rated health workers’ opinion as one of the most important factors in making a shared decision about the therapy.
From this study, the knowledge of risk factors and symptoms of uterovaginal prolapse was poor as less than half of the participants had adequate knowledge regarding each risk factors and symptoms of the condition. This finding was similar to the findings of Elsayed in Egypt which showed that majority of the participants had poor knowledge of the risk factors and symptoms of uterine prolapse [19]. In addition, a cross sectional descriptive study conducted by Singh et al., in Nepal revealed that more than half of the studied women had inadequate knowledge on the risk factors and symptoms of uterine prolapse [20]. The similarity in the findings of these studies, regardless of the socio demographic and cultural differences may be because pelvic organ prolapse is a health problem that does not receive sufficient attention in most countries of the world.
The present study also revealed that knowledge of preventive measures of uterine prolapse was inadequate apart from knowledge of family planning and birth spacing (60%) as preventive measure. Also, less than one-third of the study participants were not aware that surgery was a treatment modality for uterine prolapse. These findings differ from findings of a study in Moscow and Vienna [16]. This difference could be due to the fact that women in developing countries do not consider uterovaginal prolapse symptoms as pathologic symptoms but they consider aging process the main etiology for appearance of such symptoms so, they may not seek for the prevention or treatment of the condition.
Among the socio demographic factors, farmers, and civil servants who had formal education (primary or secondary) and are between the ages of 46 and 50 years had good knowledge of uterovaginal prolapse. These findings were different from the findings of a study by Mandimika, et al. in Connecticut, U.S.A which showed that the advanced age, and high education were significantly associated with poor knowledge of pelvic organ prolapse [17]. This difference may be due to education is a major indicator for women's knowledge in developing countries, but because uterine prolapse is a neglected issue in maternity care, even in developed countries with high education there is lack of knowledge regarding this issue. Strengths of this study include the community based approach as the participants were drawn from 13 local government areas of Ebonyi State, Nigeria and the use of validated questionnaire to assess the knowledge of the condition among the participants. Also, there is no published study on the knowledge of women in pelvic organ prolapse in Nigeria. The limitation of the study is that the participants were mainly of Igbo ethnic group from Ebonyi state. Therefore, the monoethnic nature of the study limits the generalization of the study findings to the diverse ethnic groups in Nigeria.
In conclusion, the knowledge of pelvic organ prolapse among the study participants was poor. Therefore, there is need to develop pelvic organ prolapse guidelines aiming at improving women's knowledge and implementation of educational programs/ medical campaigns by health care providers regarding pelvic organ prolapse. This educational program should target women at all places especially in the rural communities for early detection, diagnosis and treatment of the condition. This would encourage women with the condition to seek medical care and help improve their quality of life.
References
- Yakubu A, Panti AA, Ladan AA, Burodo AT, Hassan MA, Nasir S. Pelvic organ prolapse managed at Usmanu Danfodiyo University Teaching Hospital, Sokoto: A 10-year review. Sahel Med J 20 (2017): 26-29.
- Awotunde OT, Fehintola AO, Ogunlaja OA, Olujide LO, Aaron OI, Bakare B, et al. An audit of uterovaginal prolapse in Ogbomoso, south-west Nigeria. Res. J. of Health Sci 4 (2016): 31-37.
- Oraekwe OI, Udensi MA, Nwachukwu KC, Okali UK. Genital prolapse: A 5-year review at Federal Medical Centre Umuahia, Southeastern Nigeria. Niger Med J 57 (2016): 286-289.
- Scherf C, Morison L, Fiander A, Ekpo G, Walraven G. Epidemiology of pelvic organ prolapse in rural Gambia, West Africa. Int J Obstet Gynaecol 109 (2012): 431-436.
- Gjerde JL, Rortveit G, Adefris M, Belayneh T, Blystad A. Life after pelvic organ prolapse surgery: a qualitative study in Amhara region, Ethiopia. BMC Women's Health 18 (2018): 74-80.
- Pant U, Pradhan R, Aryal B. Risk Profile of Uterovaginal Prolapse. JKAHS 2 (2018): 42-46.
- Miller BJ, Seman EI, O’Shea RT, Hakendorf PH, Nguyen TT. Recent trends in the management of pelvic organ prolapse in Australia and New Zealand. Aust N Z J Obstet Gynaecol 59 (2019): 117-122.
- Ibo CC, Ajah LO, Nwafor JI, Ekwuazi KE, Okoro OS, Obi CN, et al. Knowledge and perception of postmenopausal symptoms among postmenopausal women presented at the gynecological clinic of a tertiary health institution in Abakaliki. Trop J Obstet Gynaecol 36 (2019): 437-441.
- Nwafor JI, Obi CN, Obi VO, Ibo CC, Ugoji DPC, Onwe B, et al. Knowledge and determinants of postpartum family planning use among postpartum women in abakaliki south-east Nigeria. Int J Current Research 11 (2019): 3582-3587.
- Asogwa SU, Nwafor JI, Olaleye AA, Ugoji DPC, Obi CN, Ibo CC. Prevalence of Dyspareunia and Its Effect on Sexual Life among Gynaecological Clinic Attendees in Alex Ekwueme Federal University Teaching Hospital Abakaliki, Nigeria. Adv Sexual Med 9 (2019): 110-119.
- Mirskaya M, Lindgren E, Carlsson I. Online reported women’s experiences of symptomatic pelvic organ prolapse after vaginal birth. BMC Women's Health 19 (2019): 129.
- Sha AD, Massagli MP, Kohli N. A reliable, valid instrument to assess patient knowledge about urinary incontinence and pelvic organ prolapse. Int Urogynecol J 19 (2008): 1283-1289.
- Rashad M, Fadel EA, El-Nemer A. Women’s knowledge regarding pelvic organ prolapse. Mansoura Nursing J 6 (2019): 57- 67.
- Subedi S, Thapa T, Joshi A, Chapagain S, Shrestha S. Awareness Regarding Pelvic Organ Prolapse Among Women Attending a Teaching Hospital in Chitwan. Anatol J Family Med 2 (2019): 33-37.
- Shrestha B, Choulagai B, Onta S, Shrestha KB, Petzold M, Krettek A. Knowledge, prevalence and treatment practices of uterine prolapse among women of reproductive age in the Jhaukhel-Duwakot Health Demographic Surveillance Site, Bhaktapur, Nepal. Journal of Kathmandu Medical College 3 (2014): 136-143.
- Lyatoshinskaya P, Gumina D, Popov A, Koch M, Hagmann M, Umek W. Knowledge of pelvic organ prolapse in patients and their information-seeking preferences: comparing Vienna and Moscow. Int Urogynecol J 27 (2016): 1673-1680.
- Mandimika C, Murk W, McPencow A, Lake A, Wedderburn T, Collier C, et al. Knowledge of pelvic floor disorders in a population of community-dwelling women. Am J Obstet Gynecol 210 (2014): 1-9.
- Shrestha B, Devkota B, Khadka BB, Choulagai B, Pahari DP, Onta S, et al. Knowledge on uterine prolapse among married women of reproductive age in Nepal. IJWH 6 (2014): 771-779.
- Elsayed F, Ahmed M, Gaheen M. Knowledge and Practices of women regarding risk factors of uterine prolapse. IOSR Journal of Nursing and Health Science (IOSR- JNHS) 5 (2016): 60-67.
- Singh DR, Lama S, Maharjan S. Knowledge on risk factors of uterine prolapse among reproductive age group women of Bajrabarahi Municipality of Lalitpur, Nepal. Int J Reprod Contracept Obstet Gynecol 5 (2016): 3343-3348.
