Glioblastoma Multiforme with Long Term Survival
Article Information
Adeeba Zaki1, Nida-e-Zehra2, Yasmin Abdul Rashid1, Adnan Abdul Jabbar1
1Department of Oncology, Aga Khan University Hospital, Karachi, Pakistan
2Clinical sciences, Aga Khan University Hospital Karachi, Pakistan
*Corresponding Author: Adeeba Zaki, Department of Oncology. The Aga Khan University Hospital, National Stadium Road, Karachi 74800, Pakistan.
Received: 17 June 2022; Accepted: 04 July 2022; Published: 12 August 2022
Citation: Adeeba Zaki, Nida-e-Zehra, Yasmin Abdul Rashid, Adnan Abdul Jabbar. Glioblastoma Multiforme with Long Term Survival. Archives of Clinical and Medical Case Reports 6 (2022): 595-598.
Share at FacebookAbstract
Background: GBM is the most common and aggressive primary malignant brain tumor. Despite multimodality approach in the treatment of brain tumor, survival of the patients with GBM remains poor. The median survival of glioblastoma patients is 12 months. However, 35% of the patients survives for more than 3 years and are referred to as long-term survivors. When disease progression occurs 6-month progression-free survival (PFS) is usually lower than 15%.
Case Presentation: A 68-years-old gentleman presented with a space occupying lesion in right frontoparietal region in March 2011, work up showed space (solid enhancing 4.3 x 4.2 x 2.7 cm & cystic component 3.6 x 3.5 x 3 cm). He underwent craniotomy for excision of the lesion, Postoperaticve scan confirmed gross total resection. Histopathology revealed Glioblastoma Multiforme. He received concomitant chemoradiation (60 Gy/30 Fr) with Temozolomide 75mg/m2 followed by monthly temozolomide (day 1-5 q 28 day cycle)., He was continued on monthly temozolomide (from July 2011- July 2015) with imaging Q 3 montly which revealed no residual disease. Patient primary oncologist was changed and since there was no residual disease and no evidence of prolong use of TMZ, it was stopped and was put on surveillance. He remained in remission till September 2017, when he developed recurrent disease. . He underwent right redo craniotomy & excision of SOL in November 2017. Histopathology revealed GBM. He was started on monthly temozolomide q 28day cycle from December 2017 till February 2018, interim scans in Feb shows disease progression he then received Bevacizumab and irrinotecan Q3weekly till April 2018 interim scans shows disease progression at his time his clinical condition also deteriorated and was not a candidate for any further systemic treatment hence advised palliative care and patient expired in May 2018. This is a rare cas
Keywords
Glioblastoma; Temozolomide; Radiotherapy
Article Details
1. Background
Most common and aggressive primary malignant brain tumor is Glioblastoma [1]. Annual incidence is 3.19 per 100,000 in the United States and it increases with age, with the highest between 75 to 84 years of age [2]. Despite multimodality approach in the treatment of brain tumor, survival of the patients with GBM remains poor with a median survival of 3 months if left untreated [3]. The current standard of care for management of glioblastoma is multimodal approach comprising of maximal safe surgical resection, post-operative radiation therapy (RT), and concurrent and adjuvant temozolomide (TMZ) [4,5,6]. Stupp et al shows patient who received concomitant chemoradiation followed by 6 cycle of adjuvant temozolomide 2 year survival was 26.5% vs. 10.4% when compared with radiation alone [7]. Final analysis confirmed the 5 year survival 10% vs. 2% [6]. The optimal management for patients with recurrent or progressive GBM is unclear. In general, treatment for recurrent GBM may involve repeated resection, focal irradiation, and systemic therapies. When disease progression occurs, salvage Chemotherapy is usually unsuccessful, and the 6-month progression-free survival (PFS) is usually lower than 15% [7]. The use of bevacizumab in treatment of recurrent GBM was firstly reported about ten years ago [8]. Studies showed that, patients had more benefit especially after bevacizumab plus irinotecan therapy [9,10]. In these studies PFS was generally obtained in approximately 2-4 months, and OS was 4-6 months. There is however a small percentage of Patients affected by glioblastoma multiforme who survives 3 years or longer [11,12]. Finally there are some exceptional cases, such as the one we are describing in this article.
2. Case Report
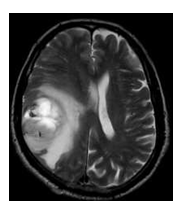
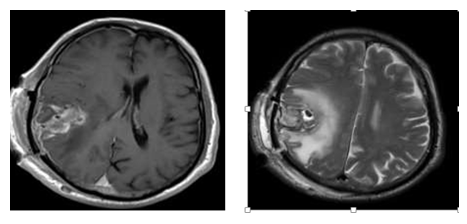
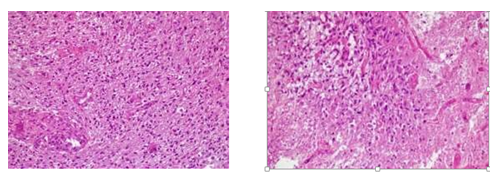
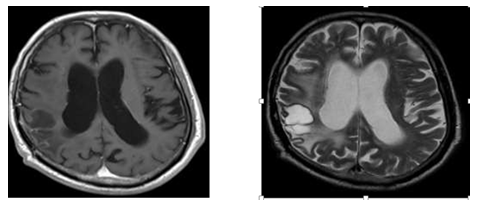
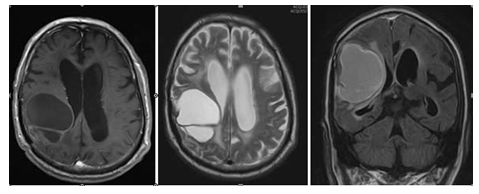
A 68 year old male presented in neurosurgery department with sudden onset of headache & left sided weakness in March 2011, work up revealed space occupying (cystic & solid component) lesion in right frontoparietal region (solid enhancing 4.3 x 4.2 x 2.7 cm & cystic component 3.6 x 3.5 x 3 cm) (Figure 1). On 5th April 2011, he underwent craniotomy + excision of right parietal lesion, the tumor was intraparenchymal and looked like a glioma.(Figure 2). Histopathology revealed Glioblastoma Multiforme (Figure 3). He recieved concomitant chemoradiation (60 Gy, 30 Fr) with Temozolomide 75mg/m2 on days of radiation (5 days/week) followed by monthly temozolomide with initial dose of 150mg/m2 for 5 days every 28 days cycle, followed by increased dose to 200mg/m2 in subsequent cycle. MRI brain was performed every 3 monthly, he was continued on monthly temozolomide (from july 2011- july 2015) with imaging every 3 montly which revealed stable disease (Figure 4).There is no data on survival benefit of such prolong TMZ, hence it was stopped and put on surveillance and was followed with serial MRI brain which revealed no reccurent disease.
He remained in remission (clinically & radiologically) till September 2017, and then developed worsening symptoms, repeat imaging revealed disease progression (Figure 5). He underwent right redo craniotomy & excision of SOL on 2nd November 2017. Histopathology revealed Glioblastoma Grade IV. Re radiation was not possible, so he was rechallanged again with monthly temozolomide (day 1-5) q 28day cycle. He was started on monthly temozolomideq 28day cycle from December 2017 till February 2018; interim scans in Feb showed disease progression he then received Bevacizumab and irrinotecan Q3weekly till April 2018 interim scans shows disease progression at his time his clinical condition also deteriorated and was not a candidate for any further systemic treatment hence advised palliative care and patient expired in May 2018. This is a rare case which reported such a long survival in GBM.
Literature review revealed median survival of patients with GBM is usually 15 months and less than a 10% 5-year survival rate13 despite an aggressive multimodal approach, the median survival time after diagnosis is approximately a year with population-based studies demonstrating even lower median survival rates. Furthermore, the prognosis for recurrent GBM is very poor, and median overall survival (OS) is usually 4-6 months, 5 years survival rate is less than 5% [14-15]. Hence this is a rare case which reported such a long survival in GBM.
3. Discussion
Glioblastoma is a rapidly progressive brain tumor. Despite of multiaggressive treatment with surgical resection followed by concurrent chemoradiation and temozolomide prognosis of patient is still dismal. In recurrent and progressive GBM optimal treatment is unclear usually management includes re-resection, re-radiation if possible, chemotherapy or best supportive care if poor performance status. For re-intervention pre-treatment performance status is most important prognostic factor. Other factors that contribute to benefit from second line therapy are volume of disease, histological grade, relapse free interval and recurrence pattern. Often used chemotherapeutic drug is temozolomide in adjuvant and recurrent cases, benefit is mainly in methylated promotor of MGMT [16]. The pathogonomonic feature of GBM are presence of necrosis and vascular proliferation. VEGF are strongly expressed in GBM tumor cells, overexpression is associated with poor prognosis. Bevacizumab is monoclonal antibody against VEGF used in combination with irrinotecan in recurrent GBM with overall survival benefit of 9 months. A very small number of cases showed greater than 3 years survival [17-18]. In literature it has been noted that long survival for glioblastoma is linked to age, complete surgical resection, good KPS before surgery. Some studies have linked long survival after surgery to the molecular markers like absence of epidermal growth factor receptor gene amplification, presence of MGMT promotor hypermethylation and IDH mutation. There is so far no satisfactory explanation as to why certain cases can be deemed cured.
4. Conclusions
GBM has poor prognosis however we describe a case with prolong outcome. Tumor biology of the patient might be the key to his differential outcome.
References
- Louis, David N, Hiroko Ohgaki, et al. WHO classification of tumors of the central nervous system. Lyon: IARC Press (2007).
- Ostrom QT, Gittleman H, Liao P, et al. statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007-2011. Neuro Oncol 16 (2014): iv1-63.
- Malmström A, Grønberg BH, Marosi C, et al. Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. The lancet oncology 13 (2012): 916-926.
- Taphoorn, Martin JB, Claassens L, et al. An international validation study of the EORTC brain cancer module (EORTC QLQ-BN20) for assessing health-related quality of life and symptoms in brain cancer patients. Eur J Cancer 46 (2010): 1033-1040.
- Chinot OL, Wick W, Mason W, et Bevacizumab plus radiotherapy temozolomide for newly diagnosed glioblastoma. New England Journal of Medicine 370 (2014): 709-722.
- Stupp R, Hegi ME, Mason WP, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10 (2009): 459-466.
- Wong ET, Hess KR, Gleason MJ, et al. Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. J Clin Oncol 17 (1999): 2572e2578.
- Stark Vance V. Bevacizumab (AvastinR) and CPT-11 (CamptosarR) in the treatment of relapsed malignant glioma. Neurooncol 7 (2005): 369.
- Ali SA, McHayleh WM, Ahmad A, et al. Bevacizumab and irinotecan therapy in glioblastoma multiforme: A series of 13 cases. J Neurosurg 109 (2008): 268e272.
- Norden AD, Young GS, Setayesh K, et al. Bevacizumab for recurrent malignant gliomas: Efficacy, toxicity, and patterns of recurrence. Neurology 70 (2008): 779e787.
- Salvati M, Cervoni L, Artico M, et al. Gagliardi, Long-term survival in patients with supratentorial glioblastoma, J. Neurooncol 36 (1998): 61-64.
- Smoll NR, Schaller K, Gautschi OP. Long-term survival of patients with glioblastoma multiforme (GBM), J. Clin. Neurosci 20 (2013): 670-675.
- Buckner JC. Factors influencing survival in high-grade gliomas. Semin Oncol 30 (2003): 10e14.
- Stark Vance V. Bevacizumab (AvastinR) and CPT-11 (CamptosarR) in the treatment of relapsed malignant glioma. Neurooncol 7(2005): 369.
- Ammirati M, Galicich JH, Arbit E, et al. Reoperation in the treatment of recurrent intracranial malignant gliomas. Neurosurgery 21 (1987): 607-614.
- Puzzilli F, Ruggeri A, Mastronardi L, et al. Long-term survival in cerebral glioblastoma. Case report and critical review of the literature. Tumori Journal 84 (1998): 69-74.
- Yoshida T, Kawano N, Oka H, et al. Clinical Cure of Glioblastoma. Neurologia medico-chirurgica 40 (2000): 224-229.
- Krex D, Klink B, Hartmann C, et al. Long-term survival with glioblastoma multiforme. Brain 130 (2007): 2596-2606.