In Order to Find Endometrial Disease in Peri- and Post-menopausal Hemorrhage, Hysteroscopy, Ultrasonography, and Histopathology Were Compared
Article Information
Jihad Al Hasan MD1,2, 3,4, Hassan Ajami,MD5, Kawsar Diab MD6, Kariman Ghazal MD 3,4,6,7
1 Head of Obstetrics and Gynecology Department, Al Zahraa Hospital University Medical Centre, Beirut, Lebanon
2 Head of Obstetrics and Gynecology Department, Lebanese University, Beirut, Lebanon
3 Assistant professor Obstetrics and Gynecology Department, Lebanese University, Beirut, Lebanon
4 Obstetrics and GynecologyDepartment, Rafik Hariri Hospital University Medical Center, Beirut, Lebanon
5 Reproductive Medicine Obstetrics and Gynecology Department, Al Zahraa Hospital University
Medical Centre, Beirut, Lebanon
6 Obstetrics and Gynecology Department, Al Zahraa Hospital University Medical Centre, Beirut, Lebanon
7 Obstetrics and Gynecology Department, Makassed Hospital University Medical Center, Beirut, Lebanon
*Corresponding Author: Kariman Ghazal, MD, Obstetrics and Gynaecology Department, Lebanese University.
Received: 31 January 2023; Accepted: 06 February 2023; Published: 14 February 2023
Citation: Kariman Ghazal, MD, Obstetrics and Gynaecology Department, Lebanese University.
Share at FacebookAbstract
Background:
Abnormal uterine bleeding is one of the most common presenting problems in a gynecologist's office or primary-care setting (AUB).
Methods:
Between December 2019 and December 2022, 264 peri and postmenopausal women participated in this study in a tertiary care hospital in Beirut, Lebanon
Results:
A total of 114 hysteroscopic operations and 264 ultrasonography exams were completed. Group A contained 149 patients, while Group B contained 113 individuals. 75% of the women in group A were postmenopausal, compared to perimenopausal women in group B
Conclusion:
Using histopathology as the gold standard, hysteroscopy showed to be extremely sensitive and specific. Although USG is less sensitive and specific than hysteroscopy, it still has good characteristics
Keywords
Abnormal uterine bleeding; Perimenopausal; Postmenopausal; Ultrasound; Hysteroscopy
Abnormal uterine bleeding articles Abnormal uterine bleeding Research articles Abnormal uterine bleeding review articles Abnormal uterine bleeding PubMed articles Abnormal uterine bleeding PubMed Central articles Abnormal uterine bleeding 2023 articles Abnormal uterine bleeding 2024 articles Abnormal uterine bleeding Scopus articles Abnormal uterine bleeding impact factor journals Abnormal uterine bleeding Scopus journals Abnormal uterine bleeding PubMed journals Abnormal uterine bleeding medical journals Abnormal uterine bleeding free journals Abnormal uterine bleeding best journals Abnormal uterine bleeding top journals Abnormal uterine bleeding free medical journals Abnormal uterine bleeding famous journals Abnormal uterine bleeding Google Scholar indexed journals Perimenopausal articles Perimenopausal Research articles Perimenopausal review articles Perimenopausal PubMed articles Perimenopausal PubMed Central articles Perimenopausal 2023 articles Perimenopausal 2024 articles Perimenopausal Scopus articles Perimenopausal impact factor journals Perimenopausal Scopus journals Perimenopausal PubMed journals Perimenopausal medical journals Perimenopausal free journals Perimenopausal best journals Perimenopausal top journals Perimenopausal free medical journals Perimenopausal famous journals Perimenopausal Google Scholar indexed journals Postmenopausal articles Postmenopausal Research articles Postmenopausal review articles Postmenopausal PubMed articles Postmenopausal PubMed Central articles Postmenopausal 2023 articles Postmenopausal 2024 articles Postmenopausal Scopus articles Postmenopausal impact factor journals Postmenopausal Scopus journals Postmenopausal PubMed journals Postmenopausal medical journals Postmenopausal free journals Postmenopausal best journals Postmenopausal top journals Postmenopausal free medical journals Postmenopausal famous journals Postmenopausal Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals Hysteroscopy articles Hysteroscopy Research articles Hysteroscopy review articles Hysteroscopy PubMed articles Hysteroscopy PubMed Central articles Hysteroscopy 2023 articles Hysteroscopy 2024 articles Hysteroscopy Scopus articles Hysteroscopy impact factor journals Hysteroscopy Scopus journals Hysteroscopy PubMed journals Hysteroscopy medical journals Hysteroscopy free journals Hysteroscopy best journals Hysteroscopy top journals Hysteroscopy free medical journals Hysteroscopy famous journals Hysteroscopy Google Scholar indexed journals gynecologist's articles gynecologist's Research articles gynecologist's review articles gynecologist's PubMed articles gynecologist's PubMed Central articles gynecologist's 2023 articles gynecologist's 2024 articles gynecologist's Scopus articles gynecologist's impact factor journals gynecologist's Scopus journals gynecologist's PubMed journals gynecologist's medical journals gynecologist's free journals gynecologist's best journals gynecologist's top journals gynecologist's free medical journals gynecologist's famous journals gynecologist's Google Scholar indexed journals Menstrual Disorders articles Menstrual Disorders Research articles Menstrual Disorders review articles Menstrual Disorders PubMed articles Menstrual Disorders PubMed Central articles Menstrual Disorders 2023 articles Menstrual Disorders 2024 articles Menstrual Disorders Scopus articles Menstrual Disorders impact factor journals Menstrual Disorders Scopus journals Menstrual Disorders PubMed journals Menstrual Disorders medical journals Menstrual Disorders free journals Menstrual Disorders best journals Menstrual Disorders top journals Menstrual Disorders free medical journals Menstrual Disorders famous journals Menstrual Disorders Google Scholar indexed journals postmenopausal bleeding articles postmenopausal bleeding Research articles postmenopausal bleeding review articles postmenopausal bleeding PubMed articles postmenopausal bleeding PubMed Central articles postmenopausal bleeding 2023 articles postmenopausal bleeding 2024 articles postmenopausal bleeding Scopus articles postmenopausal bleeding impact factor journals postmenopausal bleeding Scopus journals postmenopausal bleeding PubMed journals postmenopausal bleeding medical journals postmenopausal bleeding free journals postmenopausal bleeding best journals postmenopausal bleeding top journals postmenopausal bleeding free medical journals postmenopausal bleeding famous journals postmenopausal bleeding Google Scholar indexed journals endometrial tumor articles endometrial tumor Research articles endometrial tumor review articles endometrial tumor PubMed articles endometrial tumor PubMed Central articles endometrial tumor 2023 articles endometrial tumor 2024 articles endometrial tumor Scopus articles endometrial tumor impact factor journals endometrial tumor Scopus journals endometrial tumor PubMed journals endometrial tumor medical journals endometrial tumor free journals endometrial tumor best journals endometrial tumor top journals endometrial tumor free medical journals endometrial tumor famous journals endometrial tumor Google Scholar indexed journals Transvaginal sonography articles Transvaginal sonography Research articles Transvaginal sonography review articles Transvaginal sonography PubMed articles Transvaginal sonography PubMed Central articles Transvaginal sonography 2023 articles Transvaginal sonography 2024 articles Transvaginal sonography Scopus articles Transvaginal sonography impact factor journals Transvaginal sonography Scopus journals Transvaginal sonography PubMed journals Transvaginal sonography medical journals Transvaginal sonography free journals Transvaginal sonography best journals Transvaginal sonography top journals Transvaginal sonography free medical journals Transvaginal sonography famous journals Transvaginal sonography Google Scholar indexed journals
Article Details
INTRODUCTION
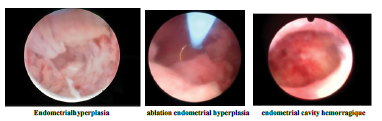
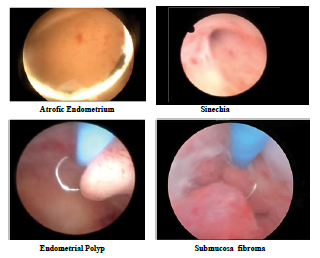
Abnormal uterine bleeding (AUB) is one of the most common presenting problems in a gynecologist's office or primary-care setting [1]. More than 70% of all gynecological consultations are for women who are peri- and postmenopausal [1]. Heavy menstrual bleeding (HMB, excessive menstrual blood loss), intermenstrual bleeding (IMB), and a combination of heavy and protracted menstrual bleeding are among the signs of AUB. The Menstrual Disorders Working Group of the International Federation of Gynecology and Obstetrics (FIGO) developed this language in 2011, and it is now being widely used [2]. Perimenopause is defined as occurring 2–8 years before menopause and 1 year after the last menstruation. The frequency of uterine disease and its related medical consequences rises in this age range, despite the fact that irregular bleeding patterns are a normal and expected aspect of perimenopause. After a year of menopause, abnormal uterine bleeding is referred to as postmenopausal bleeding (PMB). constitutes one of the most frequent causes for referral to gynecological services, mostly because of suspicion of a malignant endometrial tumor. [3]The challenge with uterine bleeding is that it has a large range of diagnostic possibilities, making it difficult to distinguish between normal and pathological patterns [2]. This is due to the wide range of normal fluctuation in monthly flow. The term PALM-COEIN, which stands for polyps, adenomyosis, leiomyoma, and malignancy, and COEIN, which stands for coagulopathies, ovulatory dysfunction, endometrial, iatrogenic, and not otherwise classified, can be used to diagnose AUB [4],[5]. The most effective methods for assessing AUB are a thorough history and physical examination [6]. A patient with AUB can be evaluated clinically in a number of phases. Transvaginal sonography (TVS) can be a useful tool in evaluating a woman who complains of abnormal vaginal bleeding by identifying anatomical abnormalities that are not visible on pelvic examination and by assessing the thickness, ovulatory status, and hormonal status of the endometrium [7]. TVS is an affordable, non-invasive, and practical approach to evaluating uterine pathology. [8]. One of the most popular methods to determine the causes of heavy uterine bleeding is dilatation and curettage (D&C). However, it is a blind method that, in fewer than 50% of instances, identifies the source of bleeding. In some situations, isolated lesions go undetected, necessitating repeated curettage or, if bleeding persists, a hysterectomy.During a D&C, problems include perforations, cervical rips and tears, the formation of scar tissue, and intrauterine adhesions are common [9]. A minimally invasive diagnostic and surgical procedure called hysteroscopy seeks to rule out or locate diseases that might require additional treatment [9]. In this surgical procedure, a gynecologist utilizes a small, illuminated telescopic equipment called a hysteroscope to obtain a panoramic view of the uterine canal and enable direct vision biopsies in order to identify and treat a variety of uterine problems, including irregular bleeding [10]. Endometrial hyperplasia, endometrial polyp, submucosal myoma, and endometrial atrophy can all be accurately detected [10].
METHODS AND MATERIALS
AUB continues to be a significant and occasionally unmet clinical need despite its relative prevalence. The goal of the current effort is to address the extensive, unjustified variance in reporting women's health outcomes [5] by standardizing assessment instruments for monitoring outcomes of AUB. To the best of our knowledge, this study is the first to explore diagnostic methods for abnormal uterine bleeding in a sample of Lebanese women. Thus, the study's objective was to assess the value of hysteroscopy and TVS in assessing irregular bleeding and in determining the provisional or final diagnosis. Additionally, it seeks to evaluate how well the results of hysteroscopy and ultrasound compare to those of histopathology.
Ethical approval:
The study protocol for all procedures was approved by the Institutional Review Board at the Lebanese University. Informed consent was obtained from the patients included in the study who fulfilled the inclusion and exclusion criteria, at the time of data collection in the last 3 years.
Study design and Participants:
This study was conducted between December 2019 and December 2022, in a tertiary care hospital in Beirut, Lebanon. Data was collected from 264 peri- and post-menopausal women who presented with abnormal uterine bleeding to private clinics and were transferred to the Department of obstetrics and gynecology at Zahraa University Hospital for evaluation. A detailed history of each patient was taken. Consecutive women aged between 35 and 90, admitted for dilatation and curettage and diagnostic operative hysteroscopy with history of abnormal menstrual bleeding were included in the study. Complaints of the women were categorized as heavy menstrual bleeding, intermenstrual bleeding, and frequent bleeding for last six months and not responding to conservative medications for postmenopausal bleeding. Women with normal or slightly bulky size uterus on bimanual examination and also by Pelvis Transvaginal Sonography (TVS) were only included. Excluded from this study werewomen beyond the age group mentioned above, with menstrual complaints such as oligomenorrhea and hypomenorrhea, having suspected pregnancy who responded to conservative medications, and not requiring hysteroscopy, were excluded from this study.All women where cervical or vaginal pathology was suspected were also excluded from the study. The eligible patients were subsequently divided into two groups, as shown in figure 1:
Group A and B underwent pelvis and vaginal ultrasound. Then, group A underwent dilatation and curettage, group B included patients who underwent hysteroscopy and the samples for 2 groups were sent to the histology laboratory Figure 1. If endometrial thickness (double layer) measured less than 15 mm in premenopausal womenafter menstrual cycle and less than 5 mm in postmenopausal women and seemed regular by TVS, it was considered a normal finding. A centrally placed echo dense line within the uterus and homogeneous endometrial lining with distinct margins to the myometrium were also considered normal. Deformations of the endometrial lining, absence of central hyperechoic line and the appearance of any structure with or without well-defined margins or variable echogenicity, were considered abnormal.
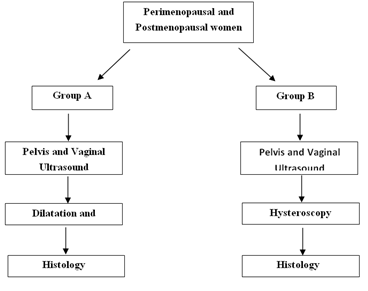
Figure 1: Figure showing the division of the patients into groups A and B
Hyperechogenic nodular lesions in the endometrial cavity were considered as polyps, while lesions with mixed echogenicity or hypoechoic lesions altering the contours of the endometrial cavity were considered as submucosal myomas. Findings were considered as suspected of malignancy in cases where the endometrial echo was irregular or with a variable echo texture. A Samsung real time ultrasound system R7 using a 3.5 Mhz convex probe was used to carry out the examination via the pelvic route for all patients with full bladder. An 8-10 Mhz probe was used to carry out the tests by transvaginal route with empty bladder. Virgin patients had pelvic ultrasound exclusively.
Operative investigations:
Dilatation curettage for group A patients:
Biopsy done from the endocervical canal before cervical dilatation, then cervical dilatation up to 7-8 Hegar. Endometrial polyp removal using ring forceps was carried out. A sharp curette was introduced and curettage starting first with the fundus then posterior wall then anterior wall then right then left lateral walls. The sample was placed in formalin 10 % for histopathological examinations by the pathologist.
Hysteroscopic examination for group B:
Under general anesthesia, the patient laid down in dorsal lithotomy position, per vaginal USG done to look for uterine size, consistency, mobility, and bilateral adnexa. Hysteroscopy was carried out by an operator who was blinded to the ultrasound findings. It was a rigid continuous flow panoramic hysteroscopy by 25 cm in length, 7 mm diameter of an outer sheath and 12°fiberoptic lens. The technique used to provide constant uterine distention was by attaching plastic bags of uro flow or sorbitol mannitol solution. Infusion pressure was elevated by pneumatic cuff under manometric control at a pressure of 100-130 mm HG . The procedure was monitored using a single chip video and the image was displayed on a monitor visible to the operator.. Once the telescope was introduced in the cavity, examination was done systematically: first the fundus, then anterior, then posterior then lateral walls of the uterus ending by visualization of the uterotubal junctions. The thickness, the color, the vasculature, and the consistency of the mucous membrane lining the uterine cavity was observed and recorded the aspect of the endocervical mucosa and the endometrium should be described. If there was any intrauterine pathology detected, the shape, the size, and the site was estimated. If submucosal fibroid or polyp was found, resectoscope was used to remove it. If endometrial hyperplasia was suspected, a groove was always done with the optic by passing it through the posterior uterine wall and the thickness was estimated.
Statistical analysis:
Statistical analysis was performed using the SPSS version 24. Sensitivity, specificity, positive and negative predictive values were calculated for TVS and hysteroscopy in diagnosing various uterine pathologies.
RESULTS
A total of 262 ultrasound examinations and 113 of hysteroscopic procedures were performed. There were 149 patients in Group A and 113 patients in group B. The mean age of women was 53 and 40 in group A and B respectively. The majority of women in group A were postmenopausal (75%) whereas group B women were perimenopausal Table 1. Postmenopausal bleeding was the main symptom of patients in group A (72%) whereas heavy menstrual bleeding (66%) was the main symptom in group B patients.
The duration of bleeding was less than 1 month in group A and more than 3 months but less than 6 months in group B. 44% of patients in group A had a normal ultrasound whereas 56% of patients showed thickness. Most of histological findings were endometrial polyps (52%), followed by proliferative endometrium (48%) and secretive endometrium (46%). Table 3 Ultrasounds, hysteroscopy andhistology findings findings for Group B Table 4. 25% normal ultrasounds were found 49% of thickness and 18% of polyps. Hysteroscopy findings confirmed the ultrasound findings in detecting normality and thickness. However, different percentages were found for polyps, fibroid, septum and
|
Variables |
Group A n=149 |
Group B n=113 |
|
Age (mean) |
53 |
40 |
|
BMI |
||
|
<35 |
11 (7%) |
95 (84%) |
|
>35 |
138 (93%) |
18 (16%) |
|
Parity |
||
|
Multipare |
140 (94%) |
86 (76%) |
|
Nullipare |
9 (6%) |
27 (24%) |
|
Period |
||
|
Perimenopausal |
37 (25%) |
98 (87%) |
|
Postmenopausal |
113 (75%) |
15 (13%) |
|
Abortion |
64 (44%) |
40 (26%) |
|
Medical conditions |
||
|
Hypertension |
88 (57%) |
10 (24%) |
|
Other |
62 (43%) |
94 (66%) |
Table 1: Characteristics of patients in Group A and Group B
|
Group B |
Group A |
Symptoms |
|
87 (66%) |
23 (15%) |
Heavy menstrual bleeding |
|
12 (20%) |
16 (12%) |
Intermenstrual bleeding |
|
2 (2%) |
1 (1%) |
Frequent bleeding |
|
15 (13%) |
110 (72%) |
Postmenopausal bleeding |
|
79 (54%) |
78 (53%) |
Vaginal discharge |
|
1 (1%) |
1 (1%) |
Pain |
|
Duration of bleeding |
||
|
<1month |
84 (56%) |
15 (17%) |
|
>3 months <6 months |
66 (44%) |
98 (83%) |
Table 2: Symptoms and duration of bleeding in group A and Group B of patients
|
Group A |
|||
|
Ultrasound |
Histology |
||
|
Normal |
64 (44%) |
Proliferative endometrium |
72(48%) |
|
Secretive endometrium |
69 (46%) |
||
|
Atrophic endometrium |
45 (30%) |
||
|
Thickness |
86 (56%) |
Endometrial polyps |
77 (52%) |
|
Adenomyosis |
12 (8%) |
||
|
Fibroma |
22 (15%) |
||
|
Adenocarcinoma |
4 (5%) |
||
|
Decidua |
2 (1%) |
||
|
Endocervical polyps |
4 (2%) |
||
Table 3; Ultrasound and histology findings for Group A
isthmocele. Hysteroscopy had a high accuracy in detecting fibroids (100%), followed by hypertrophic diagnosis (97%), normal endometrium (86%), and polyps (78%). No accuracy was found for the diagnosis of metaplasia/dysplasia Table 5.
DISCUSSION
A combination of patient history, physical examination, laboratory assessment, USG, and endometrial sampling is used to evaluate patients with abnormal uterine bleeding and identify those with dysfunctional uterine hemorrhage. We split the peri and postmenopausal AUB clinical presentations into two groups for this study, and all participants received ultrasonography as well as either a D&C or hysteroscopy. In group A, the majority of the women were between the ages of 38 and 47, with a median of 53, while in group B, the majority of the women were between the ages of 43 and 52, with a median of 40. This is supported by earlier research, which found that having AUB becomes more likely as people age [12, 13]. The beginning of menopause and decreased estrogen levels may be to blame for this. Additionally, we discovered that 94% and 76%, respectively, of the women in groups A and B, were multiparous. According to a prior study, parity increases the incidence of AUB [14]. Another study's sample, which included 91% multiparous women, showed a significant incidence of AUB [15]. Patients in group A had postmenopausal bleeding as their primary complaint (72%), while patients in group B had excessive menstrual bleeding (66%). The bulk of the women in group A were postmenopausal in age, which may account for the increased prevalence of postmenopausal bleeding symptoms in this group.
Group A:
We compared the outcomes of a histological study to the ultrasonographic findings for those patients in the first group A. 44% of patients had normal endometrium, according to the results of their ultrasounds, whereas 56% had thickened. Histology findings of thickness USG after dilatation and curettage showed endometrial polyps, adenomyosis, fibroma, adenocarcinoma, decidua, and endocervical polyps.Among other benign pathologies, secretive endometrium (46% in group A patients) was the second most frequent finding in this investigation. This finding was also seen in earlier studies by Caspi E et al[16] and Bani-Irshaid I and Al-Sumadi A et al[17]. It is unknown what specifically causes bleeding from atrophic endometrium. It is hypothesized that it results from regionally aberrant hemostatic processes or anatomical vascular changes [18]. These findings are comparable to those made by Bafna et al. [19], who discovered that endometrial hyperplasia and polyps were among the factors contributing to postmenopausal hemorrhage. Furthermore, compared to an earlier study [19], the incidence of endometrial adenocarcinoma and carcinoma cervix was substantially lower at 6.6% and 10%, respectively. This could be as a result of a smaller sample size or insufficient tissue for histopathological diagnosis.
Group B:
Group B patients' USG and hysteroscopy findings were compared to the findings of a histological examination. 25% of the sample had normal USG on ultrasound, while 49% of the individuals exhibited thickness. Additionally, the USG revealed 2% IUD, 3% fibroids, 2% isthmocele, and 18% polyps. Hysteroscopy verified the 25% of normal endometrium identified on USG, however, histological analysis revealed both problematic and normal tissue (14% proliferative, 2% secretive, 3% endometrial polyps, 5% endocervical polyps, and 1% hyperplasia without atypia, 1% metaplasia). It may be stated that this resulted in 10% of anomalies histological pathologies that were neither seen during USG nor hysteroscopy, resulting from the 25% normality. The 49% of thick endometrium found on USG were found on hysteroscopy as 3% of fibroids (confirmed as 3% myoma on histology), 32% of endometrial polyps (26% confirmed but 6% cervical polyps), 5% of normal cavity (non-confirmed on histology as 1% metaplasia, 2% fibromaadenomyosis and 3% secretive high grade cervical dysplasia), 1% septum (confirmed as 1% fibrosis on histology), 4% of hypertrophic endometrium (confirmed as 1% fibrosis on histology as atypia complex and hyperplasia without atypia), 1% synechia (which showed with no pathology by histology), 1% polyp(confirmed by fibroma 1%), 2% retained postabortion (confirmed by histology 2% villi). All this result can prove that hysteroscopy has confirmed the thickness found in USG and helped in diagnosis. However, histology was found to be more precise and gave more accurate pathological diagnostic.
|
Group B |
|||||
|
Ultrasound |
Hysteroscopy |
Histology |
|||
|
Normal |
29 (25%) |
Normal cavity and ostia |
29 (25%) |
Proliferative endometrium benign |
16 (14%) |
|
Endometrial polyp |
3 (3%) |
||||
|
Metaplasia |
1 (1%) |
||||
|
Endocervical polyps |
6 (5%) |
||||
|
Secretive endometrium |
2 (2%) |
||||
|
Hyperplasia endometrium without atypia |
1 (1%) |
||||
|
Thickness |
56 (49%) |
Fibroids |
3 (3%) |
Myoma |
3 (3%) |
|
Endometrial polyp |
37 (32%) |
Endometrial polyp |
30 (26%) |
||
|
normal cavity +ostia |
6 (5%) |
Proliferative endometrium benign |
7 (6%) |
||
|
Septum |
1 (1%) |
Cervical polyp |
0 (0%) |
||
|
Hypertrophic endometrium |
5 (4%) |
Metaplasia |
1 (1%) |
||
|
Synechia |
1 (1%) |
Fibroma adenomyosis |
2 (2%) |
||
|
Endometrial polyp |
1 (1%) |
Secretive with high grade cervical dysplasia |
3 (3%) |
||
|
Retained post abortion |
2 (2%) |
Fibrosis |
0 (0%) |
||
|
Hyperplasia with complex atypia |
3 (3%) |
||||
|
Hyperplasia without simple atypia |
2 (2%) |
||||
|
No pathology |
0 (0%) |
||||
|
Fibroma |
1 (1%) |
||||
|
VILLI |
0 (0%) |
||||
|
IUD retention |
2 (2%) |
Remove IUD |
0 (0%) |
Proliferative endometrium benign |
1 (1%) |
|
Secretive endometrium |
1 (1%) |
||||
|
Isthmocele |
2 (2%) |
Hypertrophic endometrium |
5 (4%) |
Proliferative endometrium benign |
1 (1%) |
|
Thick tissue |
1 (1%) |
||||
|
Fibroid |
3 (3%) |
Submucosa fibroid |
1 (1%) |
Submucosa fibroid |
1 (1%) |
|
Submucosa fibroid |
1 (1%) |
Submucosa fibroid |
1 (1%) |
||
|
Septum |
1 (1%) |
Normal cavity +ostia with septum in fundus |
0 (0%) |
Proliferative endometrium benign |
1 (1%) |
|
Polyp |
20 (18%) |
Polyp endometrial |
18 (16%) |
Endometrial polyp |
0 (0%) |
|
Polyp endometrial and cervical |
5 (4%) |
Proliferative endometrium benign |
18 (16%) |
||
|
Secretive endometrium |
4 (4%) |
||||
|
Polyp endometrial + endoc |
1 (1%) |
||||
Table 4
|
Hysteroscopy |
||||||
|
Sensitivity % |
Specificity % |
PPV % |
NPV % |
Accuracy % |
||
|
Ultrasound |
86.21 |
100 |
100 |
94.67 |
96 |
|
|
Histology |
Normal |
100 |
81.33 |
64.10 |
100 |
86 |
|
Fibroids |
100 |
100 |
100 |
100 |
100 |
|
|
Polyps |
58.86 |
100 |
100 |
69.01 |
78 |
|
|
FfHypertrophic |
50 |
100 |
100 |
96.91 |
97 |
|
|
Metaplasia/Dysplasia |
0 |
95 |
0 |
100 |
N/A |
|
Table 5: Sensitivity and Specificity of Hysteroscopy in comparison with TVS and histology findings in Group B
In addition, the retention of IUD (2%) was confirmed by ultrasound and hysteroscopy, on histology by 1% of secretive and 1% proliferative endometrium. For the 2% of isthmoceleon USG, showed 2% of normal cavity by hysteroscopy and were confirmed in histology by 2% of fibrosis tissue. The 3% of fibroma were confirmed with submucosa fibroid by hysteroscopy but histology revealed 1% of endometrial polyp and 2% of submucosa fibroid. Finally, the 18% of polyps found in USG were confirmed with 16% of endometrial and 2% of endocervical polyps by hysteroscopy and confirmed in histology with 16%of proliferative and secretive endometrium and2% polyps. Concerning the sensitivity and specificity of hysteroscopy, hysteroscopy had a significantly higher sensitivity (86.21%), specificity (100%), positive predictive value (100%), negative predictive value (94.67%),and accuracy of 96% in comparison with ultrasound in normality diagnosis. The sensitivity and specificity of ultrasound diagnosis of polyps compared with histology was 89.6% and 39.1%, respectively. For submucosal myomas, sensitivity was 69.2% and specificity 91.3%, suggesting a conclusion that ultrasound is not a reliable method for definitive diagnosis but is an excellent orientation method. Myomas in postmenopausal women are usually asymptomatic and often not treated operatively. However, in premenopausal women, myomas often cause symptoms such as prolonged and heavy bleeding due to cavum deformities and should be treated operatively. Hysteroscopy showed a sensitivity of 100%, specificity of 100%, positive predictive value of 100%, and negative predictive value of 100% in diagnosing endometrial cancer.
Hysteroscopy had a significantly higher sensitivity100%, specificity 100% positive predictive value 100%, negative predictive value 69.01% and accuracy 100 % in diagnosing intra-uterine fibroids and hysteroscopy had a significantly higher sensitivity58.86%, specificity 100%, positive predictive value 100%, negative predictive value 69.01% and accuracy 78 % in diagnosing intra-uterine polyp. According to Audimulapu et al, a study in 2017 conducted on a comparative diagnostic evaluation of hysteroscopy, transvaginal ultrasonography, and histopathological examination in cases of AUB. 38 cases (76%) of hysteroscopy findings correlated with histopathology and discrepancy in findings was noted in 12 cases (24%). In 26 cases (52%), TVS findings correlated with histopathology findings and the results differed in 24 patients (48%)[20]. Vitner et alshowed that ultrasound has 93% sensitivity, 58% specificity, 84.3% positive and 78.3%, negative predictive value while hysteroscopy had 92% sensitivity, 67% specificity, 87.3% positive and 77.7% negative predictive values[21]. Hysteroscopy had a significantly higher sensitivity in diagnosing intra-uterine fibroids while TVS had a significantly higher sensitivity in diagnosing retained products of conception. Although hysteroscopy had better predictive values for diagnosing uterine polyps the difference was not statistically significant [21]. The patients of this study were treated accordingly, AUB was managed conservatively for atrophic endometrium or benign endometrial polyps. Whereas, precancerous histopathologies like cystoglandular hyperplasia, atypical hyperplasia, and complex hyperplasia were subjected to hysterectomy.
Simple endometrial hyperplasia/ proliferative endometrium were put under observation for recurrent episodes of bleeding.
CONCLUSION
The combination of both TVS and hysteroscopy did not seem to improve the sensitivity and specificity. Although transvaginal ultrasonography represented a practical approach for the initial evaluation of uterine pathologies, a hysteroscopy examination would be necessary in most of the suspicious cases. Hysteroscopy remained the best option for the assessment of AUB owing to its diagnostic performance when compared to transvaginal ultrasonography. It allowed direct visualization of the cavity and also sampling for HPE.
However more multicentric studies were required to formulate guidelines to recommend TVS/Hysteroscopy as diagnostic/screening modality alternative to conventional endometrial biopsy.
Funding:
No funding sources
Conflict of interest:
Not declared
Ethical approval:
Not required
Declaration Statement:
Not Applicable
Guarantor:
Not Declared
Contributor Ship:
None Declared
Patient Consent:
Approuver
Acknowledgements:
My Colleagues
REFERENCES
- Mahajan N, Aggarwal M, Bagga AJJom-lH: Health issues of menopausal women in North India. 2012, 3(2):84.
- Kotdawala P, Kotdawala S, Nagar NJJom-lh: Evaluation of endometrium in peri-menopausal abnormal uterine bleeding. 2013, 4(1):16.
- Fraser IS, Langham S, Uhl-Hochgraeber KJERoO, Gynecology: Health-related quality of life and economic burden of abnormal uterine bleeding. 2009, 4(2):179-189.
- Munro MG, Critchley HO, Broder MS, Fraser IS, Gynecology FWGoMDJIJo, Obstetrics: FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. 2011, 113(1):3-13.
- Cheong Y, Cameron IT, Critchley HOJBmb: Abnormal uterine bleeding. 2017, 123(1):103-114.
- Goyal B, Gaur I, Sharma S, Saha A, Das NJMjafi: Transvaginal sonography versus hysteroscopy in evaluation of abnormal uterine bleeding. 2015, 71(2):120-125.
- Choudhary J, Acharya V, Jain M: Evaluation of abnormal uterine bleeding with transvaginal sonography and hysteroscopy in perimenopausal women. 2017.
- Goldstein S, Lumsden MJC: Abnormal uterine bleeding in perimenopause. 2017, 20(5):414-420.
- Radhikabai PK, Borkar KJJoDMIoMSU: Evaluation of abnormal uterine bleeding patients by conventional dilatation and curettage and hysteroscopically guided dilatation and curettage. 2019, 14(4):303.
- Upadhyay A, Tyagi M, Gupta S, Bansal R, Varma YJIJoR, Contraception, Obstetrics, Gynecology: Comparative study of hysteroscopy with ultrasonography and its correlation with histopathology in cases of abnormal uterine bleeding in perimenipausal women. 2022, 11(3):791-798.
- Gkrozou F, Dimakopoulos G, Vrekoussis T, Lavasidis L, Koutlas A, Navrozoglou I, Stefos T, Paschopoulos MJAog, obstetrics: Hysteroscopy in women with abnormal uterine bleeding: a meta-analysis on four major endometrial pathologies. 2015, 291(6):1347-1354.
- Pavone D, Clemenza S, Sorbi F, Fambrini M, Petraglia FJBP, Obstetrics RC, Gynaecology: Epidemiology and risk factors of uterine fibroids. 2018, 46:3-11.
- Salim S, Won H, Nesbitt-Hawes E, Campbell N, Abbott J: Diagnosis and Management of Endometrial Polyps: A Critical Review of the Literature. Journal of Minimally Invasive Gynecology 2011, 18(5):569-581.
- Byna P, Siddula S, Kolli S, Shaik MVJIJoR, Contraception, Obstetrics, Gynecology: Histopathological correlation of abnormal uterine bleeding in perimenopausal women. 2015, 4(6):1876.
- Jagdale N, Gawandi P, Tirankar VJMIJOG: A study of histopathological correlation of abnormal uterine bleeding with clinical symptoms. 2020, 16(2):17-22.
- Ben-Arie A, Goldchmit C, Laviv Y, Levy R, Caspi B, Huszar M, Dgani R, Hagay ZJEJoO, Gynecology, Biology R: The malignant potential of endometrial polyps. 2004, 115(2):206-210.
- Bani-Irshaid I, Al-Sumadi A: Histological findings in women with postmenopausal bleeding: Jordanian figures. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 2011, 17(7):582-586.
- Jairajpuri ZS, Rana S, Jetley SJAAJMS: Atypical uterine bleeding-Histopathological audit of endometrium A study of 638 cases. 2013, 6(1):21-28.
- Kothapally K, Bhashyakarla UJIJoR, Contraception, Obstetrics, Gynecology: Postmenopausal bleeding: clinicopathologic study in a teaching hospital of Andhra Pradesh. 2013, 2(3):344-349.
- Audimulapu S, Sudeepti MJI: A comparative diagnostic evaluation of hysteroscopy, transvaginal ultrasonography and histopathological examination in 50 cases of abnormal uterine bleeding. 2017, 4(8):1-11.
- Vitner D, Filmer S, Goldstein I, Khatib N, Weiner ZJEJoO, Gynecology, Biology R: A comparison between ultrasonography and hysteroscopy in the diagnosis of uterine pathology. 2013, 171(1):143-145.
Annex
50years G5P4 4cs 1 abortion,BMI>35 severebleeding2months ago
vaginal pelvic ultrasoundthickness >1cm
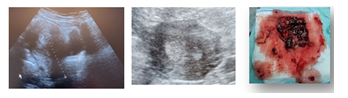
Figure 2
DC done histology villi with deciduas
76 years G6P6 6nvd menopause 15 years cardiopatique, diabetic hypertension, BMI >35,125 kg, severe vaginal bleeding and discharge about 1year, vaginal pelvic ultrasound thickness >2cm DC done histology adenocarcinoma stage
65years G5P4 1abortion 5nvd menopause 14 years hypertension, diabetic severe vaginal bleeding 1month agovaginal pelvic ultrasound thickness >1cm DC done histology revealed endometrial complex hyperplasia with atipia
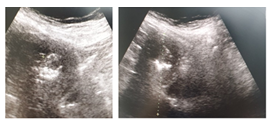
Figure 3
65years G5P4 1abortion 5nvd menopause 14 years hypertension, diabetic severe vaginal bleeding 1month agovaginal pelvic ultrasound thickness >1cm DC done histology revealed endometrial complex hyperplasia with atipia
Figure 4
Figures 5
Figures 6
