Intraoperative Endoscopic Ultrasound Guided Surgical Treatment of Herlyn-Werner-Wunderlich Syndrome. Case Report and a Systematic Literature Review
Article Information
Maria Cristina Moruzzi1, Giulia Bolomini1, Mara Albanese2, Ursula Catena1, Ilaria Romito1, Anna Fagotti1,2, Giovanni Scambia1,2, Antonia Carla Testa1,2
1Department of Women's, Child and Public Health Sciences, Agostino Gemelli University Polyclinic Foundation, Rome, Italy
2Institute of Obstetric and Gynecological Clinic, University of Cattolica del Sacro Cuore, Rome, Italy
*Corresponding Author: Maria Cristina Moruzzi, Department of Women's, Child and Public Health Sciences, Agostino Gemelli University Polyclinic Foundation, IRCCS, L.go A. Gemelli, 8, Rome, Italy
Received: 25 February 2020; Accepted: 05 March 2020; Published: 30 March 2020
Citation:
Maria Cristina Moruzzi, Giulia Bolomini, Mara Albanese, Ursula Catena, Ilaria Romito, Anna Fagotti, Giovanni Scambia, Antonia Carla Testa. Intraoperative Endoscopic Ultrasound Guided Surgical Treatment of Herlyn-Werner-Wunderlich Syndrome. Case Report and a Systematic Literature Review. Obstetrics and Gynecology Research 3 (2020): 037-080.
Share at FacebookAbstract
Aim: Herlyn-Werner-Wunderlich (HWW) syndrome is a rare congenital anomaly characterized by uterus didelphys, obstructed hemivagina, and ipsilateral renal-ureteral agenesis, due to an embryogenesis defect. Clinically, HWW results in hematometrocolpos on the obstructed hemivagina side, which produces a mass effect with pain. The diagnosis is difficult because this syndrome is infrequent, and its clinical presentation is variable. Early detection and treatment are important to prevent further complications that could affect the reproductive performance. Ultrasound (US) is the first step when a Müllerian anomaly is suspected but MRI has a higher accuracy to manage surgery. Surgical treatment consists in vaginal septum excision. This review provides information about HWW syndrome and about its diagnosis and treatment. The main objective of this report is to illustrate the clinical presentation, the ultrasound features of a rare syndrome and the use of a laparoscopic ultrasound guidance to allow a fertility sparing treatment without complications.
Material and Methods: A search of PubMed Database identified articles published from the inception to February 2019.
Results: 186 articles were identified: 125 articles were excluded for any reason. Overall, 63 articles were incorporated for further assessment.
Conclusions: The case reported was treated successfully by minimally invasive surgical drainage procedure supported by full time intraoperative ultrasound guidance. Only few researches described transvaginal and transabdominal probe use during surgery; this is the first case in the literature in which a laparoscopic ultrasound probe was used to guide surgeons in the excision of the vaginal septum to prevent complications and to preserve future fertility.
Keywords
Hematocolpos, Intraoperative Endoscopic Ultrasound, Müllerian Congenital Anomalies, Ultrasonography, Uterine Anomalies
Hematocolpos articles Hematocolpos Research articles Hematocolpos review articles Hematocolpos PubMed articles Hematocolpos PubMed Central articles Hematocolpos 2023 articles Hematocolpos 2024 articles Hematocolpos Scopus articles Hematocolpos impact factor journals Hematocolpos Scopus journals Hematocolpos PubMed journals Hematocolpos medical journals Hematocolpos free journals Hematocolpos best journals Hematocolpos top journals Hematocolpos free medical journals Hematocolpos famous journals Hematocolpos Google Scholar indexed journals Intraoperative Endoscopic Ultrasound articles Intraoperative Endoscopic Ultrasound Research articles Intraoperative Endoscopic Ultrasound review articles Intraoperative Endoscopic Ultrasound PubMed articles Intraoperative Endoscopic Ultrasound PubMed Central articles Intraoperative Endoscopic Ultrasound 2023 articles Intraoperative Endoscopic Ultrasound 2024 articles Intraoperative Endoscopic Ultrasound Scopus articles Intraoperative Endoscopic Ultrasound impact factor journals Intraoperative Endoscopic Ultrasound Scopus journals Intraoperative Endoscopic Ultrasound PubMed journals Intraoperative Endoscopic Ultrasound medical journals Intraoperative Endoscopic Ultrasound free journals Intraoperative Endoscopic Ultrasound best journals Intraoperative Endoscopic Ultrasound top journals Intraoperative Endoscopic Ultrasound free medical journals Intraoperative Endoscopic Ultrasound famous journals Intraoperative Endoscopic Ultrasound Google Scholar indexed journals Müllerian Congenital Anomalies articles Müllerian Congenital Anomalies Research articles Müllerian Congenital Anomalies review articles Müllerian Congenital Anomalies PubMed articles Müllerian Congenital Anomalies PubMed Central articles Müllerian Congenital Anomalies 2023 articles Müllerian Congenital Anomalies 2024 articles Müllerian Congenital Anomalies Scopus articles Müllerian Congenital Anomalies impact factor journals Müllerian Congenital Anomalies Scopus journals Müllerian Congenital Anomalies PubMed journals Müllerian Congenital Anomalies medical journals Müllerian Congenital Anomalies free journals Müllerian Congenital Anomalies best journals Müllerian Congenital Anomalies top journals Müllerian Congenital Anomalies free medical journals Müllerian Congenital Anomalies famous journals Müllerian Congenital Anomalies Google Scholar indexed journals Ultrasonography articles Ultrasonography Research articles Ultrasonography review articles Ultrasonography PubMed articles Ultrasonography PubMed Central articles Ultrasonography 2023 articles Ultrasonography 2024 articles Ultrasonography Scopus articles Ultrasonography impact factor journals Ultrasonography Scopus journals Ultrasonography PubMed journals Ultrasonography medical journals Ultrasonography free journals Ultrasonography best journals Ultrasonography top journals Ultrasonography free medical journals Ultrasonography famous journals Ultrasonography Google Scholar indexed journals Uterine Anomalies articles Uterine Anomalies Research articles Uterine Anomalies review articles Uterine Anomalies PubMed articles Uterine Anomalies PubMed Central articles Uterine Anomalies 2023 articles Uterine Anomalies 2024 articles Uterine Anomalies Scopus articles Uterine Anomalies impact factor journals Uterine Anomalies Scopus journals Uterine Anomalies PubMed journals Uterine Anomalies medical journals Uterine Anomalies free journals Uterine Anomalies best journals Uterine Anomalies top journals Uterine Anomalies free medical journals Uterine Anomalies famous journals Uterine Anomalies Google Scholar indexed journals uterus articles uterus Research articles uterus review articles uterus PubMed articles uterus PubMed Central articles uterus 2023 articles uterus 2024 articles uterus Scopus articles uterus impact factor journals uterus Scopus journals uterus PubMed journals uterus medical journals uterus free journals uterus best journals uterus top journals uterus free medical journals uterus famous journals uterus Google Scholar indexed journals renal-ureteral agenesis articles renal-ureteral agenesis Research articles renal-ureteral agenesis review articles renal-ureteral agenesis PubMed articles renal-ureteral agenesis PubMed Central articles renal-ureteral agenesis 2023 articles renal-ureteral agenesis 2024 articles renal-ureteral agenesis Scopus articles renal-ureteral agenesis impact factor journals renal-ureteral agenesis Scopus journals renal-ureteral agenesis PubMed journals renal-ureteral agenesis medical journals renal-ureteral agenesis free journals renal-ureteral agenesis best journals renal-ureteral agenesis top journals renal-ureteral agenesis free medical journals renal-ureteral agenesis famous journals renal-ureteral agenesis Google Scholar indexed journals female genital articles female genital Research articles female genital review articles female genital PubMed articles female genital PubMed Central articles female genital 2023 articles female genital 2024 articles female genital Scopus articles female genital impact factor journals female genital Scopus journals female genital PubMed journals female genital medical journals female genital free journals female genital best journals female genital top journals female genital free medical journals female genital famous journals female genital Google Scholar indexed journals woman articles woman Research articles woman review articles woman PubMed articles woman PubMed Central articles woman 2023 articles woman 2024 articles woman Scopus articles woman impact factor journals woman Scopus journals woman PubMed journals woman medical journals woman free journals woman best journals woman top journals woman free medical journals woman famous journals woman Google Scholar indexed journals abdominal pain articles abdominal pain Research articles abdominal pain review articles abdominal pain PubMed articles abdominal pain PubMed Central articles abdominal pain 2023 articles abdominal pain 2024 articles abdominal pain Scopus articles abdominal pain impact factor journals abdominal pain Scopus journals abdominal pain PubMed journals abdominal pain medical journals abdominal pain free journals abdominal pain best journals abdominal pain top journals abdominal pain free medical journals abdominal pain famous journals abdominal pain Google Scholar indexed journals
Article Details
1. Introduction
Herlyn-Werner-Wunderlich (HWW) syndrome is a rare congenital anomaly involving Müllerian and Wolffian structures, anatomically characterized by a triad of uterus didelphys, obstructed hemivagina, and ipsilateral renal-ureteral agenesis, with the right side twice more frequently affected than the left [1, 2]. In the general population, the reported incidence of uterine didelphys with renal agenesis is 0.1% to 3.8%; out of these, two thirds have a complete vaginal septum [3]. New classification proposed by Zhu et al. includes two types. Type 1, with a completely obstructed hemivagina and type 2, with an incompletely obstructed hemivagina [4]. Clinically, HWW syndrome results in hematometrocolpos on the obstructed hemivagina side, which produces a mass effect with pain [5]. Patients usually present symptoms shortly after menarche. Delays can occur in case of incomplete hemivagina obstruction or partial blood absorption between menstruations [6, 7]. The diagnosis is often difficult due to syndrome infrequency and clinical presentation variability. Early detection is important because surgical resection of the obstructed vaginal septum can provide pain relief and prevent further complications [2]. Delayed diagnosis could affect the reproductive performance of these patients, because retrograde blood flow destroys tubal function and leads to endometriosis [8]. Radiologic imaging is a fundamental tool in HWW syndrome diagnosis. Ultrasound is the first step when a Müllerian anomaly is suspected, but the technique is not able to clearly identify this anatomical abnormality. MRI depicts structural abnormalities with high-level accuracy and results are necessary to precisely plan surgery [7]. Surgical treatment consists in vaginal septum excision, showing good results. Around 80% of patients are able to conceive after surgery. Renal abnormalities and endometriosis are often associated with HWW syndrome. Therefore, it is important that physicians pay attention to these two indicator conditions, to guarantee a timely diagnosis and to avoid complications [8]. We present an HWW syndrome case, type 1.1 according to Zhu classification 4, with unusual late symptom onset. The minimally invasive surgical drainage procedure was supported by intraoperative ultrasound guidance carried out by an experienced ultrasonographer who helped the surgeon through a real-time visual ultrasonographic feedback to minimize surgical risks and to preserve fertility. The goal of this report is to review the published literature on HWW syndrome diagnosis, treatment and discuss the potential future role of laparoscopic ultrasound guidance to improve fertility-sparing surgery in female genital anomalies.
2. Case Report
A twenty-year-old woman was admitted to our department with 1-month history of lower abdominal pain, not responsive to medical treatment. No associated menstrual irregularity, urinary or bowel symptoms, or loss of appetite/weight was evident, and menarche started at the age of twelve. No significant family and personal medical history were referred. No external genitalia abnormalities were noted, and secondary sexual characteristics were well developed. Physical examination exposed a tender and mobile mass in the pelvic region up to the umbilicus level. Gynecologic examination revealed a bulge occupying the upper part of the vaginal canal. Laboratory exams revealed normal white blood cells count and negative serum beta HCG. The CA 125 serum level was elevated (155 UI/mL; normal range= 0-34 U/mL). Abdominal and pelvic ultrasonography revealed a 197x83x120 mm regular neoformation, tender to the push of the ultrasound probe, with a “jelly like” content and absent flow at Doppler examination. The mass seemed to be connected to the uterine body, which appeared dislocated in the right hypochondrium (Figure 1). Only the right ovary was identified. The right kidney was not visualized. The left kidney was normal with a distal ureteral dilation (mm 49x20).
Magnetic resonance imaging (MRI) of the pelvis revealed uterus didelphys with two separated vaginas. The right vagina was inferiorly obstructed and distended, with blood as hematocolpos, suggesting a longitudinal obstructing vaginal septum. Both ovaries were described as normal. The right kidney was not visualized. Herlyn-Werner-Wunderlich syndrome was hypothesized in consideration of the right renal agenesis, uterus didelphys, and unilateral obstructed hemivagina with resultant hematocolpos. The patient was scheduled for combined laparoscopic and hysteroscopic treatment under laparoscopic ultrasound guidance. Prior to the surgery the patient underwent a gynecologic examination under anesthesia confirming the bulge on the right anterolateral vagina wall and confirmed the cervix in the left portion. Laparoscopy was performed in lithotomic position, after a 10-mm trocar insertion in the umbilicus. Two 5-mm ancillary trocars were introduced in the lower abdomen. Continuous CO2 pneumoperitoneum was induced keeping an intra-abdominal pressure below 12 mmHg. A 0° optic was introduced in the umbilical 10-mm trocar. Diagnostic laparoscopy revealed normal ovaries and fallopian tubes, but two uterine bodies as uterus didelphys, dislocated in the mesogastric and hypochondriac region and the presence of 100 mm mass, tender to the touch by laparoscopic forceps (Figure 2). Moreover, peritoneal brown patches were present suggesting early peritoneal endometriosis due to retrograde menstruation. An intraoperative ultrasound exam was required to clarify the origin of the formation. A 10 mm-suprapubic trocar was positioned to enter with a laparoscopic probe (model Toshiba PET-805LA, Toshiba Aplio i800 ultrasound machine), covered with a sterile cover. The probe was inserted in the 10 mm suprapubic trocar and positioned in direct contact with the uterus (Figure 3). The laparoscopic ultrasound guidance revealed an obstructive longitudinal vaginal septum with a massive hematocolpus in the right blind hemivagina and allowed surgeon to incise the septum using a transvaginal approach, spilling out a large amount of chocolate-like fluid (900 cc) (Figure 4). The septum was resected revealing a second cervix (Figure 5).
Hysteroscopy was performed with a vaginoscopic approach, using a 5-mm diameter continuous-flow hysteroscope with oval profile, a 30° fore-oblique telescope and a 5 Fr operating channel (Office Continuous Flow Operative Hysteroscopy ‘size 5’; Karl Storz, Tuttlingen, Germany). Saline solution (NaCl 0.9%) was used as distension medium, which was introduced with an electronic irrigation and aspiration system (Endomat; Karl Storz, Tuttlingen, Germany). A stable intrauterine pressure of about 40 mmHg was obtained. The hysteroscopic view showed a left external uterine ostium with a regular cervix. A left hemicavity with a single fallopian tube ostium was visualized examining the left cervical canal. On the right side, after the incision of the septum, a right external uterine ostium with a regular cervix was found. This right cervical canal led to a right hemicavity with a single fallopian tube ostium. The procedure took 30 minutes. No significant bleeding nor postoperative complications were encountered. Our case is classified as U3bC2V2 congenital anomaly according to the ESHRE/ESGE classification established by the CONUTA working group [9]. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
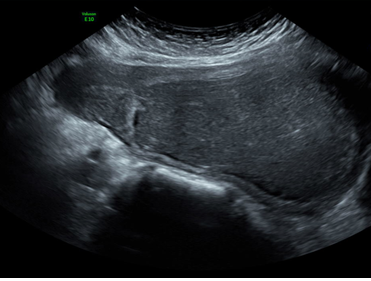
Figure 1: Ultrasound image of the hematocolpos.
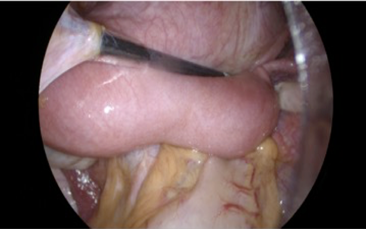
Figure 2: Laparoscopic view of two two uterine hemicorpi and hematocolpos.

Figure 3: Laparoscopic probe in contact with the uterus.
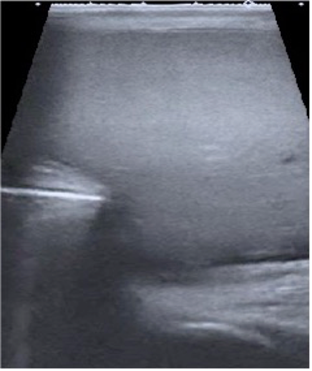
Figure 4: Laparoscopic ultrasound guidance during hematocolpos incision.
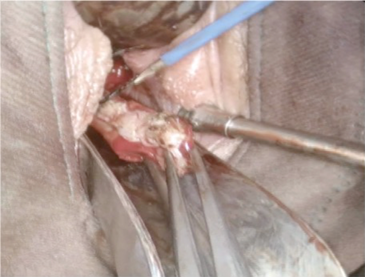
Figure 5: Vaginal septum resection.
3. Methods
A systematic review was therefore undertaken following
the Preferred Reporting Items for Systematic reviews and Meta-Analyses “PRISMA” guidelines [10]. The clinical question was developed based on the PICOS format for this review (Table 1) [10]. Studies with patients with HWW syndrome were considered for the inclusion. Case reports were included in the selection. We searched PubMed (all from inception to 20 February 2019) to identify previous HWW syndrome case reports and reviews. No language restrictions were initially applied. We made an advanced search using in “all fields” the following key words: “Herlyn-Werner-Wunderlich”, “didelphys uterus, obstructed hemivagina, ipsilateral renal agenesis” and “congenital vaginal oblique septum syndrome”. This process was performed collaboratively by 2 authors (AM, MMC).
4. Results
The electronic database search provided 186 results. 159 records were screened after 27 duplicates were removed and of which 15 were excluded for linguistic reasons and 17 were excluded because full text was not available. 127 full text articles were screened and of which 20 were excluded because of ante menarche age of patients, 14 because related to pregnancy, 3 because presenting with cervical carcinoma, 20 because considered not relevant for the review, 9 because patients did not have all HWWS characteristics. 61 articles were considered eligible and of which reference lists were analyzed finding 2 additional eligible studies. Overall, 63 articles were incorporated in our review and patient features are summarized in Table 2. The main bias of the review is that many studies include few patients or single case report.
|
Definition |
Search Keywords |
|
|
Participants |
Patients with HWW syndrome. Patient with cancer, ante menarchal and pregnant were excluded. |
“Herlyn-Werner-Wunderlich”, “didelphys uterus, obstructed hemivagina, ipsilateral renal agenesis” and “congenital vaginal oblique septum syndrome” |
|
Intervention |
Any intervention |
Not set |
|
Comparison |
Any intervention |
Not set |
|
Outcome |
To assess the accuracy of the diagnosis and to identify the best treatment approach to avoid complications and improve the fertility outcome |
Not set |
|
Study Design |
Any type of study including case report |
Not set |
Table 1: PICOS Format and Search Keywords.
Table 2: Sistematic literature review about cases of HWW syndrome.
5. Discussion
5.1 Definition
Herlyn?Werner-Wunderlich syndrome represents currently a combination of two different syndromes: Herlyn-Werner syndrome, described in 1971, consisting of renal agenesis and ipsilateral blind hemivagina, and Wunderlich syndrome, described in 1976 that broadened the syndrome adding uterus didelphys [1, 7]. The first article in English using the term Herlyn-Werner-Wunderlich syndrome described the triad of uterine didelphys with obstructed hemivagina and ipsilateral renal agenesis and was published in 2006. The acronym OHVIRA (obstructed hemivagina and ipsilateral renal anomaly) syndrome was proposed in 2007 to allow the inclusion of other uterine and renal anomalies [4].
5.2 Etiopathogenesis
HWW syndrome occurs at the eighth week of gestation due to an embryogenesis defect affecting both the paramesonephric (Müllerian) and mesonephric (Wolffian) ducts [11]. The close embryological relationship between the Müllerian and Wolffian ducts results in a strong association between renal and genital tract abnormalities. Indeed, renal agenesis is a predictor for ipsilateral obstructive Müllerian anomaly in more than 50% of cases [12, 13]. During the 6ed week of embryogenesis, the absence of Müllerian Inhibiting Factors promotes in female embryos bidirectional growth of paired Müllerian ducts [14]. At the 8th week, the Müllerian ducts migrate to the midline where they fuse to develop the uterus, the cervix, and the upper part of the vagina [6]. The lower third of vagina is formed from sinovaginal bulbs, which are protrusions of the urogenital sinus [15]. Wolffian ducts induce kidneys development and play an important role in the internal genital organ development, as adequate fusion inductor of the Müllerian ducts [2]. Failure of fusion leads to uterine duplication with two uterine bodies, two cervices, and a vaginal septum [16]. The absence of one Wolffian duct leads to kidney and ureteral agenesis on the absent side, and to lateral displacement of the Müllerian duct, which cannot fuse with the contralateral duct, resulting in uterus didelphys. The contralateral Müllerian duct induces vagina development, whereas the displaced duct cannot come into contact with the urogenital sinus and centrally forms a blind sac, leading to an imperforate hemivagina
5.3 Classification
Zhu et al. [4] reviewed the characteristics of 79 HWW patients at the Peking Union Medical College Hospital and suggested a new syndrome classification based on complete or incomplete obstructed vaginal septum presence. Each of these two groups included two classification types. Type 1.1: The affected hemivagina is completely obstructed and hematocolpos usually occur a few months after menarche, alongside abdominal pain, fever, and vomiting. Type 1.2: The hemivagina is completely obstructed, the cervix behind the septum is maldeveloped/atresic and menses cannot outflow from the uterus behind the septum through the atresic cervix. Type 2.1: A small connection exists between the two hemivaginas, which obstructs the vaginal cavity behind the septum incompletely. Type 2.2: The hemivagina is completely obstructed and a small connection exists between the duplicated cervices. In the two last classifications, menses can outflow through a small connection, therefore patient symptom onset occurs later in life [4]. We classified our case according to Zhu et al. [4] as a 1.1 type, since a completely obstructed hemivagina was evident and in absence of cervical atresia or communication between the two cervices. However, the late symptom onset (seven years after menarche) makes our case unusual.
5.4 Clinical presentation
Herlyn-Werner-Wunderlich syndrome is usually diagnosed at puberty, shortly after menarche, compared to most frequent congenital anomalies of the female genital tract, such as imperforate hymen or vaginal atresia, presenting symptomatic amenorrhea, Initially, the syndrome may remain unrecognised as regular menstrual flow, from the unobstructed hemivagina appears as normal menses. Additionally, dysmenorrhea, if present, is a common complaint in this age group [1, 3, 11]. Clinical symptoms may vary and non-specific features such as acute abdominal, pelvic or vaginal pain, dysuria, urinary retention, vaginal discharge and infertility have been reported. Associated complications include infectious collections and long-term sequelae such as endometriosis, pelvic adhesions, and infertility [11]. In case of infected hematocolpos, fever, chills, nausea and vomiting may be present [8]. In extremely rare cases, hematocolpos can lead to hematosalpinx and rupture, resulting in peritonitis, while incomplete obstruction could cause mild intermittent symptoms that do not get worse until complete obstruction with hematocolpos occurring later in life [6]. Rarely, adenocarcinoma of the obstructed uterine cervix and clear cell carcinoma of the obstructed vagina portion are also reported [3]. Clinical symptoms are mainly related to the abnormality type. In classification I, the common clinical presentation can be pelvic pain shortly after menarche, associated with vaginal or pelvic mass. In classification 2, the clinical presentation may be delayed as the obstructed side can be drained through the contralateral vagina [17]. Fedele et al. conducted a large institutional case series including 87 patients with OHVIRA syndrome, of which 67 patients were diagnosed with didelphys uterus, obstructed hemivagina and ipsilateral renal agenesis. Clinical characteristics, in particular main symptoms, were underlined like dysmenorrhea (94%), spotting (41%), chronic pelvic pain (24%), vaginal discharge (14%), dyspareunia (14%), fever (3%) and acute abdomen pain (2%) [18].
5.5 Diagnosis
Sonography and magnetic resonance imaging (MRI) are extremely useful to diagnose and classify Müllerian duct anomalies [4]. Ultrasound is frequently the initial imaging modality due to its wide availability and relatively low cost [19]. Recently Gai et al. investigated ultrasound features of 21 patients affected with HWW and compared them with surgery results. All 21 HWW syndrome cases were diagnosed with ultrasonography prior to surgery. Based on these results, he suggested that a sonographic type 1 HWW syndrome diagnosis might be possible in evidence of a double uterus, with or without uterine cavity hemorrhage, featuring an echo?free area below one cervix, with dot?like hyperechoic regions, mimicking endometriotic ovarian cysts and ipsilateral renal agenesis. Type 2 HWW syndrome ultrasonographic features are the same as for type 1, apart from a smaller and lower mass tension, due to partial menstrual blood drainage [20]. In a retrospective analysis, including 70 patients with hemivaginal septum, uterus didelphys and ipsilateral renal agenesis, a high ultrasonography accuracy rate to diagnose HWW syndrome was reported. Only 37 out of 70 patients required MRI or further confirmation of uterine and cervical development [21]. Ultrasound achieved 90-92% accuracy to diagnose HWW syndrome. However, vaginal septum visualization is often difficult and requires an MRI. This modality has long been considered as the gold standard to diagnose and plan surgical treatment, especially in a tertiary center with experience in Müllerian anomaly interpretation [18, 15, 22]. MRI with multiplanar image provides more detailed information regarding uterine morphology (uterine horns disposition), vaginal channels continuity (obstructed/not obstructed) [22], vaginal septum thickness and location, obstructed cavity contents (e.g. blood versus simple fluid) and coexisting urinary tract malformations [11, 19].
MRI accuracy, to diagnose uterine malformations, is well established and even 100% accuracy has been reported [23]. Laparoscopy has been advocated as the gold standard for HWW syndrome evaluation and associated complication treatment, specifically for those cases where a clear MRI diagnosis is impossible, an MRI is not available or when suspected concurrent intraperitoneal pathologies such as endometriosis, adhesions and pelvic infection are present [3, 11]. Intraoperative ultrasound guidance can be very helpful in HWW syndrome surgery in order to gain access to the obstructed hemivagina, especially when the vaginal bulges are not obvious, avoiding bladder, rectum and blood vessels damage [24]. We performed full time intraoperative ultrasound guidance using a laparoscopic probe, to identify first the origin of the pelvic mass, then to guide the surgeon to drain the hematocolpus and finally to identify the two different hemicavities during the hysteroscopic procedure. We could not identify any HWW case reports in which the use of a laparoscopic ultrasound probe was described. We identified three case reports describing intraoperatively ultrasound guidance. Khong et al described a transabdominal ultrasound guidance of vaginal septum resection [25]; Gungor Ugurlucan et al. [26] and Schutt et al. [27] described a transvaginal ultrasound guidance, Alur et al described an intraoperatively ultrasound guidance but without reference to the approach they used [24].
5.6 Treatment
HWW syndrome treatment aims at complication prevention to avoid hematocolpos and hematometra in order to restore genital system functionality, achieving normal fertility potential [1, 3]. Currently, the preferred surgical approach for patients with 1.1, 2.1, and 2.2 classification is the full excision and marsupialization of the vaginal septum applying a transvaginal approach in order to reestablish the continuity of the obstructed hemivagina. This approach is better executed under ultrasound guidance and during menstruation as large distended hematocolpos are easier to visualize and to palpate [1]. Although not yet reported in literature, the grossly distorted uterovaginal anatomy could increase the risk of resecting normal vaginal tissue or even lead to bladder perforation, particularly when the obstructed vagina reaches the hymeneal ring. Intraoperative ultrasound guidance is very useful to identify anatomical structures to decrease this risk. Treatment for patients with 1.2 classification differs from the treatment of patients with other classifications because surgical cervical agenesis correction is difficult and laparoscopic or transabdominal resection of the atresic hemi-uterus is suggested [4]. Complete vaginal septum excision was performed in all 16 HWW syndrome patients described by Kapczuk et al. The surgery was for 15 patients uneventful. Vaginal septum excision was complicated by urinary bladder injury in one patient, with spontaneous perforation of the vaginal septum a week before hospital admission [28]. Hur et al. suggested not omitting laparoscopic evaluation in patients with obstructed vaginal septum, which may inevitably result in massive menstrual regurgitation or even endometriosis and pelvic adhesions, which cannot be detected by ultrasonography or MRI [29]. Postoperative vaginal adenosis should be considered in patients with previously obstructed vagina. No definitive guidelines are yet existing, although some authors recommend yearly Papanicolaou tests and colposcopy [1].
5.7 Prognosis
Untreated HWW syndrome can lead to endometriosis, pelvic adhesions, and pyosalpinx or pyocolpos [1]. Endometriosis occurs in 17%–35% of patients with uterus didelphys. The rate of endometriosis was higher among patients with complete hemivaginal obstruction compared to those with incomplete obstruction, possibly because of consistent and severe retrograde menstrual flow [21]. Women with uterus didelphys have a reasonable chance of getting pregnant, but the abortion rate is high (74%) and premature delivery is common (22%). In 82% of pregnancies a caesarean section is required [13]. Zhu et al. performed a retrospective long-term follow-up study on surgical prognosis and pregnancy outcomes. They found that full resection of the vaginal septum was associated with good outcomes and fertility. No pathologic pregnancies or pregnancy complications were documented [4]. Gholoum et al. performed a review including 12 HWWS patients who were treated surgically with vaginal septectomy and hematocolpos/hematometrocolpos drainage. The median follow-up was 3 years in which 11 patients were asymptomatic after treatment and only one patient complained irregular menses [1]. MRI evaluation of the genital tract is recommended in all young women with known renal abnormalities, to carry out surgical corrections of the obstruction before menarche and therefore before any damage has occurred [13]. In conclusion, HWW syndrome prognosis is good for early diagnosed and treated patients, except for those with 1.2 classification. Ipsilateral hysterectomy is suggested in HWW syndrome cases complicated by cervical atresia, because septum resection would not relieve obstructions [4].
6. Conclusions
Although rare, HWW syndrome should be considered in young patients presenting symptoms like dysmenorrhea, abdominal pain, pelvic mass and renal agenesis because early detection and management is important for symptom relieve, to prevent complications and to preserve future fertility. The current study is the first literature review on HWW syndrome; moreover, we present the first case in which the use of laparoscopic ultrasound probe is fundamental to diagnose and treat a uterine defect. Only few cases are described using transvaginal and transabdominal probes during surgery [24, 25, 26, 30]. We think that our technique allows a precise intraoperative definition of some complex uterine malformations, supporting a precise and safe surgical procedure and avoiding intraoperative complications; albeit just one case, we propose intraoperative laparoscopic ultrasound guidance as an innovative approach to be used in complex female genital malformations, waiting at least larger case series to have solid results about surgical outcomes and fertility.
Acknowledgments
No acknowledgments to declare.
Disclosure
No disclosures to declare.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Gholoum S, Puligandla PS, Hui T, et al. Management and outcome of patients with combined vaginal septum, bifid uterus, and ipsilateral renal agenesis (Herlyn-Werner-Wunderlich syndrome). J Pediatr Surg 41 (2006): 987-992.
- Khaladkar SM, Kamal V, Kamal A, et al. The Herlyn-Werner-Wunderlich Syndrome. A case report with radiological review. Pol J Radiol 81 (2016): 395-400.
- Gupta N, Gandhi D, Goyal P, et al. A variant of Herlyn-Werner-Wunderlich syndrome presenting with acute abdomen: a case report and review?of literature. Global Pediatric Health 5 (2018): 1-5.
- Zhu L, Chen N, Tong J L, et al. New classification of Herlyn-Werner-Wunderlich syndrome. Chin Med J (Engl) 128 (2015): 222-225.
- Karaca L, Pirimoglu B, Bayraktutan U, et al. Herlyn-Werner-Wunderlich syndrome: a very rare urogenital anomaly in a teenage girl. The Journal of Emergency Medicine.; 48 (2015): e73-e75.
- Beer WM, Carstairs SD. Herlyn Werner Wunderlich syndrome: an unusual presentation of acute vaginal pain. J Emerg Med 45 (2013): 541-543.
- Van Der Byl G, Di Giacomo V, Miele V. Herlyn Werner Wunderlich syndrome (HWWS): an unusual presentation of acute abdominal pain. J Ultrasound 17 (2014): 171-174.
- Piccinini PS, Doski J. Herlyn-Werner-Wunderlich syndrome: a case report. Rev Bras Ginecol Obstet 37 (2015): 192-196.
- Grigoris F Grimbizis, Stephan Gordts, Attilio Di Spiezio Sardo, et al. The ESHRE–ESGE consensus on the classification of female genital tract congenital anomalies. Gynecol Surg 10 (2013): 199-212.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8 (2010): 336-341.
- Mishra N, Ng S. Sonographic diagnosis of Obstructed Hemivagina and Ipsilateral Renal Anomaly Syndrome: a report of two cases. Australas J Ultrasound Med 17 (2014): 153-158.
- Sabdia S, Sutton B, Kimble RMN. The obstructed hemivagina, ipsilateral renal anomaly, and uterine didelphys triad and the subsequent manifestation of cervical aplasia. J Pediatr Adolesc Gynecol 27 (2014): 375-378.
- Aveiro A C, Miranda V, Cabral A J, et al. Herlyn-Werner-Wunderlich syndrome: a rare cause of pelvic pain in adolescent girls. BMJ case reports (2011): bcr0420114147.
- Mehra S, Chamaria K, Garga U, et al. Imaging diagnosis of Herlyn-Werner-Wunderlich syndrome. An extremely rare urogenital anomaly. Journal Of Clinical And Diagnostic Research 9 (2015): Td06-Td08.
- Yilmaz S, Yildiz AE, Fitoz S. Herlyn-Werner-Wunderlich syndrome: sonographic and magnetic resonance (MR) imaging findings of this rare urogenital anomaly. Pol J Radiol 82 (2017): 216-219.
- Wang J, Zhu L, Lang J, et al. Clinical characteristics and treatment of Herlyn–Werner– Wunderlich syndrome. Arch Gynecol Obstet 290 (2014): 947-950.
- Hamidi H, Haidary N. Late presentation, MR imaging features and surgical treatment of Herlyn-Werner-Wunderlich syndrome (classification 2.2); a case report. BMC Women's Health; 18 (2018): 161.
- Fedele L, Motta F, Frontino G, et al. Double uterus with obstructed hemivagina and ipsilateral renal agenesis: pelvic anatomic variants in 87 cases. Human Reproduction 28 (2013): 1580-1583.
- Al Ghafri A, Fida A, Al-Gharras A. Obstructed Hemivagina and Ipsilateral Renal Anomaly (OHVIRA) Syndrome. Oman Medical Journal 33 (2018): 69-71.
- Gai YH, Fan HL, Yan Y, et al. Ultrasonic evaluation of congenital vaginal oblique septum syndrome: a study of 21 cases. Experimental and Therapeutic Medicine 16 (2018): 2066-2070.
- Tong J, Zhu L, Lang J. Clinical characteristics of 70 patients with Herlyn–Werner–Wunderlich syndrome. International Journal of Gynecology and Obstetrics 121 (2013): 173-175.
- Widyakusuma LS, Lisnawati Y, Pudyastuti S, et al. A rare case of pelvic pain caused by Herlyn-Werner-Wunderlich Syndrome in an adult: A case report. International Journal of Surgery Case Reports 49 (2018): 106-109.
- Orazi C, Lucchetti MC, Schingo PMS, et al. Herlyn-Werner-Wunderlich syndrome: uterus didelphys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr Radiol 37 (2007): 657-665.
- Alur S, Nicandri K, Bhagavath B. Longitudinal vaginal septa with associated uterine anomalies: a case series. Female Pelvic Medicine & Reconstructive 21 (2015): e23-e26.
- Khong TL, Siddiqui J, Mallinson P, et al. Herlyn-Werner-Wunderlich Syndrome: Uterus Didelphys, Obstructed Hemivagina, and Ipsilateral Renal Agenesis–Role of Sonographically Guided Minimally Invasive Vaginal Surgery. Eur J Pediatr Surg 22 (2012): 171-173.
- Ugurlucan FG, Bastu E, Gulsen G, et al. OHVIRA syndrome presenting with acute abdomen: a case report and review of the literature. Clinical Imaging 38 (2014): 357-359.
- Schutt AK, Barrett MR, Trotta BM, Stovall DW. Perioperative evaluation in Herlyn-Werner-Wunderlich syndrome. Obstet Gynecol 120 (2012): 948-951.
- Kapczuk K, Friebe Z, Iwaniec K, et al. Obstructive Mullerian Anomalies in Menstruating Adolescent Girls: A Report of 22 Cases. J Pediatr Adolesc Gynecol 31 (2018): 252-257.
- Hur JY, Shin JH, Lee JK, et al. Septate uterus with double cervices, unilaterally obstructed vaginal septum, and ipsilateral renal agenesis: a rare combination of Müllerian and Wolffian anomalies complicated by severe endometriosis in an adolescent. J Minim Invasive Gynecol 14 (2007): 128-131.
- Pereira N, Anderson SH, Verrecchio ES, et al. Hemivaginal septum resection in a patient with a rare variant of Herlyn-Werner-Wunderlich syndrome. J Minim Invasive Gynecol 21 (2014): 1113-1117.
- Zurawin RK, Dietrich JE, Heard MJ, et al. Didelphic uterus and obstructed hemivagina with?renal agenesis: case report and review of the literature. J Pediatr Adolesc Gynecol 17 (2004): 137-141.
- Smith NA, Laufer MR. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertility and Sterility 87 (2007): 918-922.
- Kim TE, Lee GH, Choi YM, et al. Hysteroscopic resection of the vaginal septum in uterus didelphys with obstructed hemivagina: a case report. J Korean Med Sci 22 (2007): 766-769.
- Asha B, Manila K. An unusual presentation of uterus didelphys with obstructed hemivagina with ipsilateral renal agenesis. Fertil Steril 90 (2008): 849.e9-849.e10.
- Kimble RM, Khoo SK, Baartz D, et al. The obstructed hemivagina, ipsilateral renal anomaly, uterus didelphys triad. Aust N Z J Obstet Gynaecol 49 (2009): 554-557.
- Sarac A, Demir MK. Herlyn-Werner-Wunderlich syndrome: a rare cause of infertility. Eur Radiol 19 (2009): 1306-1308.
- Jindal G, Kachhawa S, Meena GL, et al. Uterus didelphys with unilateral obstructed hemivagina with hematometrocolpos and hematosalpinx with ipsilateral renal agenesis. J Hum Reprod Sci 2 (2009): 87-89.
- Takagi H, Matsunami K, Imai A. Uterovaginal duplication with blind hemivagina and ipsilateral renal agenesis: review of unusual presentation. J Obstet Gynaecol 30 (2010): 350-353.
- Ar?kan I, Harma M, Harma M, et al. Herlyn-Werner-Wunderlich syndrome (uterus didelphys, blind hemivagina and ipsilateral renal agenesis): a case report. J Turk Ger Gynecol Assoc 11 (2010): 107-109.
- Nigam A, Raghunandan C, Yadav R, et al. OHVIRA syndrome: rare cause of chronic vaginal discharge in an unmarried female. Congenit Anom (Kyoto) 51 (2011): 153-155.
- Dhar H, Razek YA, Hamdi I. Uterus didelphys with obstructed right hemivagina, ipsilateral renal agenesis and right pyocolpos: a case report. Oman Med J 26 (2011): 447-450.
- Cox D, Ching BH. Herlyn-Werner-Wunderlich syndrome: a rare presentation with pyocolpos. J Radiol Case Rep 6 (2012): 9-15.
- Guducu N, Gonenc ? G, Isci H, et al. Herlyn-Werner-Wunderlich Syndrome Timely Diagnosis is Important to Preserve Fertility. J Pediatr Adolesc Gynecol 25 (2012): 111-112.
- Mandava A, Prabhakar RR, Smitha S. OHVIRA Syndrome (obstructed hemivagina and ipsilateral renal anomaly) with uterus didelphys, an unusual presentation. J Pediatr Adolesc Gynecol 25 (2012): e23-e25.
- Del Vescovo R, Battisti S, Di Paola V, et al. Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging 12 (2012): 4.
- Bajaj SK, Misra R, Thukral BB, et al. OHVIRA: Uterus didelphys, blind hemivagina and ipsilateral renal agenesis: advantage MRI. J Hum Reprod Sci 5 (2012): 67-70.
- Moshiri M, Seyal AR, Cruite I, et al. Herlyn-Werner-Wunderlich syndrome with a partially obstructed hemivagina. Radiol Case Rep 7 (2015): 800.
- Zhou Y, Fu X, Qian H, et al. A Herlyn-Werner-Wunderlich syndrome variant with ipsilateral renal absence and a contralateral duplex collecting system in a 26-year-old female. Gynecol Obstet Invest 77 (2014): 137-140.
- Ahmad Z, Goyal A, Das CJ, et al. Herlyn-Werner-Wunderlich syndrome presenting with infertility: Role of MRI in diagnosis. Indian J Radiol Imaging 23 (2013): 243-246.
- Nabeshima H, Nishimoto M, Shiga N, et al. Laparoscopic Strassman metroplasty in a postmenarcheal adolescent girl with Herlyn-Werner-Wunderlich müllerian anomaly variant, obstructed noncommunicating didelphic uterus without gartner duct pseudocyst. J Minim Invasive Gynecol 20 (2013): 255-258.
- Attar R, Y?ld?r?m G, Inan Y, et al. Uterus didelphys with an obstructed unilateral vagina and ipsilateral renal agenesis: A rare cause of dysmenorrhoea. J Turk Ger Gynecol Assoc 14 (2013): 242-245.
- Lin TB, Hsieh MF, Han SC, et al. Obstructed hemivagina and ipsilateral renal anomaly with uterus didelphys and vaginal discharge. Taiwan J Obstet Gynecol 52 (2013): 593-596.
- Wozniakowska E, Torres A, Milart P, et al. Delayed diagnosis of Herlyn-Werner-Wunderlich syndrome due to microperforation and pyocolpos in obstructed vaginal canal. J Pediatr Adolesc Gynecol 27 (2014): e79-e81.
- Yavuz A, Bora A, Kurdoglu M, et al. Herlyn-Werner-Wunderlich syndrome: merits of sonographic and magnetic resonance imaging for accurate diagnosis and patient management in 13 cases. J Pediatr Adolesc Gynecol 28 (2015): 47e52.
- Kumar S, Rajagopal K V, Karegowda L H, et al. Herlyn-Werner-Wunderlich syndrome: a rare cause of acute urinary retention in an adolescent girl. BMJ case reports (2015): bcr2015209638.
- Tug N, Sargin MA, Çelik A, et al. Treatment of Virgin OHVIRA Syndrome with Haematometrocolpos by Complete Incision of Vaginal Septum without Hymenotomy. J Clin Diagn Res 9 (2015): QD15-QD16.
- Mittal R. Herlyn-Werner-Wunderlich Syndrome. The Journal of Obstetrics and Gynecology of India 66 (2016): 128-130.
- Sharma R, Dey AK, Mittal K, et al. Use of imaging in diagnosis of Herlyn-Werner-Wunderlich syndrome, a case report. J Obstet Gynaecol 36 (2016): 873-875.
- Bhoil R, Ahluwalia A, Chauhan N. Herlyn Werner Wunderlich Syndrome with Hematocolpos: An Unusual Case Report of Full Diagnostic Approach and Treatment. Int J Fertil Steril 10 (2016): 136-140.
- Unal E, Tanyildiz HG, Sonmezer M, et al. Herlyn-Werner-Wunderlich syndrome: a rare cause of pelvic pain and high CA 19-9 levels in an adolescent girl. APSP J Case Rep 7 (2016): 4.
- Tsai JL, Tsai SF. Case Report: A Rare Cause of Complicated Urinary Tract Infection in a Woman with Herlyn-Werner-Wunderlich Syndrome. Iran Red Crescent Med J 18 (2016): e40267.
- Ellspermann R, Sirhari C, Chapin E, et al. Point-of-care ultrasound aiding in the diagnosis of Herlyn-Werner-Wunderlich syndrome. Clin Pract Cases Emerg Med 1 (2017): 370-373.
- Sleiman Z, Zreik T, Bitar R, et al. Uncommon presentations of an uncommon entity: OHVIRA syndrome with hematosalpinx and pyocolpos. Facts Views Vis Obgyn 9 (2017): 167-170.
- Jung EJ, Cho MH, Kim DH, et al. Herlyn-Werner-Wunderlich syndrome: An unusual presentation with pyocolpos. Obstet Gynecol Sci 60 (2017): 374-377.
- Ilyas M, Khan I, Saldanha CL. Herlyn-Werner-Wunderlich syndrome a rare genitourinary anomaly in females: a series of four cases. Pol J Radiol 83 (2018): e306-e310.
