Impact of Contrast-Induced Nephropathy on Long-Term Renal Function after Coronary Angiography and Contrast-Enhanced Computed Tomography
Article Information
Hidekazu Moriya1*, Yasuhiro Mochida1, Kunihiro Ishioka1, Machiko Oka1, Kyoko Maesato1, Mizuki Yamano1, Hiroyuki Suzuki1, Takayasu Ohtake1, Sumi Hidaka1, and Shuzo Kobayashi1
1Kidney Disease and Transplant Center, Shonan Kamakura General Hospital, Kanagawa, Japan
*Corresponding author: Hidekazu Moriya, Kidney Disease and Transplant Center, Shonan Kamakura General Hospital, Kanagawa, Japan.
Received: 26 July 2022; Accepted: 01 August 2022; Published: 16 September 2022
Citation:
Hidekazu Moriya, Yasuhiro Mochida, Kunihiro Ishioka, Machiko Oka, Kyoko Maesato, Mizuki Yamano, Hiroyuki Suzuki, Takayasu Ohtake, Sumi Hidaka and Shuzo Kobayashi. Impact of Contrast-Induced Nephropathy on Long-Term Renal Function after Coronary Angiography and Contrast- Enhanced Computed Tomography. Cardiology and Cardiovascular Medicine 6 (2022): 473-479.
Share at FacebookAbstract
Background: It remains unclear whether contrast-induced nephropathy (CIN) has a prognostic impact on subsequent renal dysfunction and whether deteriorating renal function is a risk factor for CIN. This study aimed to evaluate the occurrence of CIN in patients with pre-existing renal dysfunction and investigate the long-term effects of worsening renal function after coronary angiography or contrast-enhanced computed tomography (CT). The prognostic factors of worsening renal dysfunction were also analyzed.
Methods: This was a prospective cohort study of patients at risk for CIN, defined as an estimated glomerular filtration rate (eGFR) <60 mL/ min/1.73 m2 on coronary angiography or eGFR <45 mL/min/1.73 m2 on contrast-enhanced CT. Serum creatinine levels and the 2-year prognosis were evaluated. CIN was defined as an increase in serum creatinine level by more than 0.5 mg/dL or a 25% increase from the previous value within 72 hours after contrast administration. The primary endpoint was the proportion of patients who had serum Cr doubling or induction of dialysis within 2 years according to CIN occurrence.
Results: Of the 410 patients, 19 patients developed CIN (8/142 patients on coronary angiography and 11/268 patients on contrast-enhanced CT), and 38 patients had worsened renal function (21/142 patients on coronary angiography and 17/268 patients on contrast-enhanced CT). CIN was not associated with worsening renal function at 2 years. Analysis by renal function at the time of coronary angiography or contrast-enhanced CT (i.e., eGFR ≥30 ml/min/1.73 m2 and eGFR ≤1.73 m2) found no between group difference in the occurrence of CIN.
Conclusions: CIN is not a prognostic risk factor for the long-term of chronic kid
Keywords
Contrast-Induced Nephropathy; Chronic Kidney Disease; Contrast Media; Prognosis
Contrast-Induced Nephropathy articles, Chronic Kidney Disease articles; Contrast Media articles; Prognosis articles
Article Details
Abbreviations:
CIN- Contrast-Induced Nephropathy; CT- Computed Tomography; eGFR- Estimated Glomerular Filtration Rate
1. Introduction
The use of contrast media increases the risk of worsened renal function in patients with pre-existing renal dysfunction. An estimated glomerular filtration rate (eGFR) <60mL/min/1.73 m2 on coronary angiography eGFR <30 mL/min/1.73 m2 on transvenous contrast-enhanced CT is associated with the risk of contrast-induced nephropathy (CIN). However, data on worsening renal function as a long-term prognosis of CIN are limited. The risk of acute kidney injury after contrast media administration is also influenced by patient- and procedure-related factors. Clinical factors that increase the risk for CIN include pre-existing renal dysfunction, diabetes mellitus in the setting of underlying renal impairment, advanced congestive heart failure, intravascular volume depletion, administration of large volumes of contrast media, and the use of high-osmolar contrast media [1-5]. In 2018, the Japanese Society of Nephrology, the Japanese Society of Radiology, and the Japanese Society of Cardiology jointly developed the “Guideline on the use of iodinated contrast media in patients with kidney disease” [6]. The guidelines include the definition of CIN, patient assessment, and the occurrence of CIN on coronary angiography and contrast-enhanced CT. The guidelines are aimed to prevent the occurrence of contrast media-induced renal dysfunction, standardize renal function assessment methods for patients who use contrast media, and optimize the use of contrast media. However, the guidelines do not clearly state the standardization of renal function assessment after contrast testing, evaluation of long-term effects on renal function, and differentiation from other complications that affect renal function, such as cholesterol crystal embolism. The impact of contrast tests on renal function is important for patients with chronic kidney disease. As such, the long-term decline in renal function and development of other complications due to contrast tests should be carefully considered. This study aimed to evaluate the occurrence of CIN in patients with renal dysfunction who underwent contrast media test and treatment (coronary angiography or contrast-enhanced CT) and the long-term effects of contrast media testing on renal function after. Further, we examined the prognostic factors related to worsening renal function.
2. Materials and Methods
2.1 Study Design and Patients
We prospectively studied the changes in renal function after coronary angiography or contrast-enhanced computed tomography (CT) performed between April 2014 and March 2017. Patients at risk for CIN, defined as an eGFR <60 mL/min/1.73 m2 on coronary angiography or an eGFR <45 mL/min/1.73 m2 contrast-enhanced CT, were eligible. The inclusion criterion was age at least 20 years. The exclusion criteria were as follows: 1) allergy to contrast media, 2) renal replacement therapy, 3) pregnancy, 4) severe liver dysfunction, and 5) hyperthyroidism. Serum saline loading was performed at the discretion of the attending physician before and after administration of contrast media. Pre-study assessments included patient background (age, sex, presence of diabetes, cardiovascular disease, and smoking), examination conditions (amount of contrast medium, volume of supplemental fluid), and history of drug use (diuretics, RAS inhibitors). The blood tests included evaluation of renal function before the contrast test and at 3 days, 1 month, 3 months, 1 year, and 2 years after coronary angiography or contrast-enhanced CT.
2.2 Variable Definitions and Study End Points
CIN was defined as an increase in serum creatinine level by more than 0.5 mg/dL or a 25% increase from the previous value within 72 hours after iodine contrast administration according to the above guideline [1]. Renal cholesterol crystal embolism was defined as (1) cholesterol crystals on renal biopsy or (2) presence of blue toe and rapidly progressive renal dysfunction, reticular plaques in the lower limbs, or eosinophilia (>500/μL). To evaluate the long-term prognosis of renal function after the occurrence of CIN, the primary endpoint was set as worsening renal function, defined as a doubling of serum creatinine or initiation of dialysis at 2 years. The secondary endpoints were the presence of renal cholesterol crystal embolism, death, and an exploratory evaluation of risk factors related to serum creatinine doubling or induction of dialysis at 2 years.
2.3 Statistical Analyses
Our primary analyses were based on assessing the occurrence of CIN and the associations of CIN with outcomes at 2 years in the overall study population, and among subgroups by baseline renal function and comorbidities. Th patients were stratified by comorbidities, and their characteristics were compared using analysis of variance or chi-square tests for categorical variables. Bonferroni analysis was used to evaluate the significance of differences among the groups. All statistical analyses were performed using SPSS statistical software.
3. Results
3.1 Patient Characteristics
Of the 162 patients who underwent coronary angiography, 142 patients were identified to be at risk for CIN and were followed up for 2 years. Meanwhile, of the 283 patients who underwent contrast-enhanced CT examination, 268 were identified to be at risk for CIN and were followed up for 2 years. Thus, 410 patients were included in the analysis. Among them, 19 patients (4.6%; 8/142 (5.6%) patients in the coronary angiography group and 11/268 patients in the contrast-enhanced CT group) developed CIN within 3 days after the administration of contrast media. There were 38/410 (9.3%) patients who had worsening renal function at 2 years. With respect to the long-term prognosis of CIN, 4/19 (21.1%) patients who developed CIN had worsening of renal function thereafter (2 and 2 patients in the coronary angiography and contrast-enhanced CT groups, respectively). The patient characteristics in each group are detailed below.
3.2 Coronary Angiography Group
The mean patient age was 71.6 years, and the mean serum creatinine and eGFR at the time of enrollment were 1.96 mg/dl and 30.1 ml/min/1.73 m2, respectively. There were 48 patients (33.8%) with diabetes mellitus, and 45 patients (31.7%) received serum saline infusion before and after the examination. The mean volume of the contrast medium used was 35 ml (Table 1). The mean serum creatinine level 3 days after angiography was 2.00±0.66 mg/dl, which was not significantly elevated than that at baseline. After 2 years, 21 patients (14.8%) had serum Cr doubling or initiated dialysis, but only 1 patient developed cholesterol crystal embolism. Fifteen patients died, and eleven of them died due to cardiovascular disease (Table 2). Analysis according to renal function at the time of coronary angiography (eGFR ≥30 ml/min/1.73 m2 and eGFR of ≤1.73 m2) showed no significant difference in the occurrence of CIN (Table 3A). There was also no significant association between the occurrence of CIN and worsening of renal function at 2 years (Table 4A). The factors related to the worsening of renal function at 2 years were the presence of cardiovascular disease (i.e., the presence of myocardial infarction, angina pectoris, and chronic heart failure) and pre-existing renal dysfunction at the time of coronary angiography (Table 5).
|
Age (years) |
71.6±12.1 |
|
Sex (M/F) |
119/43 |
|
Smoking |
34 (23.9) |
|
Diabetes |
48 (33.8) |
|
Cardiovascular disease |
56 (39.4) |
|
Systolic blood pressure (mmHg) |
123±14 |
|
Diastolic blood pressure (mmHg) |
78±8 |
|
Blood urea nitrogen (mg/dl) |
28.6±5.6 |
|
Creatinine (mg/dl) |
1.96±0.71 |
|
Estimated glomerular filtration rate (ml/min/1.73m2) |
30.1±11.3 |
|
Albumin (g/dl) |
3.4±0.4 |
|
Hemoglobin (g/dl) |
13.4±2.3 |
|
Eosinophil count (/μl) |
234±22 |
|
Saline infusion (n(%)) |
45 (31.7) |
|
Volume of saline infused (ml) |
845±235 |
|
Volume of contrast media administered (ml) |
35±22 |
Table 1: Patient Characteristics in the Coronary Angiography Group (n=142).
Data are presented as the mean or n (%).
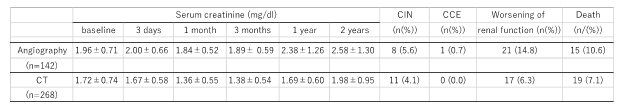
Table 2: Changes in serum creatinine and outcomes at 2 years in patients undergoing coronary angiography or contrast-enhanced computed tomography.
Abbreviations: CT, computed tomography; CIN, contrast-induced nephropathy; CCE, cholesterol crystal
embolism
- A)
|
n=142 |
Renal function at contrast media administration (estimated glomerular filtration rate [eGFR]) |
p |
|
|
≧30 ml/min/1.73m2 |
<30 ml/min/1.73m2 |
||
|
Contrast-induced nephropathy (CIN) (+) |
3 (2.1%) |
5 (3.5%) |
0.441 |
|
CIN (-) |
69 (48.6%) |
65 (45.8%) |
|
B)
|
n=268 |
Renal function at contrast media administration (eGFR) |
p |
|
|
≧30 ml/min/1.73m2 |
<30 ml/min/1.73m2 |
||
|
CIN (+) |
5 (1.9%) |
6 (2.2%) |
0.457 |
|
CIN (-) |
146 (54.5%) |
111 (41.4%) |
|
Table 3: Relationship between the occurrence of CIN and renal function at contrast media administration.
- A) Coronary angiography. B) Contrast-enhanced computed tomography.
A)
|
n=142 |
Worsening of renal function |
p |
|
|
(+) |
(-) |
||
|
Contrast-induced nephropathy (CIN) (+) |
2 (1.4%) |
6 (4.2%) |
0.402 |
|
CIN (-) |
19 (13.4%) |
115 (81.0%) |
|
B)
|
n=268 |
Worsening of renal function |
p |
|
|
(+) |
(-) |
||
|
CIN (+) |
2 (0.7%) |
9 (3.4%) |
0.099 |
|
CIN (-) |
15 (5.6%) |
242 (90.4%) |
|
Table 4: Relationship between occurrence of contrast-induced nephropathy and worsening of renal function at 2 years. A) Coronary angiography. B) Contrast-enhanced computed tomography.
|
Number |
Worsened renal function (n, %) |
p |
||
|
Diabetes |
(-) |
94 |
9 (9.6) |
0.089 |
|
(+) |
48 |
12 (25.0) |
||
|
Cardiovascular disease |
(-) |
86 |
4 (4.7) |
<0.001 |
|
(+) |
56 |
17 (30.4) |
||
|
Diuretics |
(-) |
114 |
15 (13.2) |
0.269 |
|
(+) |
28 |
6 (21.4) |
||
|
Renin angiotensin system inhibitors |
(-) |
54 |
9 (16.7) |
0.621 |
|
(+) |
88 |
12 (13.6) |
||
|
Serum creatinine (mg/dl) |
-1.5 |
78 |
1 (1.3) † |
<0.001 |
|
1.5-2.5 |
42 |
8 (19.4) † |
||
|
2.5- |
22 |
12 (54.5) ‡ |
||
|
Estimated glomerular filtration rate (ml/min/1.73m2) |
45- |
34 |
1 (2.9) |
<0.001 |
|
30-45 |
66 |
6 (9.1) † |
||
|
-30 |
42 |
14 (33.3) † |
||
|
Age |
80- |
34 |
9 (26.5) |
0.053 |
|
60-80 |
78 |
7 (9.0) |
||
|
-60 |
30 |
5 (16.7) |
||
|
Volume of contrast media administered (ml) |
-25 |
78 |
9 (11.5) |
0.112 |
|
25-50 |
44 |
6 (13.6) |
||
|
50- |
20 |
6 (30.0) |
||
|
Saline infusion |
(-) |
97 |
15 (15.5) |
0.739 |
|
(+) |
45 |
6 (13.3) |
Table 5: Factors associated with worsening renal function after coronary angiography (n=142).
†, p <0.001; ‡, p <0.01
3.3 Contrast-Enhanced CT Group
The mean patient age was 74.3 years, and the mean serum creatinine and eGFR at enrollment were 1.72 mg/dl and 35.6 ml/min/1.73 m2, respectively. Diabetes mellitus was present in 76 patients (28.4%), and 47 patients (17.5%) received serum saline infusion before and after the examination. The mean volume of the contrast medium used was 82 ml (Table 6). The serum creatinine level 3 days after contrast-enhanced CT was 1.67±0.58 mg/dl, which was not significantly elevated than that at baseline. At 2 years after the procedure, 17 patients had serum Cr doubling or initiated dialysis, but no patient had cholesterol crystal embolism. Nineteen patients died, and most deaths were due to malignancy or infection (Table 2). Analysis by renal function at the time of contrast-enhanced CT (i.e., eGFR ≥30 ml/min/1.73 m2 and eGFR ≤1.73 m2) showed no difference in the occurrence of CIN (Table 3B). There was no significant association between the occurrence of CIN and the 2-year prognosis of renal function, similar in the coronary angiography group (Table 4B). The factors associated with the 2-year prognosis of renal function were age and diabetes mellitus, in addition to pre-existing renal dysfunction (Table 7).
|
Age (years) |
74.3±11.1 |
|
Sex (M/F) |
177/109 |
|
Smoking |
48(17.9) |
|
Diabetes |
76(28.4) |
|
Cardiovascular disease |
42(15.7) |
|
Systolic blood pressure (mmHg) |
132±12 |
|
Diastolic blood pressure (mmHg) |
82±8 |
|
Blood urea nitrogen (mg/dl) |
20.5±5.6 |
|
creatinine (mg/dl) |
1.72±0.74 |
|
Estimated glomerular filtration rate (ml/min/1.73m2) |
35.6±8.8 |
|
Albumin (g/dl) |
3.3±0.4 |
|
Hemoglobin (g/dl) |
11.8±1.8 |
|
Eosinophil count (/μl) |
379±65 |
|
Saline infusion (n(%)) |
47(17.5) |
|
Volume of saline infused (ml) |
568±40 |
|
Volume of contrast media administered (ml) |
82±34 |
Table 6: Patient characteristics in the contrast-enhanced computed tomography group (n=268).
Data are presented as the mean or n (%).
|
Number (n) |
Worsening renal function, n (%) |
p |
||
|
Diabetes |
(-) |
192 |
7 (3.6) |
<0.001 |
|
(+) |
76 |
10 (13.2) |
||
|
Cardiovascular disease |
(-) |
226 |
11 (4.7) |
0.125 |
|
(+) |
42 |
6 (14.3) |
||
|
Diuretics |
(-) |
234 |
13 (5.6) |
0.127 |
|
(+) |
34 |
4 (11.8) |
||
|
Renin angiotensin system inhibitor |
(-) |
192 |
11 (5.7) |
0.529 |
|
(+) |
76 |
6 (7.9) |
||
|
Serum creatinine (mg/dl) |
-1.5 |
186 |
0 (0.0) |
<0.001 |
|
1.5-2.5 |
55 |
8 (14.5) † † |
||
|
2.5- |
27 |
9 (33.3) |
||
|
Estimated glomerular filtration rate (ml/min/1.73m2) |
30-45 |
211 |
6 (2.8) |
<0.001 |
|
-30 |
57 |
11 (19.3) |
||
|
Age |
-80 |
34 |
7 (20.6) |
0.002 |
|
60-80 |
176 |
7 (4.0) ‡ * |
||
|
60- |
58 |
3 (5.2) |
||
|
Volume of contrast media administered (ml) |
−50 |
16 |
2 (12.5) |
0.132 |
|
50-100 |
212 |
10 (4.7) |
||
|
100- |
40 |
5 (12.5) |
||
|
Saline infusion |
(-) |
221 |
13 (5.9) |
0.56 |
|
(+) |
47 |
4 (8.5) |
Table 7: Factors correlated with renal function deterioration in the contrast-enhanced CT group (n=268).
†, p <0.001; ‡, p <0.01; *, p <0.05
4. Discussion
In the past, it was considered that the use of contrast media had a risk of worsening renal function. However, in the present study, CIN is not a prognostic risk factor for the long-term of chronic kidney disease after coronary angiography or contrast-enhanced CT. Pre-existing renal dysfunction is also not a risk factor for CIN, even if the eGFR is <30 ml/min/1.73 m2. Contrast-induced acute kidney injury is characterized by a decrease in renal function that occurs within 3 days after the intravascular administration of an iodinated contrast material. After contrast media exposure, vasoconstriction leads to intense, but transient reduction in renal blood flow, direct toxicity to the renal tubular epithelium, and tubular obstruction by protein precipitates [7]. It is generally believed that arteriography is associated with a higher risk of contrast-induced acute kidney injury than venography (e.g., contrast-enhanced CT) owing to the delivery of a more concentrated contrast material to the kidneys with angiography and the higher overall risk profile of patients requiring such procedures [8]. The 2012 Japanese guidelines on the use of contrast media initially stipulated that a contrast-enhanced CT scan was associated with a risk of CIN in patients with eGFR <45 ml/min/1.73 m2. However, the revised guidelines in 2018 lowered the risk level to eGFR <30 ml/min/1.73 m2 [6]. Several studies have also reported that there is no risk of CIN even in patients with eGFR <30 ml/min/1.73 m2 [9-12]. Meanwhile, the risk of CIN remains high in coronary angiography. In this study, the risk of CIN was not significantly related to renal function at the time of angiography, even in patients with eGFR <30 ml/min/1.73 m2. There was also no risk of CIN in contrast-enhanced CT scan in patients with eGFR <30 ml/min/1.73 m2. Recent studies have suggested that the risk of acute kidney injury due to contrast material is overestimated [13-17]. The rate of CIN in the present study is lower (5.6% for arterial contrast and 4.1% for venous contrast) than in previous studies despite that we included only patients with pre-existing renal dysfunction. Contrast media-induced renal dysfunction in both coronary angiography and contrast-enhanced CT is a risk factor for long-term renal dysfunction. However, this study found that the occurrence of CIN was not significantly related to pre-existing renal dysfunction on either coronary angiography or contrast-enhanced CT. Furthermore, even if CIN occurs, it is not associated with the long-term prognosis of renal function. These findings support that there is a reconsideration of “renalism,” in which patients are discouraged from having contrast studies because of fear of developing CIN, even though these studies are necessary. However, pre-existing chronic kidney disease is the strongest patient-related risk factor for long-term renal prognosis, regardless of the occurrence of CIN. We also found that in coronary angiography, a history of cardiovascular disease was associated with long-term renal prognosis. Most patients with cardiovascular disease undergo coronary angiography. Therefore, cardiac function assessment of prior to coronary angiography is extremely important. In this study, saline administration before and after angiography or the amount of contrast media used did not lower the risk of CIN, but this may be due to the small sample size. Only one case of cholesterol crystal embolism was found on coronary angiography in the current study. Cholesterol crystal embolism causes systemic organ embolism due to the dissemination of cholesterol crystals caused by the continuous disintegration of atherosclerotic foci in the walls of large vessels such as the aorta. Thus, it has poor prognosis. The general population has an approximately 0.06% In probability of cholesterol crystal embolism after cardiac catheterization [18]. The subjects of the present study were patients with pre-existing renal dysfunction, and the percentage of occurrence of cholesterol crystal embolism in this study cannot be simply compared with that of previous reports. A recent approach to coronary angiography is mainly the radial artery, and the occurrence of cholesterol crystal embolism is expected to be lower than that in the past. However, when renal function deteriorates after coronary angiography, it is necessary to pay attention not only to changes in serum creatinine, but also to the eosinophil count and lower limb symptoms. This study has some limitations. First, the sample size was small, and thus, the study findings may have limited generalizability. Second, this was a single-center study, limiting the external validity of the findings. Third, it was not possible to accurately determine whether the preoperative administration of serum saline was ineffective because the use of serum saline was randomly assigned by the attending physician’s judgment. A larger clinical study is needed in the future.
5. Conclusion
CIN is not a risk factor of long-term renal prognosis after coronary angiography or contrast-enhanced CT scans. Pre-existing renal dysfunction does not increase the risk of CIN, even in patients with an eGFR <30 ml/min/1.73 m2. These findings will provide a help that patients with kidney disease who need contrast-enhanced testing should be tested appropriately.
Availability of Data and Materials
The datasets generated and/or analysed during the current study are not publicly available due to limitations of ethical approval involving the patient data and anonymity but are available from the corresponding author on reasonable request.
Acknowledgement
We would like to thank Editage (www.editage.com) for English language editing.
Funding
None.
Contributions
HM, YM, KI, MO, KM, MY, HS, TO, SH collected data. HM analyzed data and wrote the manuscript. HM and SK designed the study and critically reviewed the manuscript. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Ethics Declarations
This study was approved by the Tokushukai Group Ethics Committee (Registration number: TGE00389-024) and was conducted according to the tenets of the Helsinki Declaration. Informed consent was obtained from all patients.
Competing Interests
The authors report no conflicts of interest.
References
- Barrett BJ. Contrast nephrotoxicity. Am Soc Nephrol 5 (1994): 125-137.
- Taliercio CP, Vlietstra RE, Fisher LD, et al. Risks for renal dysfunction with cardiac angiography. Ann Intern Med 104 (1986): 501-504.
- Rudnick M, Tumlin J. Pathogenesis, clinical features, and diagnosis of radiocontrast media-induced acute kidney in- jury (acute renal failure). In: Up to Date, edited by Rose BD, UpToDate, Waltham, MA (2007).
- Manske CL, Sprafka JM, Strony JT, et al. Contrast nephropathy in azotemic diabetic patients undergoing coronary angiography. Am J Med 89 (1990): 615-620.
- Barrett BJ, Parfrey PS, Vavasour HM, et al. Contrast nephropathy in patients with impaired renal function: high versus low osmolar media. Kidney Int 41 (1992): 1274 -1279.
- Isaka Y, Hayashi H, Aonuma K, et al. Guideline on the use of iodinated contrast media in patients with kidney disease 2018. Clin Exp Nephrol 24 (2020): 1-44.
- Gruberg L, Mintz GS, Mehran R, et al. The prognostic implications of further renal function deterioration within 48 h of interventional coronary procedures in patients with pre-existent chronic renal insufficiency. J Am Coll Cardiol 36 (2000): 1542-1548.
- Mehran R, Dangas GD, Weisbord SD. Contrast-Associated Acute Kidney Injury. N Engl J Med 380 (2019): 2146-2155.
- McDonald JS, McDonald RJ, Carter RE, et al. Risk of intravenous contrast material-mediated acute kidney injury: a propensity score-matched study stratified by baseline-estimated glomerular filtration rate. Radiology 271 (2014): 65-73.
- Hinson JS, Ehmann MR, Fine DM, et al. Risk of Acute Kidney Injury After Intravenous Contrast Media Administration. Ann Emerg Med 69 (2017): 577-586.e4.
- McDonald JS, McDonald RJ, Williamson EE, et al. Is Intravenous Administration of Iodixanol Associated with Increased Risk of Acute Kidney Injury, Dialysis, or Mortality? A Propensity Score-adjusted Study. Radiology 285 (2017): 414-424.
- Tao SM, Kong X, Schoepf UJ, et al. Acute kidney injury in patients with nephrotic syndrome undergoing contrast-enhanced CT for suspected venous thromboembolism: a propensity score-matched retrospective cohort study. Eur Radiol 28 (2018): 1585-1593.
- McDonald JS, Leake CB, McDonald RJ, et al. Acute kidney injury after intravenous versus intra-arterial contrast material administration in a paired cohort. Invest Radiol 51 (2016): 804-809.
- McDonald RJ, McDonald JS, Bida JP, et al. Intravenous contrast material-induced nephropathy: causal or coincident phenomenon? Radiology 267 (2013): 106-118.
- McDonald RJ, McDonald JS, Carter RE, et al. Intravenous contrast material exposure is not an independent risk factor for dialysis or mortality. Radiology 273 (2014): 714-725.
- Bruce RJ, Djamali A, Shinki K, et al. Background fluctuation of kidney function versus contrast- induced nephrotoxicity. AJR Am J Roentgenol 192 (2009): 711-718.
- Goulden R, Rowe BH, Abrahamowicz M, et al. Association of Intravenous Radiocontrast With Kidney Function: A Regression Discontinuity Analysis. JAMA Intern Med 5 (2021): e210916.
- Johnson LW, Esente P, Giambartolomei A, et al: Peripheral vascular complications of coronary angioplasty by the femoral and brachial techniques. Cathet Cardiovasc Diagn 3 (1994): 165-172.
