Intimate Partner Violence among Pregnant Women and Associated Factors in Negelle Borena Town Guji Zone, South Oromia
Article Information
Kebebush Worku, Hunde Lami, Godana Arero
Comprehensive specialized hospital and medical college, Adama, Oromia, Ethiopia
*Corresponding author: Hunde Lami, Comprehensive specialized hospital and medical college, Adama, Oromia, Ethiopia.
Received: 18 July 2022; Accepted: 26 July 2022; Published: 25 August 2022
Citation: Worku K, Lami H, Arero G. Intimate Partner Violence among Pregnant Women and Associated Factors in Negelle Borena Town Guji Zone, South Oromia. Fortune Journal of Health Sciences 5 (2022): 488-498
Share at FacebookAbstract
Background: Intimate partner violence is an important public health and human rights issue. Intimate partner violence during pregnancy has been found to be associated with fatal and non-fatal adverse health outcomes for the pregnant woman and her baby. The aim of this study is to determine the magnitude of intimate partner violence among pregnant mothers and associated factors.
Objective: To assess Intimate partner violence among pregnant women and associated factors in Negelle Borena town in the selected public health facility 2020.
Methods: Facility based cross-sectional study was carried out from Oct15 –Dec15/2020. Face to face interviews were conducted using a pre-tested structured questionnaire. The collected data was entered into Epi info version 7.2.1.0 and then exported into Statical package for social science version 20 for analysis. Descriptive statistics were conducted. Bivariate analysis was done to select candidate variable for multivariate analysis. Finally, variables which had significant associations with intimate violence during pregnancy were identified on the basis of p-value<0.05 and AOR with 95% CI.
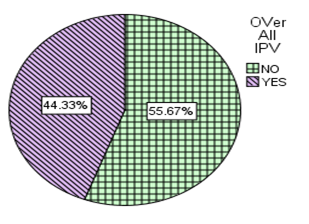
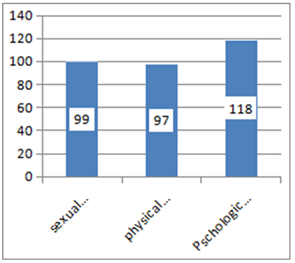
Result: About 44.3% (95% CI 44.2-44.4) of pregnant women had faced at least one form of intimate partner violence during the current pregnancy. Psychological violence 29.1%, Sexual violence 24.4%, physical violence 23.9% were forms of violence the respondents was encountered. Respondents who were primary educated (AOR 2.99, 95%CI 1.23-7.25), secondary educated (AOR 2.36,95%CI 1.047-5.34),respondents in age group of 26-34years (AOR 0.20 95%CI 0.065-0.64) and age group of >=35years (AOR 0.26, 95%CI 0.09-0.77),responandants with history of miscarriage, abortion and/ still birth (AOR 0.5 ,95%CI 0.32-0.78),respondents who accepted their partner had right to beat them(AOR 1.83 , 95% CI 1.82-2.82),respondents whose partners were in age group of 4
Keywords
intimate partner, Violence, pregnancy, Negelle Borena, oromia, 2020
intimate partner articles, Violence articles, pregnancy articles, Negelle Borena articles, oromia articles, 2020 articles.
Article Details
1. Introduction
According to the world health organization (WHO) intimate partner violence (IPV) is defined as “any behaviour within an intimate relationship that causes physical, psychological or sexual harm to those in the relationship” .Intimate partner is current or former partner, whom the woman has been married, cohabited or dated. The terms “wife abuse”, “domestic violence” and “violence against women,” are interchangeably used to refer the extent of sexually, psychologically, and physically coercive acts used against adult and adolescent women by current or former male intimate partners. Violence against women may occur at any stage of women lives, including during pregnancy [1-4].
Violence against women is largely recognized as a major human right abuse, and a significant public health problem with multiple adverse physical, mental, sexual, and reproductive health effects. Intimate partner violence can occur prior to pregnancy, during pregnancy and in the postpartum period. Because of the changes in the emotional, physical, social and economic needs of women during pregnancy, conception may be a time of unique vulnerability for women to become victims of IPV. Intimate partner violence during pregnancy is increasingly being recognized as an important risk factor for adverse health outcomes for both mother and newborn(4-6).
The risk factors for IPV during pregnancy is usually not different from that of IPV in general, the only difference is that pregnancy is a time that may need increased relationship commitment and increase the resources needed. Some risk factors are likely to be more important during pregnancy one potential risk factor significantly associated with intimate partner violence during pregnancy is having an unwanted or unplanned pregnancy (4, 6) . Globally, one third of women who have been in a relationship have experienced physical and/or sexual violence by their intimate partner in their life time and the prevalence is highest in African, Eastern Mediniterranean and South-East Asia regions where approximately 37% of ever-partnered women reported having experienced physical and/or sexual intimate partner violence at some point in their lives. Whereas the prevalence of intimate partner violence during violence varies between1% to 28% worldwide (7-9).The magnitude of intimate partner violence during pregnancy in Africa range between 2% to 57%.The magnitudes of intimate partner violence during pregnancy in Ethiopia is estimated to be 4%-59% (10-13). Intimate partner violence is an important public health and human rights issue. Pregnant mothers are not immuned against intimate partner violence. Violence at any time in a woman’s life can result in an innumerable devastating health problem however; violence during pregnancy is of special concern for a number of reasons. First, violence during pregnancy poses health risks not only for the woman but also for her fetus. Second evidence to suggest that violence occurring during pregnancy may be more severe in its nature, or more frequent in its occurrence, than violence occurring at other times, at least for some women(6, 4).
Violence against women has immense health problem that sap her energy, compromise mental and physical health reduce her self –esteems .Intimate partner violence as sub set of domestic violence during pregnancy has been discovered to be related with many negative health outcomes both for the victim women and growing fetus(4). The consequence of IPV during pregnancy can be fatal and Non- fatal both for the mother and new born baby. Fatal consequences like homicide and suicide.(4,14, 15).Study showed that pregnant women who face IPV will have more likely hood of acquiring post natal depression and the likely hood of acquiring PND increase by 2- 3 times and women who encounter IPV more likely to have under five mortality (16-19).Effect of IPV on reproductive health includes Low birth weight, Pre-term labour/delivery, insufficient weight gain, Obstetric complications, STIs/HIV, Miscarriage, Unsafe abortion. (17, 20-22). Intimate partner violence during pregnancy (IPVDP) is also associated with negative health behaviour, like heavy use of alcohol, illicit drugs and poor utilization of maternity health service. IPVDP will increase the likely hood of using of alcohol and illicit drug 2 times. Women who reported physical IPV in their relationship were less likely to use ≥4 ANC, be tested for HIV and less likely to delivery by skilled attendant and deliver in a health facility (23-25).
The risk factors for IPV are not single there are many interrelated factors. The most widely used model for understanding violence is the ecological model(26). Which proposes that violence is a result of factors operating at four levels: individual, relationship, community and societal. Individual factor like partner’s drinking alcohol, age of partners, educational level, unintended pregnancy; History of Experience of violence in the family Origin, polygamy, norm related to gender equality, social support and occupation are most commonly claimed as risk factor for IPVDP in existining literature. For example evidence show that women whose partner is drink alcohol frequently will increase the risk of IPVDP by 5 times. At the level of the family and relationship, the male controls wealth and decision making within the family and marital conflict is frequent. At the community level, women are isolated with reduced mobility and lack of social support. Male peer groups condone and legitimize men’s violence. At the societal level, gender roles are rigidly defined and enforced and the concept of masculinity is linked to toughness, male honor, or dominance. The prevailing culture tolerates physical punishment of women and children, accepts violence as a means to settle interpersonal disputes, and perpetuates the notion that men “own” women (27-30). Reducing maternal & child mortality is a top priority so any effort to reduce maternal mortality & to achieve the sustainability development goals should focus on addressing IPVDP. Evidence show that Reducing IPV by 50% could potentially reduce unintended pregnancy by 2%–18% and abortion by 4.5%–40% (1).As we see the burden is high & the consequence of IPVDP many .In the presence of this fact previous study on intimate partner were focused mainly on non-pregnant women, due to this there is lack of publish research in the area of intimate partner violence during pregnancy in Ethiopia as whole and specifically in the study area. So the aim of this study is to determine the magnitude of intimate partner violence among pregnant mothers attending antenatal care in Negelle Borena town public health facility and identify associated factors.
2. Materials and Methods
2.1 Study Design and Period
Institutional based cross-sectional study was carried out from Oct 15 – Dec 15/2020.
2.2 Study Area and Setting
The study was conducted at Nagele Borena general hospitals and health center in Negelle Borena town Guji zone; Oromia, south Ethiopia. Negelle Borena is located in the southern part Ethiopia in oromia region, 610km away from the capital city of the country. In Nagele Borena there are two public health facility that serve the community ; one general Hospital and health center .Negelle Borena hospital and health center officially commenced their functioning in 1938 and 2010 respectively .The catchment population of Negelle Borena hospital and health center were estimated to be 1,112,435 and 56,777 respectively. From this the proportion of pregnant mother is 3.47% (expected pregnancy 38601 and 1970 for hospital and health center respectively.
2.3 Source and Study Population
All pregnant women who visited Negelle Borena hospital and health center for antenatal care (ANC) were the source population.
Sampled pregnant mothers who got ANC in Negelle Borena Hospital and health center and full fill the selection criteria was the study population.
2.3.1 Study Unit
A pregnant woman who was randomly selected and who gives consent was the study unit.
Inclusion Criteria
Mothers who were pregnant and Visit health center for ANC service only was included in the study.
Exclusion Criteria
Those women come for first time during data collection was excluded because of their list was not available to fix sampling frame.
2. 4 Sample Size and Sampling Procedures
2.4.1 Sample Size Determination
Sample size was calculated by using single population proportion formula.
n= (Zα/2)2 p (1-p)
d2
With assumption of desired precision (d) = 0.05, Prevalence of IPV is assumed to be 0 .59 this from Study conducted in oromia Bale zone(12) .Z α\2 at 95% confidence interval = 1.96 Based on the assumption, the calculated sample size (n) = 372 & by considering 10 % for non-response rate would became =37 the actual sample size would be became =409.
2.4.2 Sampling Procedure
The number of sample size for each health facility was determined by proportion to population size by reviewing the previous annual ANC service report of the two facilities. So six month ANC service achievement of Negelle Borena Hospital and health center of the year 2011/2019 were 1980 and 891 respectively. The sampling interval (K) for each health facilities was determined by dividing the number of average expected ANC during the study period by the sample size for each health facilities. Thus, for hospital K=4 and for health center K= 2. Study participants were selected by using systematic sampling. The first mother was selected by lottery method. Then every kth mother was selected and interviewed till the Sample size fulfilled. Sampling frame was fixed based on antennal registration list. In case the women in the list absent the next consecutive women was interviewed.
2.5 Variables of the Study
2.5.1 Dependant Variable
Intimate partner violence during current pregnancy
4.4.2. Independent Variables
Demographic FactorAge, educational status, Residence, Monthly income, occupation, Factor related to husband Alcohol/chat/tobacco use, aggressive behavior, Women related factor Women income contribution, family History of violence experience Family factors Type of marriage, head of house hold, house hold monthly income, decision making power, Nuber of children. Reproductive Factors Parity, miscarriage, abortion, still birth, intent of pregnancy.
2.6 Operational Definitions
In this study intimate partner was considered as current spouse, co-habited (live in the same house without formal marriage), Current non-marital partners (boyfriends), former partner or spouse.
Intimate partner violence was defined as if the respondent said “Yes” to any one of the ranges of sexually, psychologically, and physically or any combination of the three coercive acts used against adult and adolescent women during current pregnancy, regardless of the legal status of the relationship with current/former intimate partner(7). Physical violence was defined as if the study participants say “Yes” to one or more intentional acts of physical force or aggression such as pushing, slapping, throwing, hair pulling, punching, kicking, or burning, use of a weapon, perpetrated with the potential to cause harm, injury, disability or death towards pregnant women (7).
Psychological/emotional violence was defined as if the study participant said “Yes” to one or more acts or threats of acts, such as shouting, controlling, intimidating, humiliating, and threatening the victim(7).
Sexual violence was defined as if the study subject said “Yes” to any one of the uses of force, coercion, or psychological intimidation to force the woman to engage in a sex act against her will whether or not it is completed Sexual violence was presumed to have taken place when a woman was physically forced to have sexual Intercourse against one’s will, or having sexual intercourse because of being afraid of what a partner might do, or being forced to do something sexual one has found degrading or humiliating (7).
2. 7 Data Collection Procedures (Instruments, Personnel, Measurements)
Validated instrument, based on the standard of WHO multicounty study on women’s health and domestic violence against women was used to collect data from each of the Study participants. This questionnaire had four items for psychological violence, six items for physical violence, and three additional items for sexual violence(8). The standardized questionnaire was first prepared in English and then translated to Afan Oromo (local language) and back to English to maintain consistency of the tool by language expert. Two female midwives for data collection and one experienced Bsc nurse for supervision were recruited. A face-to-face interviewer-administered questionnaire was used to collect data from all pregnant women who consented to be part of the study.
Data collectors and the supervisor were trained for one day on techniques of data collection and on supervision. The principal investigator and supervisor was made a day to day on-site supervision during the whole period of data collection as WHO standard of researching violence against women(2) .And data was checked in each questionnaire daily for completeness and consistency. The questionnaire was pre-tested to check the response, language clarity and appropriateness of the questionnaire, while the pretest was done outside study area with 5% of sample Size on 20 women. Based on the finding from the pre-test, modification on the questionnaire was done, and arrangement of questions was revised.
2.9 Data Processing and Analysis
Data was first checked manually for completeness, Coded then entered into Epi-Info version 7.2.1.0 and exported to SPSS version 20 for further analysis. Exploratory data analysis was done to check missing values and outliers. Descriptive statistics was conducted to summarize the data. Then results would be presented in text, tables, graphs and charts. Bivariate analysis was done to select candidate variables for multivariate analysis. Variables which had p values up to 0.25 were considered for the multivariable logistic regression analysis to control the effects of confounding variables. Collinearity test was carried out to see the correlation between independent variables using the standard error. A Hosmer– Lemeshow and Omnibus tests were conducted to test model goodness of fit. Finally, variables which had significant associations with intimate partner violence during pregnancy were identified on the basis of AOR with 95% CI and p-value of 0.05.
The Institutional Review Board (IRB) of Adama Hospital Medical College was approved the research for scientific and ethical integrity. Letter of permission was obtained from Negelle district administration and health offices. Before conducting the interviews, information was given to the participants and participants were assured of voluntary participation, confidentiality, anonymity and freedom to withdraw from the study at any time. The nature and importance of the study was explained and written consent was obtained from the participants. The interview with the pregnant women was conducted privately in the separate room. In case interview may trigger emotional response appropriate counselling and where to go for help was told. The WHO ethical and safety recommendation protocol for research on domestic violence against women was followed as guide (2).
3. Result
3.1 Socio-Demographic Characteristics tnd Socio-Economic Factors of the Respondent
A total of 406 pregnant women participated in the study, making the response rate of 99.3%.The socio-demographic character of women and obstetrics associated factors are described in table 2.The median age of the respondents were 25years with 6 interquartile range /6 IQR in range of 16-38. Majority (48.8%) and (60.8%) of the respondents were Muslim religion follower and Oromo ethnicity. More than nine in every ten (93.6%) they were married. Regardless of their occupation more than two in every five (44.1%) of them were house wife followed by 18% of them were merchant. Vast majority (40.9%) of them were primary educated and about less than one in three (28.3%) of them were illiterate. About three in every four (74.9%) of them were urban dweller look table2 below.
Table 1: Socio-demography characteristics and socio-economic factors of pregnant women in Negelle Borena town selected public health facility 2020(n=406)
|
Variable |
Frequency |
Percent |
|
|
Age |
16-25 |
216 |
53.2 |
|
26-35 |
165 |
40.6 |
|
|
>35 |
25 |
6.2 |
|
|
Religion |
Orthodox |
124 |
30.5 |
|
Muslim |
198 |
48.8 |
|
|
protestant |
70 |
17.2 |
|
|
Othera |
14 |
3.4 |
|
|
Ethnicity |
Oromo |
247 |
60.8 |
|
Amhara |
45 |
11.1 |
|
|
Tigre |
18 |
4.4 |
|
|
Somali |
43.6 |
10.6 |
|
|
Otherb |
53 |
13.1 |
|
|
Current marital status |
Divorced |
12 |
3 |
|
Have regular partner but living apart |
11 |
2.7 |
|
|
married |
380 |
93.6 |
|
|
widow |
3 |
0.7 |
|
|
Occupation |
Gov`t employee |
39 |
9.6 |
|
Merchant |
73 |
18 |
|
|
House wife |
179 |
44.1 |
|
|
self employed |
51 |
12.6 |
|
|
private |
18 |
4.4 |
|
|
Daily Laborer |
30 |
7.4 |
|
|
Otherc |
16 |
3.9 |
|
|
educational status |
Illiterate |
115 |
28.3 |
|
Primary(1-8) |
166 |
40.9 |
|
|
Secondary(9-12) |
81 |
20 |
|
|
Tertiary( Diploma and above) |
44 |
10.8 |
|
|
Residence |
urban |
304 |
74.9 |
|
Rural |
102 |
25.1 |
|
|
Income categories(n=327) |
≤200-2500 |
66 |
16.3 |
|
>=2500 |
261 |
64.3 |
|
3.2 Reproductive and Women Related Characteristics
Half (50%) of the respondents contributed income more or less. Nearly two in every three (56.7%) of them witnessed their father battered their mother. More than one in every three (40.9%), (61.3%) of them accept wife beating if there is justifiable reasons and didn’t want the current pregnancy respectively. Similarly more than one in every three (35.2%) of them had history of abortion, miscarriage or still birth. Concerning their parity nearly four in every three (73.4%) of the respondents had one to four (1-=4) children on range. More than two third (70.7%) of the respondents were in third trimester. See table 2 below.
Table 2: Reproductive and women related Factors of IPVDP in Negelle Borena town selected public health facility 2020(n=406)
|
Variable |
Frequency |
persent |
|
|
Witnessed maternal abuse during childhood |
yes |
230 |
56.7 |
|
no |
176 |
43.3 |
|
|
Acceptance of violence |
yes |
166 |
40.9 |
|
no |
240 |
59.1 |
|
|
Want current pregnancy |
yes |
157 |
38.7 |
|
no |
249 |
61.3 |
|
|
Mischarge ,Abortion, Still birth |
yes |
143 |
35.2 |
|
no |
263 |
64.8 |
|
|
Number of children (Para |
No children |
100 |
24.6 |
|
1-=4 |
298 |
73.4 |
|
|
>=5 |
8 |
2 |
|
|
Month of pregnancy |
5-6 mon |
119 |
29.3 |
|
7-9 mon |
287 |
70.7 |
|
|
Contribution of income |
yes |
203 |
50 |
|
no |
203 |
50 |
|
3.3 Socio-Demography Characteristics ,Socio-Economic and Behavioral Factors of Respondent’s Partners
According to respondents report the median age of their partners were 31years with interquartile range of 8 years. Majority(28.8%) of the respondent’s partner were merchant. More than one third (36.2%) of them were primary educated. More than half (52.2%) of the partner’s income was in>= 2500ETB categories. Concerning respondent’s partner behavioral factors; more than half (52.7%), more than half (53.7%) and 18 % of them drunk alcohol, chew khat and smoke cigrate respectively. More than one in every three (39.9 %) of the partner had history of violence with other men.
3.4 Prevalence of Intimate Partner Violence among Pregnant Women
More than two in every five 180(44.3% 95% CI 44.2-44.4) of pregnant women had faced at least one form of intimate partner violence during the current pregnancy.
3.5 Forms of Intimate Partner Violence among Pregnant Women
From the three form of violence emotional /psychological violence was the leading 118(29.1%); from this emotional violence majority (28.1%) of the victim was insulted or made to feel bad about herself followed and some (8.9%) of them were belittled or humiliated in front of other people.
Sexual violence was the second common 99(24.4%) form of intimate partner violence during the current pregnancy. From this majority (23.2%) of them had sexual intercourse without their interest because of fair of partner .About 6.9%, 6.4% of them were forced to had sexual intercourse without their interest and to did something sexual that found her degrading or humiliating by their partner respectively during the current pregnancy. Less than one in every three 97(23.9) of the respondents were victim of atleast on form physical violence during their current pregnancy. Majority (19.2%) of them were slapped by their partner. About 2.2% of them were chocked or burned.
3.6 The Overlap of Different Form of Ipv
There were overlap of the different forms of intimate partner violence among respondents. About five percent (5.6%) of them were victim of all the three form of violence (physical, sexual and psychological violence. Around ten percent (10.3%) of them were physical and sexual, thirteen (13.8%) of them were physical and psychological, the remaining fourteen percent (14.2%) them were sexual and psychological violence respectively violence victim respectively.
3.7 Factors Associated with Ivp among Pregnant Women
Bivariate logistic regression was used to identify factors associated with IPV. Accordingly many Sociodemographic variables of the respondents and their partners, Respondents partners’ behavioral factor, respondent’s reproductive and pregnancy related factors, respondents associated factors and family associated factors were assessed for the presence or absence of association with IPV. From variables entered in Bivariate fifteen were identified as candidate for multivariate, based on the criteria specified in method part.
At multivariate from fifteen candidates seven of them were identified as significantly associated with IPV. From those seven factors half of them were allied to respondents and her partner Sociodemographic factors look below table5.Respondent’s educational status were one of the factor significantly associated with IPV. Respondent who were primary educated were three times (AOR 2.99, 95%CI 1.23-7.25), secondary educated more than two times(AOR 2.36,95%CI 1.047-5.34) more likely encountered IPV during current pregnancy respectively compared to illiterate( uneducated) pregnant women. Age of respondents were also significantly associated and those respondents in age group of 26-34years were about 80% times (AOR 0.20 95%CI 0.065-0.64) and age group of >=35years about 70% time (AOR 0.26, 95%CI 0.09-0.77) less likely encountered IPV during current pregnancy compared to age group of 16-25years.Respondants were also asked about their reproductive and women related factors; responandants with history of miscarriage, abortion and or still birth were 50% times less likely to report IPV compared to respondents without history of miscarriage ,abortion and or stillbirth(AOR 0.5 ,95%CI 0.32-0.78). Accepting or justifying as husband had right to beat his wife is also significantly associated with IPV. And respondents who accepted their partner had right to beat them were about two times more likely to faced IPV compared to those didn’t accepted(AOR 1.83 , 95% CI 1.82-2.82).
Respondents were asked about their partners’ socio-demographic characteristics and behavioral factors. Respondents whose partners were in age group of 40-49 years were encountered IPV about two times(AOR 2.22,95%CI 1.10-4.47) compared to respondents’ whose partner were in age group of 20-29yers.Concerning education status; respondent’s whose Partners were tertiary (diploma and above) educated 62% times (AOR 0.38, 95%CI 0.20-0.71) less likely violent to the respondents compared to illiterate respondent’s partners. Partners’ behavior like fighting with other men or aggressive behaviors were significantly associated with IPV. Respondents whose partners had history of fighting with other men were encountered IPV about two times (AOR 1.77 95%CI 1.14- 2.75) more likely compared to respondents whose partner had not fighting.
Table 3: Bivariete and Multivariate analysis results of intimate partner violence associated factors in Negelle Borena selected public health facility 2020
|
Variable |
IPVDP |
COR(95%CI) |
AOR(95%CI) |
||
|
NO |
YES |
||||
|
Respondents educational status |
Illiterate |
56 |
59 |
1 |
|
|
Primary(1-8) |
91 |
75 |
2.26(1.086 - 4.69)* |
2.99(1.23-7.25)* |
|
|
Secondary(9-12) |
49 |
32 |
1.76 t(0.87 - 3.57 |
2.37(1.05-5.34)* |
|
|
Tertiary |
30 |
14 |
1.39(0.645 - 3.03) |
2.01(0.84- 4.82) |
|
|
Educational status of respondent’s partner |
Illiterate |
23 |
21 |
1 |
|
|
Primary(1-8) |
76 |
71 |
0.87(0.42 - 1.80) |
0.49(0.19-1.21) |
|
|
secondary(9-12) |
84 |
43 |
0.89(0.52 – 1.54) |
0.61(0.33-1.13) |
|
|
Tertiary |
43 |
45 |
0.48(0.28 – 0.85)* |
0.38(0.20 – 0.71)* |
|
|
Respondent’s partner history of violence with other men |
no |
122 |
122 |
1 |
|
|
yes |
104 |
58 |
1.79(1.19-2.69)* |
1.77(1.14-2.75)* |
|
|
Acceptance of violence |
no |
118 |
122 |
1 |
|
|
yes |
108 |
58 |
1.93 ( 1.28-2.89 )* |
1.83(1.82-2.82)* |
|
|
Miscarriage ,Abortion, Still birth |
no |
163 |
100 |
1 |
|
|
yes |
63 |
80 |
0.48(0.32-0.73)* |
0.50(0.32-0.78)* |
|
|
Age catagory |
16-25 |
131 |
85 |
1 |
|
|
26-35 |
88 |
77 |
0.25(0.01 – 0.63)* |
0.20(0.065 – 0.63)* |
|
|
>35 |
7 |
18 |
0.34(0.13 – 0.85)* |
0.26(0.08 – 0.64)* |
|
|
Partner age Group |
20-29 |
86 |
51 |
1 |
|
|
30-39 |
102 |
99 |
0.75(0.41-2.75) |
1.78(0.78 – 4.07) |
|
|
40-49 |
38 |
30 |
1.22(0.7-2.13) |
2.22(1.10 – 4.47)* |
|
Key COR - Crude odds Ratio, AOR - Adjusted Odds Ratio, CI: confidence interval.* P- Value<0.05
1=reference
4. Discussion
In this cross-sectional study the prevalence of intimate partner violence among pregnant women were 44.3% (95% CI 44.2-44.4). This finding is in agreement with findings from Portugal (43.4)(52),systematic review of Africa(2%-57%)(13) and also finding in our country such as in Abay chamone(44.5%)(34) ,Debre Markos(41.1%)(11) and Tigre region (40.8%)(43).It is higher than study in Vietnam(37%)(18) ,Rwanda(10.2%)(45) and Uganda (27.8%)(51), in Ethiopia in south east part of the counters (25.8%)(22) , Tigray region (20.6%)(21) and ofla district in Tigray region (37.%)(54) .This higher variation could be as a result of sample size difference. For example in Uganda the total smple size was 180.This could be result in lower prevalence. Other possible cause of such discrepancy could be using only physical intimate partner violence for example in Tigray region only physical intimate partner aspect were used but in our case physical, sexual and psychological aspect were assessed this could result in higher prevalence. Such a higher prevalence could be due to the impact of covid-19. Due to covid-19 Schools closed, and many workers were furloughed, laid off, or told to work from home. With personal movement limited and people confined to their homes, advocates expressed concern about a potential increase in intimate partner violence. Stay-at-home orders, intended to protect the public and prevent widespread infection, left many IPV victims trapped with their abusers(55). The high prevalence of IPV may lead to poor pregnancy outcome and maternal Psychological and physical health problems. However this finding was lower than finding from Kenya putoko (66.9%)(30), finding from different part of Ethiopia; Gonder (58.7%)(29), Bale zone (59.0%)(12).The higher prevalence in finding from Bale zone (59%) could be due to using economical and controlling aspect in addition to in to the usual physical, sexual, psychological .In this study psychological violence was frequent; followed by sexual and physical intimate partner violence.
Nearly one in every three (29.1%) of the respondents were victim of psychological violence in the form of insult or made her to feel bad about herself. This finding is in line with finding from Namibia(38) but lower the finding from Gonder town(47) and Abay chamone(43). Physical violence was less frequent type of violence which accounts for about one in every (23.8%). The finding that psychological violence was the most prevalent abusive act in this study may be due to the fact that pregnancy could offer protection against physical violence for many women, and that the decrease in physical violence during the pregnancy period may parallel an increase in psychological violence, as evidenced by the patterns of longitudinal violence prevalence in relation to pregnancy onset in studies from Brazil(28) and Bangladesh(59) .Moreover, in this study, the use of the culturally sensitive WHO Violence Against women questionnaire is considered to increase detection of the emotionally abusive acts of insulting, intimidating and threatening, which might not be culturally considered as acts of violence in many traditional societies.
Respondent’s educational status were one of the factor that significantly associated with IPV.Respondents who were primary and secondary educated were about three and two times more likely encounter IPV during current pregnancy. This finding is consistent with finding from Brazil(28), study in Hind Mumbai(44), systematic review in Africa(13), Gonder(29). This due to those primary and secondary educated women were more complain / report violence than uneducated or illiterates are more tolerant of violence (57)
Respondents age were one of significantly associated with IPV during the current pregnancy. Respondents in age group of 26 – 35 years and age group of >=35years about 80% time were about 70% times less likely to encountered IPV during current pregnancy compared to age group of 16-25years.this in line with finding ever where (8) and in Ethiopia(12).This according to Fernandez idea who described as the age of woman increases she often grows in social status as she becomes not only a wife, but also a mother and a socially influential member of her community(58). Thus, older women are less likely to report current experience of IPV than younger.
In this study women acceptance or supporting as husband has right to beat his wife was significantly associated with IPV. Respondents who accept violence were about 2 times more likely to encounter IPV.This finding congruent with findings from WHO multi country study on women’s health and domestic violence, findings northern part of the country shire town(8), Ofla district in Tigray region(54).The possible justification for this unawareness of basic human rights and other legal rights of women. It is this state of ignorance that ensure their acceptance and consequently, the perpetuation of harmful traditional practices affecting their wellbeing or it can be due to poor and weak implementation of various women oriented laws is also a factor we need to take into Consideration as one of the cause of violence against women (61).
Respondents reproductive and pregnancy history were significantly associated with IPV during current pregnancy. Accordingly respondents with history of pregnancy loss /miscarriage, abortion or/and stillbirth /were 50% times less likely to encounter IPV during current pregnancy. This finding is inconsistence with other finding(12, 36).This could be due to different study showed that unwanted pregnancy is associated is more likely hood of IPV during pregnancy (12, 13, 47, 54).As this unwanted pregnancy is lost /miscarriage, abortion or /and stillbirth; this can result in less likely of IPV.But such type of association is more liable for reverse causality that whether pregnancy lose result into IPV or IPV lead to pregnancy loss. This beyond such across-section study and it need further study.
Respondent’s partner educational status was one of the factor that were significantly associated with IPV during current pregnancy; Respondent’s whose partner was higher educated/diploma and above 61% times less likely to encounter IPV.This finding is in agreement with finding of Else were(8, 38, 44) and finding in Ethiopia(43).possible justification is educated partner did had awareness about basic human and women right this and consequence it’s of violation or it can be due to understanding the consequence of violence during pregnancy both on the mother and unborn baby. Finding from Abay chamone in oromia region contradicted this (34) Respondent’s partner age is also significantly associated with IPV. Respondent’s whose partner was in age group of 40- 49years were more than two times more likely to encountered IPV Compared with their younger age groups. This finding is in line with (12, 59). The age discrepancy between women and their partners could be the possible reason for the increased odds of violence among oldest intimate partners. In our study, there was a big difference between the age of the pregnant women and their intimate partners. This study the mean age of the respondents was 25±4.6 and partners was 32±5 more than fifty percent of the respondents were in age group of 16-25 years. Finding in Nigeria showed that age difference of between 5-9years increase the likelihood encountering IPV by 1.35times(60). The age difference between the partners might affect communication and understanding that lead to violation.
Respondent’s partner history of violence with other men or aggressive behavior was also significantly associated with IPV during the current pregnancy. Respondent’s whose partner had history of violence with other men were 77% more likely to encounter IPV during current pregnancy. This congruent with find from elsewhere (8, 13, 39)and in Ethiopia (12). The possible explanation violence is learned behavior (61).
Recommendation
Creating the community awareness to change beliefs that are culturally embedded in collaboration with the indigenous leadership, community leader, and other key stakeholders is mandatory. Policy makers need to consider screening for IPV in the antenatal care service as one component. It is also better to include IPV screening as one component of community health extension package. Further studies that show the effect of intimate partner violence on the pregnancy outcome need to be conducted.
Conclusion
The prevalence of intimate violence intimate partner violence in the Negelle Borena town selected public health facility is among the highest compared to other area.More than two in every five(44.3%) women were experienced at least one act of IPV.Psychological and sexual violence were the most frequent type of IPV.Primary and secondary educated ,age group of 26-35years,acceptance of violence or women beating ,miscarriage ,abortion /or still birth were responants relate factors that were associated with IPV.Respondant’s partner tertiary educated,age of 40-49years,historyof violence with other men were partners associted factors with IPV.
References
- Organization WH. Understanding and addressing violence against women: Intimate partner violence. World Health Organization (2012).
- Ellsberg M aHL. Researching Violence Against Women: A Practical Guide for Researchers and Activists. Washington DC, United States:: World Health Organization PATH (2005).
- Bessa MMM, Drezett J, Rolim M, de Abreu LC. Violence against women during pregnancy: sistematized revision. Reprodução & Climatério 29 (2014): 71-9.
- Organization WH. Intimate partner violence during pregnancy: Information sheet. Geneva: World Health Organization (2011).
- Organization WH. WHO Global Consultation on Violence and Health. Violence: a public health. Geneva. document WHO/EHA/SPI. POA. 2) who. int … (1996).
- da Costa Marques DF. Intimate Partner Violence During Pregnancy (2012).
- Organization WH. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence: World Health Organization (2013).
- Claudia García-Moreno HAFMJME, Lori Heise,Charlotte Watts. WHO Multi-country Study on Women’s Health and Domestic Violence against Women (2005).
- Fletcher TR, Clements AD, Bailey B. Identifying intimate partner violence during pregnancy in prenatal care settings. International journal of health sciences education 3 (2016): 3.
- <Ethiopian Demographic and Health Survey 2016.pdf> (2016).
- Azene ZN, Yeshita HY, Mekonnen FA. Intimate partner violence and associated factors among pregnant women attending antenatal care service in Debre Markos town health facilities, Northwest Ethiopia. PloS one 14 (2019): e0218722.
- Lencha B, Ameya G, Baresa G, Minda Z, Ganfure G. Intimate partner violence and its associated factors among pregnant women in Bale Zone, Southeast Ethiopia: A cross-sectional study. PloS one 14 (2019): e0214962.
- Shamu S, Abrahams N, Temmerman M, Musekiwa A, Zarowsky C. A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PloS one 6 (2011): e17591.
- Alhusen JL, Ray E, Sharps P, Bullock L. Intimate partner violence during pregnancy: maternal and neonatal outcomes. Journal of women's health 24 (2015): 100-6.
- Organization WH. Global plan of action: health systems address violence against women and girls. World Health Organization (2016).
- Yu H, Jiang X, Bao W, Xu G, Yang R, Shen M. Association of intimate partner violence during pregnancy, prenatal depression, and adverse birth outcomes in Wuhan, China. BMC pregnancy and childbirth 18 (2018): 469.
- Adhikari R, Wagle A. Effect of intimate partner violence on pregnancy outcomes. Journal of Reproductive Health and Contraception 3 (2018): 17-26.
- Tho Nhi T, Hanh NTT, Hinh ND, Toan NV, Gammeltoft T, Rasch V, et al. Intimate partner violence among pregnant women and postpartum depression in Vietnam: a longitudinal study. BioMed research international (2019).
- Tsai AC, Tomlinson M, Comulada WS, Rotheram-Borus MJ. Intimate partner violence and depression symptom severity among South African women during pregnancy and postpartum: population-based prospective cohort study. PLoS medicine 13 (2016): e1001943.
- Sigalla GN, Mushi D, Meyrowitsch DW, Manongi R, Rogathi JJ, Gammeltoft T, et al. Intimate partner violence during pregnancy and its association with preterm birth and low birth weight in Tanzania: A prospective cohort study. PloS one 12 (2017).
- Berhanie E, Gebregziabher D, Berihu H, Gerezgiher A, Kidane G. Intimate partner violence during pregnancy and adverse birth outcomes: a case-control study. Reprod Health 16 (2019): 22.
- Demelash H, Nigatu D, Gashaw K. A Case-Control Study on Intimate Partner Violence during Pregnancy and Low Birth Weight, Southeast Ethiopia. Obstetrics and gynecology international (2015): 394875.
- Amaro H, Fried LE, Cabral H, Zuckerman B. Violence during pregnancy and substance use. American journal of public health 80 (1990): 575-9.
- Mohammed BH, Johnston JM, Harwell JI, Yi H, Tsang KW, Haidar JA. Intimate partner violence and utilization of maternal health care services in Addis Ababa, Ethiopia. BMC health services research 17 (2017): 178.
- Gashaw BT, Magnus JH, Schei B. Intimate partner violence and late entry into antenatal care in Ethiopia. Women and birth 32 (2019): e530-e7.
- Level ES. The Social-Ecological Model: A Framework for Violence Prevention. Health 1 (2002): 56.
- Audi CAF, Segall-Corrêa AM, Santiago SM, Andrade MdGG, Pèrez-Escamila R. Violence against pregnant women: prevalence and associated factors. Revista de saude publica 42 (2008): 877-85.
- Cripe SM, Sanchez SE, Perales MT, Lam N, Garcia P, Williams MA. Association of intimate partner physical and sexual violence with unintended pregnancy among pregnant women in Peru. International Journal of Gynecology & Obstetrics 100 (2008): 104-8.
- Fekadu E, Yigzaw G, Gelaye KA, Ayele TA, Minwuye T, Geneta T, et al. Prevalence of domestic violence and associated factors among pregnant women attending antenatal care service at University of Gondar Referral Hospital, Northwest Ethiopia. BMC Womens Health 18 (2018): 138.
- Owaka IO, Nyanchoka MK, Atieli HE. Intimate partner violence in pregnancy among antenatal attendees at health facilities in West Pokot county, Kenya. Pan African Medical Journal 18 (2017).
- Nguyen TH, Ngo TV, Nguyen VD, Nguyen HD, Nguyen HTT, Gammeltoft T, et al. Intimate partner violence during pregnancy in Vietnam: prevalence, risk factors and the role of social support. Global health action 11 (2018): 1638052.
- Women U. Progress of the World’s Women 2019–2020: Families in a Changing World. New York: United Nations Women (2019).
- Assembly UG. Declaration on the elimination of violence against women (1993).
- Abate BA, Wossen BA, Degfie TT. Determinants of intimate partner violence during pregnancy among married women in Abay Chomen district, Western Ethiopia: a community based cross sectional study. BMC women's health 16 (2016): 16.
- Pallitto CC, García-Moreno C, Jansen HA, Heise L, Ellsberg M, Watts C, et al. Intimate partner violence, abortion, and unintended pregnancy: Results from the WHO Multi-country Study on Women's Health and Domestic Violence. International Journal of Gynecology & Obstetrics 120 (2013): 3-9.
- Fujiwara T, Isumi A. Development of the intimate partner violence during pregnancy instrument (IPVPI). Frontiers in public health 7 (2019): 43.
- Johnson J, Haider F, Ellis K, Hay D, Lindow S. The prevalence of domestic violence in pregnant women. BJOG: An International Journal of Obstetrics & Gynaecology 110 (2003): 272-5.
- Bikinesi LT, Mash R, Joyner K. Prevalence of intimate partner violence and associated factors amongst women attending antenatal care at Outapi clinic, Namibia: A descriptive survey. African journal of primary health care & family medicine 9 (2017): 1-6.
- Ezeudu CC, Akpa O, Waziri NE, Oladimeji A, Adedire E, Saude I, et al. Prevalence and correlates of intimate partner violence, before and during pregnancy among attendees of maternal and child health services, Enugu, Nigeria: mixed method approach, January 2015. The Pan African Medical Journal 32 (2019).
- Shamu S, Shamu P, Machisa M. Factors associated with past year physical and sexual intimate partner violence against women in Zimbabwe: results from a national cluster-based cross-sectional survey. Global health action 11 (2018): 1625594.
- Coutinho E, Almeida F, Duarte J, Chaves C, Nelas P, Amaral O. Factors related to domestic violence in pregnant women. Procedia-Social and Behavioral Sciences 171 (2015): 1280-7.
- Abebe Abate B, Admassu Wossen B, Tilahun Degfie T. Determinants of intimate partner violence during pregnancy among married women in Abay Chomen district, Western Ethiopia: a community based cross sectional study. BMC Women's Health 16 (2016).
- Gebrezgi BH, Badi MB, Cherkose EA, Weldehaweria NB. Factors associated with intimate partner physical violence among women attending antenatal care in Shire Endaselassie town, Tigray, northern Ethiopia: a cross-sectional study, July 2015. Reproductive health 14 (2017): 76.
- Das S, Bapat U, More NS, Alcock G, Joshi W, Pantvaidya S, et al. Intimate partner violence against women during and after pregnancy: a cross-sectional study in Mumbai slums. BMC public health 13 (2013): 817.
- Rurangirwa AA, Mogren I, Ntaganira J, Krantz G. Intimate partner violence among pregnant women in Rwanda, its associated risk factors and relationship to ANC services attendance: a population-based study. BMJ open 7 (2017): e013155.
- Brownridge DA, Taillieu TL, Tyler KA, Tiwari A, Chan KL, Santos SC. Pregnancy and intimate partner violence: risk factors, severity, and health effects. Violence against women 17 (2011): 858-81.
- Bifftu BB, Dachew BA, Tadesse Tiruneh B, Zewoldie AZ. Domestic violence among pregnant mothers in Northwest Ethiopia: prevalence and associated factors. Advances in Public Health (2017).
- Deuba K, Mainali A, Alvesson HM, Karki DK. Experience of intimate partner violence among young pregnant women in urban slums of Kathmandu Valley, Nepal: a qualitative study. BMC Womens Health 16 (2016): 11.
- Ludermir AB, Araújo TVBd, Valongueiro SA, Muniz MLC, Silva EP. Previous experience of family violence and intimate partner violence in pregnancy. Revista de saude publica 51 (2017): 85.
- Barros ÉNd, Silva MA, Falbo Neto GH, Lucena SG, Ponzo L, Pimentel AP. Prevalence and factors associated with intimate partner violence among women in Recife/Pernambuco, Brazil. Ciencia & saude coletiva 21 (2016): 591-8.
- Clarke S, Richmond R, Black E, Fry H, Obol JH, Worth H. Intimate partner violence in pregnancy: a cross-sectional study from post-conflict northern Uganda. BMJ open 9 (2019).
- Coutinho E, Almeida F, Duarte J, Chaves C, Nelas P, Amaral O. Factors Related to Domestic Violence in Pregnant Women. Procedia - Social and Behavioral Sciences 171 (2015): 1280-7.
- Alebel A, Kibret GD, Wagnew F, Tesema C, Ferede A, Petrucka P, et al. Intimate partner violence and associated factors among pregnant women in Ethiopia: a systematic review and meta-analysis. Reprod Health 15 (2018): 196.
- Adhena G, Oljira L, Dessie Y, Hidru HD. Magnitude of Intimate Partner Violence and Associated Factors among Pregnant Women in Ethiopia. Advances in Public Health (2020).
- Evans ML, Lindauer M, Farrell ME. A pandemic within a pandemic—Intimate partner violence during Covid-19. New England journal of medicine 383 (2020): 2302-4.
- Ferdos J, Rahman MM. Maternal experience of intimate partner violence and low birth weight of children: A hospital-based study in Bangladesh. PloS one 12 (2017): e0187138.
- Weitzman A. Women’s Education and Intimate Partner Violence: Evidence from a Natural Experiment. Ann Arbor 1 (2001): 48106-1248.
- Fernandez M. Domestic violence by extended family members in India: Interplay of gender and generation. Journal of Interpersonal Violence 12 (1997): 433-55.
- Semahegn A, Mengistie B. Domestic violence against women and associated factors in Ethiopia; systematic review. Reprod Health 12 (2015): 78.
- Adebowale AS. Spousal age difference and associated predictors of intimate partner violence in Nigeria. BMC public health 18 (2018): 212.
- Nicholls TL. Family interventions in domestic violence: A handbook of gender-inclusive theory and treatment: Springer Publishing Company (2006).