Healthcare Workers' Experience in Saudi Health institutes with Post- Exposure Management against Bloodborne Pathogens
Article Information
Hani S Almugti1, Mujib M Alzahrani2, Amani T Barnawi3, Maram Alajmi4, Abdulrahman A Alharbi5, Tariq Alkaabi6, Fatimah A Bajafar7, Mohammed A Al Garni8, Azzah Alfaden9, Mohai Eddin Bali10, Sari A AlSulami11, Mohamad F AlMathkouri12, Fatima M Shaheen13, Murtadha H Alameer14, Omar M Al Saeidi15
1Primary Health Care, Ministry of National Guard - Health Affairs, King Abdullah International Medical Research Center, King Saud bin Abdul-Aziz University for Health Sciences, Jeddah City, SAU
2Faculty of Medicine, Faculty ofMedicine, Al Baha University, Baha , SAU
3PHC, Ministry of Health Holdings / Azzaher hospital, Makkah, SAU
4Plastic and Reconstructive Surgery, Al-Adan Hospital, Ahmadi, KWT
5Intensive Care Unit, King Faisal Hospital, Makkah, SAU
6General Practice, King Faisal Hospital, Makkah Almukarramah, SAU
7Medicine, Al Qunfudah Hospital, Al Qunfudah, SAU
8Radiology, Thurayban General Hospital/ General Directorate Al Qunfudhah Health Affairs, Al Qunfudah, SAU
9Primary Healthcare, Ministry of Health Holdings, Medinah, SAU
10Adult Intensive Care Unit, King Fahad Specialist Hospital, Dammam, SAU
11Intensive Care Unit, Rabigh General Hospital, Rabigh, SAU
12Internal Medicine, Ahmadi Health Area, Kuwait, KWT
13Medical Intern, Salmaniya Medical Complex, Bahrain , BHR
14Neurosurgery, King Fahad Hospital, Huffof, SAU
15Internal Medicine, Jahra Hospital, Jahra, KWT
*Corresponding author: Hani S. Almugti, Primary Health Care, Ministry of National Guard - Health Affairs, King Abdullah International Medical Research Center, King Saud bin Abdul-Aziz University for Health Sciences, Jeddah City, SAU.
Received: 15 February 2022; Accepted: 22 February 2022; Published: 03 March 2023
Citation:
Hani S Almugti, Mujib M Alzahrani, Amani T Barnawi, Maram Alajmi, Abdulrahman A Alharbi, Tariq Alkaabi, Fatimah A Bajafar, Mohammed A Al Garni, Azzah Alfaden, Mohai Eddin Bali, Sari A AlSulami, Mohamad F AlMathkouri, Fatima M Shaheen, Murtadha H Alameer, Omar M Al Saeidi. Healthcare Workers' Experience in Saudi Health institutes with Post- Exposure Management against Bloodborne Pathogens. Archives of Clinical and Biomedical Research 7 (2023): 125-132.
Share at FacebookAbstract
Background: Effective measures to prevent occupational injuries are required to create a safety culture in any health institute. Establishing a baseline assessment of these measures is recommended for planning and improvement purposes. The objective of the present study was to measure how healthcare workers perceive a culture of safety and sharps injury prevention in their healthcare institutes by using the adapted survey of the sharps injury prevention workbook from Disease Control and Prevention (CDC).
Methods: A cross-sectional study was conducted using electronic selfadministered questionnaires; the questions were answered and submitted by 397 healthcare workers who met the inclusion criteria through a nonprobability sampling technique.
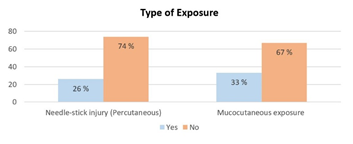
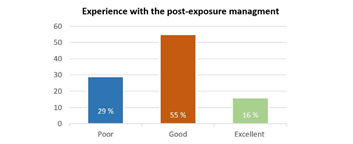
Results: The overall perception of the safety and sharps injury prevention culture was good and positive among 397 healthcare workers from the four Saudi health sectors. However, almost a third of them admitted having at least one occupational exposure to blood or other body fluids (26 % had needle stick injury, and 33 % had mucocutaneous exposure). Moreover, a third of the exposed workers reported poor experience with post-exposure management in their health institutes. It was somewhat surprising that the participants from private hospitals had low perception scores (p < 0.001).
Conclusion: Participants in this study had a good perception regarding the culture of safety and sharps injury prevention at their health institutes. The results of this study indicate that the perception of healthcare workers toward leadership support should be demonstrated and addressed by frequent assessment for the purpose of culture safety improvement.
Keywords
Healthcare Workers; Perception; Occupational Injury; Saudi Arabia; Safety Culture
Healthcare Workers articles; Perception articles; Occupational Injury articles; Saudi Arabia articles; Safety Culture articles
Article Details
1. Introduction
Exposure to bloodborne pathogens from needle sticks and other sharps injuries is a preventable occupational problem. Hepatitis B and C virus with human immunodeficiency virus (HIV) represent the greatest risk of occupational infections among healthcare workers (HCWs) [1]. The World Health Organization (WHO) estimated that needle-stick injuries cause 39%, 37%, and 4.4%, respectively, of hepatitis C, hepatitis B, and HIV infections [2]. Occupational hazards to HCWs have lately earned more national attention than forty years ago. Many researchers studied the incidence of needle-stick and sharps injuries (NSSI). It was 30 NSSI per 100 beds per year in the United States [3] compared with 100,000 NSSI per year in the United Kingdom [4]. In Saudi Arabia [5], NSSI was 33 per 1000 HCWs in a prospective study conducted in a tertiary center. Providing a safe environment by health institutes is considered one of the rights of patients and healthcare personnel. For that, at the national level, regulatory agencies have always systematically overseen and monitored the necessity of addressing hazard prevention in healthcare organizations. Consequently, the implementation of a range of risk-management strategies (HCWs), including administrative controls and engineering controls of needle devices [6,7], reduced the exposure incidents, including needle sticks and subsequent infection in healthcare workers. Despite that, needle-stick injuries and other types of exposures continue to occur, and many researchers observed a considerable number of underreported incidents of needle-stick and sharps injuries [8]. On the other hand, there is increasing concern about the high degree of anxiety after exposure and the potential effects of psychological disturbances on healthcare workers' productivity and work quality [7,8]. Changing long-standing practices is difficult, and even with all the pre-exposure precautions, occupational injuries will continue. On the other hand, post-exposure management is considered a complementary and integral part of the whole prevention strategy [1]. It includes determining the risk of transmission through a detailed history and laboratory testing with prompt delivery of the appropriate post-exposure prophylaxis (PEP) if indicated. Since the initial logical step to start the post-exposure treatment process is to report occupational injuries, healthcare providers should be trained on the immediate reporting of their occupational injuries, as the benefit of prophylactic management resides in the early days of injury [9]. Yet there is concern about healthcare workers' compliance with the pre and post-exposure recommendations. In Saudi Arabia, many studies have mainly addressed the knowledge level of these recommendations among HCWs, the reporting rate of exposure, and the clinical consequences of occupational exposure among healthcare workers [10,11]. Creating a safety culture, reporting injuries, analyzing data, and selecting and evaluating devices are the backbone of the sharps injury prevention program. Health institutes are required to have a baseline assessment of these processes for effective program planning and improvement [9]. From healthcare workers' perception, the present study aimed to help healthcare organizations measure how their employees perceive a culture of safety and sharps injury prevention for the purpose of improvement.
2. Aim of the Study
The study aimed to assess the operation processes of occupational health programs in Saudi healthcare institutes from the perspective of safety culture and sharps injury prevention. The primary (Specific) objective was to measure how healthcare workers perceive a culture of safety and sharps injury prevention in their healthcare institutes by using the adapted survey of the sharps injury prevention workbook from Disease Control and Prevention (CDC).
3. Materials and Methods
3.1 Study Area/Setting
The study was carried out in Saudi Arabia. Saudi Arabia provides healthcare services to more than 30 million citizens and residents, as well as several million visitors during Hajj and Umrah. These services are provided through several healthcare sectors such as medical cities, specialized hospitals, university and military hospitals, and primary care centers. The participants of the current research were approached through the electronic questionnaire that was distributed on Facebook, Whats app, and Twitter, which are considered the most popular social media used by the Saudi nation.
3.2 Study Subjects and Study Design
The present study is a cross-sectional study, subjects were the healthcare workers who were working at Saudi health institutes and had the job title of physicians, dentists, nurses, emergency medical personnel, laboratory technicians, pharmacists, and administrative staff. However, students and interns from the medical and health college were excluded from this study.
3.3 Sample Size and Sampling Technique
As per the latest report, the total number of healthcare workers in Saudi Arabia is 400,000[12]. With a confidence level of 95% and a margin of error of 5%, the present study will recruit 384 healthcare workers after applying the inclusion and exclusion criteria. A multistage sampling technique will be used. The first stage is a stratified cluster at the levels of healthcare institutions (Ministry of Health hospitals, Military hospitals, university hospitals, and private healthcare institutions). Through non-probability sampling (snow bowling sampling), the study recruited roughly 100 healthcare workers from each stratum using a self-administered online questionnaire after applying the inclusion and exclusion criteria to the participants.
3.4 Data Collection Methods, Instrument Used, Measurements: Variables
The dependent vriables were the mean score of the perception of healthcare workers against the culture of safety and sharps injury prevention at their health institutes. Whereas the independent variables were the age, gender, nationality, profession, length of experience, hospital (governmental or private), and workers' affiliated departments.
3.4.1 Definition of the Culture of Safety [9]: The shared commitment of management and staff to ensure workplace safety is known as a "culture of safety" [9]. All aspects of the workplace interplay with a safety culture. Employees perceive the presence of a culture of safety based on multiple factors, including management commitment to safety, healthcare personnel involvement in safety decisions, method of handling safety hazards in the work environment, feedback on safety improvements, promotion of individual accountability.
3.5 Questionnaire: (see the appendix)
The questionnaire of this study was electronic, self-administered, and consisted of three sections (see Appendix A). The assessment of the healthcare workers' perceptions was taken from a survey of the sharps injury prevention workbook[9]from Disease Control and Prevention (CDC). However, the questionnaire of this study was tested for validity (face and content validity ensured by revising the questionnaire from an expert panel of occupational medicine, preventive medicine, infection control, and health quality). Furthermore, the reliability was tested through a pilot sample, and the internal consistency from Cronbach's alpha coefficient was 0.76, indicating good reliability. However, the levels of perception were estimated by using the suggested scoring system,the highest total score was, 50 and the grading scores were calculated for each participant and categorized into poor perception if the total score is less than 16, good perception if the total score is from 16 to 33 and, excellent perception if the total score is more than 33.
3.6 Data Management and Analysis Plan
The Windows-based SPSS statistical software suite was used for data entry and analysis (version 20.0; IBM Corp., Armonk, NY, USA). Data entry and coding stages were performed to enhance the data quality. Data presented using frequencies and percentages for qualitative variables, and means and standard deviations for quantitative variables. The median test was used between participants' answers and other variables to record the statistically significant.
3.7 Ethical Considerations
Data collection was started after obtaining permission from the ethical and scientific committee of King Abdullah International Medical Research Center at King Abdul-Aziz Medical City. The participants' confidentiality was ensured, and the data was kept confidential throughout the research. Consent to participate in the present study was obtained from the patients.
4. Results
4.1 Demographic Information
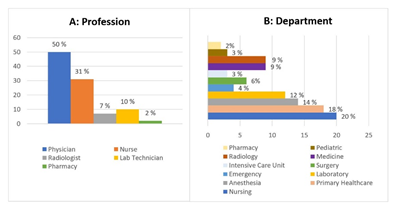
As indicated in Table 1, 397 healthcare workers from the study population responded to our online questionnaire, and from each predefined Saudi health sector, we got approximately a quarter of the participants. Almost half of them were from the age group of less than 30. Nearly two-thirds of the participants (71%) were Saudi, and more than half (60.5%) were females. Slightly more than half of them (57 %) had an average of more than five years of tenure at their present job. The occupational history of participants is summarized in Figure 1. Half of the participants (50 %) were physicians, and a third (30 %) were nurses. However, the participants were working in different departments, 20 % of them from the nursing department.
|
Demographic characteristics |
Frequency (n) |
Percent (%) |
|
Age category |
||
|
20 - 30 years |
213 |
53.7 |
|
31 - 40 years |
167 |
42.1 |
|
41 - 50 years |
17 |
4.3 |
|
Gender |
||
|
Male |
157 |
39.5 |
|
Female |
240 |
60.5 |
|
Nationality |
||
|
Saudi |
285 |
71.8 |
|
Non- Saudi |
112 |
28.2 |
|
Health Sectors |
||
|
Governmental Hospitals (Ministry Of Health) |
110 |
28 |
|
Governmental Hospitals (Military) |
105 |
26 |
|
University Hospitals |
101 |
25 |
|
Private Hospital |
81 |
20 |
|
Length of Experience |
||
|
Less than five years |
170 |
42.8 |
|
From five to ten years |
114 |
28.7 |
|
More than ten years |
113 |
28.5 |
Table 1: Demographic characteristics of participants (n=397).
4.2 History of Exposure to Blood or Other Body Fluids
As shown in Figure 2, almost two third of participants did not experience exposure to blood or other body fluids. In contrast, a third of them (26 % had needle stick injury, and 33 % had mucocutaneous exposure) admitted to having at least one occupational exposure to blood or other body fluids. Figure 3 demonstrates that 77% of participants statedthat their health institutes have a procedure or protocol regarding the reporting system of blood and bodily fluids exposure. Despite that, 12% of participants only reported their exposure incidents, reflecting that nearly half of those with a history of exposure in the present study did not report their incidents. Concerning participants' experience with the post-exposure management provided by their health institutes, Figure 4 indicates that two-thirds of participants who had exposure to blood or other body fluids reported good and excellent experiences of post-exposure management.
4.3 Perceptions of a Culture of Safety
In response to the question that was designed to represent the culture of safety in health institutes, approximately three percent (3 %) of participants were categorized as having a poor perception of the culture of safety. However, the majority of participants (97%) had good and excellent perception, and the median score for the overall score was 31, with a confidence interval of (29.71 - 30.59) (Table 2). Table 3 illustrates that almost half of the participants were uncertain about the two first questions related to their health institutes' commitment to safety and whether the health institutes considered safety an active agenda for discussion during staff meetings. On the other hand, about a third of the participants reported that their organization did not support or encourage reporting of errors and hazardous conditions and did not include personal accountability for safety as an evaluation item of the annual performance evaluations of their employees. However, the overall responses to other questions were very positive. In regards to the relationship between participants' total perception score and their characteristics (demographic and occupational), Table 4 demonstrates the absence of any association of statistical significance between participants' perception and their demographic characteristics. However, there were trends of lower perception scores among participants of private hospitals, and interestingly, the differences reached statistical significance (p < 0.001).
|
Score of perceptions |
||
|
Total Score |
||
|
95 % CI* |
29.71 – 30.59 |
|
|
Range |
14- 38 points |
|
|
Median |
31 points |
|
|
Mode |
31 |
|
|
Mean ± SD** |
30 ± 4.4 points |
|
|
Score Category |
Frequency |
Percent (%) |
|
Poor |
12 |
3 |
|
Good |
318 |
80 |
|
Excellent |
67 |
17 |
Table 2: Participants' perceptions score of the culture of safety (n=397).
*CI: Confidence Interval, **SD: Standard Deviation.
|
Item |
No (%) |
Score (max=5) |
||||
|
Agree/ Strongly agree |
Uncertain |
Disagree/ Strongly disagree |
Mean ± SD |
Median |
||
|
1. Commitment to safety |
142 (35 %) |
205 (52 %) |
50 (13 %) |
2.8 ± 0.4 |
3 |
|
|
2. Feedback on safety |
151 (38 %) |
180 (45 %) |
66 (17 %) |
2.9 ± 0.7 |
3 |
|
|
3. Promotion of hazard reporting |
175 (44 %) |
91 (23 %) |
131(33 %) |
3 ± 0.4 |
3 |
|
|
4. Personal accountability |
227 (57 %) |
27 (7 %) |
143 (36 %) |
3.1 ± 1.12 |
4 |
|
|
5. Hazard correction |
297 (75 %) |
57 (14 %) |
43 (11 %) |
3.8 ± 1.1 |
4 |
|
|
6. Availability of sharps containers |
249 (63 %) |
87 (22 %) |
61 (15 %) |
3.5 ± 1.05 |
4 |
|
|
7. Employee/management collaboration on safety |
267 (67 %) |
85 (21 %) |
45 (12 %) |
3.7 ± 0.98 |
4 |
|
|
8. Safety training |
276 (69 %) |
103 (26 %) |
18 (5 %) |
3.7 ± 0.79 |
4 |
|
|
9. Provision of safer technology |
251 (63 %) |
107 (27 %) |
39 (10 %) |
3.6 ± 0.9 |
4 |
|
|
10. Non-punitive reporting environment |
350 (88 %) |
23 (5.8 %) |
24 (6 %) |
4 ± 0.8 |
4 |
|
Table 3: Culture of safety perceptions among all participants (n=397).
|
Demographic and Occupational characteristics |
Perception score (max=50) |
||
|
Median |
Median test Statistic |
p-value |
|
|
Age category |
|||
|
20 - 30 years |
31 |
||
|
31 - 40 years |
30 |
||
|
41 - 50 years |
31 |
5.1 |
0.07 |
|
Gender |
|||
|
Male |
30 |
||
|
Female |
31 |
2.5 |
0.13 |
|
Nationality |
|||
|
Saudi |
31 |
||
|
Non- Saudi |
31 |
3.05 |
0.61 |
|
Health Sectors |
|||
|
Governmental Hospitals (Ministry Of Health) |
31 |
||
|
Governmental Hospitals (Military) |
33 |
||
|
University Hospitals |
26 |
||
|
Private Hospital |
33 |
7.3 |
0.009* |
|
Profession |
|||
|
Physician |
31 |
||
|
Nurse |
31 |
||
|
Radiologist |
30 |
||
|
Lab worker |
30 |
||
|
Pharmacist |
31 |
4.2 |
0.06 |
|
Length of Experience |
|||
|
Less than five years |
30 |
||
|
From five to ten years |
31 |
||
|
More than ten years |
31 |
2.7 |
0.249 |
Table 4: Relation between participants' total perception score and their characteristics. (n=397).
5. Discussion
According to the statistical report from Saudi Arabia [12], about half of the country's healthcare workers are Saudi citizens, and females comprise the majority of workers among the nursing staff. The present study was designed to assess the perception of healthcare workers in Saudi Arabia concerning a culture of safety and sharps injury prevention at their health institutes. The majority of participants were Saudi (71 %), and the female staff comprised 60 % of them. Moreover, because the culture of safety of the health institution is closely related to the administrative system, four health institutions were identified in order to assess the perception of the safety culture and sharps injury prevention among their workers. Occupational exposure to blood is a highly prevalent risk to healthcare workers. Globally, there are variations in the incidence rates of blood exposure throughout various studies depending on countries, the number of hospital beds, the job category of health staff, and different data recording periods. In the present study, almost a third of participants experienced blood exposure during their careers. This rate is higher than others reported in Saudi medical literature [13,14], similar to studies conducted in Iran [15] and Lebanon [16], and lower than one previous study in Egypt [17]. The anonymous data collection from participants in the current study allowed for admitting incidents of exposure that were never reported, which could explain the increased prevalence rate of blood exposure compared to previous studies that used registries or other data sources. Reporting the incidences of blood exposure to the hospital's concerned authorities is a challenge that requires leadership support. The present findings seem consistent with other research, which found that less than half of the exposed individuals only reported their blood exposure incidents [13,18]. Further, this underreporting phenomenon may explain the lower exposure rates recorded in previous studies where the data source was from reporting papers. For the purpose of detecting and preventing positive seroconversion as promptly as possible, post-exposure management should be followed after accidental occupational exposure to blood and bodily fluids. Among those who had exposure to blood or other body fluids, the present study showed almost two-thirds expressed their satisfaction with post-exposure management and the follow-up care provided by the occupational clinic. However, the previous research [7] highlighted the dissatisfaction with waiting time and the need for rapid turnaround time for source patients' test results, which might help reduce the panic and anxiety among most healthcare workers. Institutionalizing a safety culture to protect patients, personnel, and others in the healthcare environment is an essential element of the success of the occupational injury prevention program. In the present study, the overall perception of a culture of safety was good in Saudi health institutes. It is interesting to note that although the health institutes were striving to build a culture of safety for their workers, half of the participants were uncertain whether workers' safety was a priority in their healthcare organization. Moreover, the perception was poor among a third of them regarding their organizations' efforts to encourage and reward the recognition and reporting of errors and hazardous conditions. This discrepancy could be attributed to the misunderstanding of the leadership role [19] of the culture of safety in their health institutes. According to the results of the present study, none of the participants' personal characteristics had a significant relationship to their perceptions of the safety culture in their health institutes. This supports the generalization of this survey and indicates equal perception scores across all ages, gender, job types, and different lengths of experience. Contrary to expectations, this study showed lower perception scores among healthcare workers in private hospitals, however, this statistical significance result is difficult to be explained, but it might be related to the fact [20] that the private health sector has a different system that is neither owned nor directly controlled by government regulations in regard culture of safety. Limitations of the current study include the fact that it was cross-sectional; hence, the results are mainly observations for formulating the hypothesis only. Additionally, because of the limited accessibility to the Saudi health institutes, we could not use the probability sampling technique and thus influence the level of research generalizability.
6. Conclusion
This study has shown that the perception of a culture of safety and sharps injury prevention was optimal among healthcare workers in Saudi institutes. Despite significant progress in lowering the risk of occupational exposure to bloodborne pathogens, there is still a need to do more. Leadership support and commitment to promoting safety should be translated and demonstrated by assessing the culture of safety perception of the employees as baseline data for the purposes of future improvement.
Conflict of Interest and Financial Relationships
All authors have declared that they have no conflict of interest or financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Authorship
The manuscript has been read and approved by all the authors, that the requirements for authorship have been met, and that each author believes that the manuscript represents honest work
References
- Updated U.S. public health service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for post exposure prophylaxis. Recommendations and reports 50 (2001): 1-42.
- World Health Organization (WHO). Sharps injuries: global burden of disease from sharps injuries to healthcare workers. (2003).
- National institute for occupational safety and health (NIOSH). Preventing needle stick injuries in health care settings. (2000).
- O'Connor MB. Needlestick injury advice in the UK and Ireland. Journal of Hospital Infection 1 (2009): 185-186.
- Memish ZA, Almuneef M, Dillon J. Epidemiology of needle-stick and sharps injuries in a tertiary care center in Saudi Arabia. American journal of infection control 1 (2002): 234-241.
- Jagger J, Hunt EH, Pearson RD. Sharp object injuries in the hospital: causes and strategies for prevention. American journal of infection control 18 (1991): 227-231.
- Gershon RR, Flanagan PA, Karkashian C, et al. Health care workers' experience with postexposure management of bloodborne pathogen exposures: a pilot study. American journal of infection control 28 (2001): 421-428.
- Behzadmehr R, Balouchi A, Hesaraki M, et al. Prevalence and causes of unreported needle stick injuries among health care workers: a systematic review and meta-analysis. Reviews on environmental health (2021).
- Centers for Disease Control and Prevention (CDC). Workbook for Designing, Implementing, and Evaluating a Sharps Injury Prevention Program. (2008).
- Samargandy SA, Bukhari LM, Samargandy SA, et al. Epidemiology and clinical consequences of occupational exposure to blood and other body fluids in a university hospital in. Saudi Arabia. Saudi medical journal 37 (2016): 783.
- El-Hazmi MM, Al-Majid FM. Needle stick and sharps injuries among health care workers: a 5-year surveillance in a teaching center in Saudi Arabia. Biomedical Research 19 (2008):133-140.
- Saudi Ministry of Health, Key Health Indicators. (2017).
- Alsabaani A, Alqahtani NS, Alqahtani SS, et al. Incidence, Knowledge, Attitude and Practice Toward Needle Stick Injury Among Health Care Workers in Abha City, Saudi Arabia. Frontiers in Public Health 10 (2022): 771190.
- Mahfouz AA, Abdel Moneim I, Khan MY, et al. Injection safety at primary health care level in south-western Saudi Arabia. EMHJ-Eastern. Mediterranean Health Journal 2 (2009): 443-450.
- Yarahmadi R, Dizaji RA, Hossieni AF, et al. The Prevalence of Needle sticks injuries among health care workers at a hospital in Tehran. Iranian Journal of Health, Safety and Environment 23 (2014): 23-29.
- Sabbah I, Sabbah H, Sabbah S, et al. Occupational exposures to blood and body fluids (BBF): assessment of knowledge, attitude and practice among health care workers in general hospitals in Lebanon. Health 5 (2013): 70-78.
- HanafiMI, Mohamed AM, KassemMS, et al. Needle stick injuries among health care workers of University of Alexandria Hospitals. East Mediterr Health J 17 (2011): 26-35.
- Elmiyeh B, Whitaker IS, James MJ, et al. Needle-stick injuries in the National Health Service: a culture of silence. Journal of the Royal Society of Medicine 97 (2004): 326-327.
- Alonazi NA, Alonazi AA, Saeed E, et al. The perception of safety culture among nurses in a tertiary hospital in Central Saudi Arabia. Sudanese journal of paediatrics 16 (2016): 51.
- The private health sector: an operational definition. (2020).