Gall Bladder Duplication: An Interesting Report of Laparoscopic Cholecystectomy performed on Two Cases of Gall Bladder Duplication over a Period of One Week
Article Information
Mourad Halfaoui1, Fahad Aurif1*, Abdullah Salman Dalol1, Murad Alahmad1, Fathimathul Zumara Anwar1, Tamer Abdelhafez Elbakry1
1Al Wakra Hospital, General Surgery, Hamad Medical Corporation, Al Wakrah, Qatar
*Corresponding Author: Fahad Aurif, Al Wakra Hospital, General Surgery, Hamad Medical Corporation, Al Wakrah, Qatar.
Received: 03 March 2023; Accepted: 14 March 2023; Published: 28 March 2023
Citation: Mourad Halfaoui, Fahad Aurif, Abdullah Salman Dalol, Murad Alahmad, Fathimathul Zumara Anwar, Tamer Abdelhafez Elbakry. Gall Bladder Duplication: An Interesting Report of Laparoscopic Cholecystectomy performed on Two Cases of Gall Bladder Duplication over a Period of One Week. Archives of Clinical and Medical Case Reports. 7 (2023): 136-140.
Share at FacebookAbstract
Gall Bladder Duplication: An interesting report of laparoscopic cholecystectomy performed on two cases of Gall Bladder Duplication over one week.
Introduction: Duplication of the gall bladder is very rare. Due to the unusual anatomy, laparoscopic cholecystectomy can be challenging.
Case Report: Two routine cases of symptomatic gallstones presented to the clinic for elective laparoscopic cholecystectomy in 1 week, the first was a 37-year-old male, and the other was a 35-year-old female patient. Ultrasound of the abdomen in the male patient showed a partially distended gall bladder with multiple stones impacted in the neck, focal wall thickening in the fundal region with surrounding collaterals, and diffuse bilobar periportal thickening. An MRCP revealed an extraluminal gall bladder stone superoanterior to neck region narrow thin cleft of fluid around it, representing congenital true or acquired pseudo diverticulum Ultrasound of the female patient revealed a folded gall bladder with multiple stones and a normal CBD. Laparoscopic cholecystectomy was performed successfully in both patients.
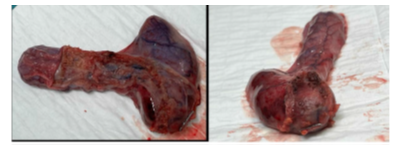
Discussion: In the male patient inspection of the gall bladder revealed a diverticulum at the region of the Hartman, the specimen had a single artery and a single cystic duct, the wall of the specimen was thick containing a large stone whilst the diverticulum was thin-walled and had no stones. The female patient inspection revealed duplicated gall bladder with two fundi, each containing stones, a common Hartman’s pouch, and a single cystic duct and single artery.
Conclusion: Double gall bladder is a very rare congenital abnormality. It is prudent to pay extensive attention to the ductal and vascular anatomy. Laparoscopic cholecystectomy with intraoperative Cholangiogram is preferred in difficult cases.
Keywords
Cholecystitis; Cholelithiasis; Gall Bladder Duplication; Laparoscopic Cholecystectomy
Article Details
1. Introduction
Duplication of the gall bladder is a very rare congenital abnormality that occurs in around 1 in 4000 births. Particular consideration should be given to the ductal and arterial anatomy of the biliary system since such malformations are highly related to increased complexities during surgery [1].
2. Case Report
Two cases of Gall stones disease presented to the Clinic and were booked for elective laparoscopic cholecystectomy. The first was a 37-year-old heavy-smoker male known case of coronary artery disease, who was evaluated in the clinic for recurrent biliary colic. The patient had an episode of right upper quadrant pain eight months back for which he was managed conservatively. Ultrasound of the abdomen at the time revealed a gall bladder stone of about 0.5 cm impacted at the neck. Repeat ultrasound after 4 months showed focal wall thickening in the fundal region, diffuse bilobar periportal thickening representing chronic inflammation, also a gall bladder stone about 1 cm impacted in the neck. An MRCP with contrast revealed an extraluminal gall bladder stone superoanterior to the neck region with a narrow cleft of fluid around it without signs of acute cholecystitis. There was a stone about 1.4 x 1.2 cm in the congenital true or acquired pseudo diverticulum, arising from chronic pressure from the GB neck region. His present medications include aspirin, bisoprolol, glyceryl trinitrate, lisinopril, and rosuvastatin. After cardiac evaluation, the patient was scheduled for elective surgery. A laparoscopic cholecystectomy was performed and the patient had an uneventful recovery. The second case involved a 35-year-old lady with symptomatic gall stones, she had no comorbidities. Ultrasound of the abdomen revealed folded gall bladder with multiple stones, the largest measuring 0.77 cm. She had a normal CBD. She proceeded to laparoscopic cholecystectomy. A duplication of the gall bladder was seen intraoperatively, it had two fundus containing separate stones, a common Hartmann's pouch, one cystic duct, and a posterior cystic artery. The surgery was completed, and the patient had an uneventful recovery.
3. Discussion
Duplication of the gall bladder is a very rare congenital abnormality that occurs in around 1 in 4000 births [1]. The earliest description of Double accessory Gallbladder dates to 31 BC, in the sacrificial victim of Emperor Augustus [2]. In 1911 Sherren documented the first double accessory gall bladder in a living human [3]. B. Senecail et al studied ultrasound of gallbladder surgeries performed on 1823 patients and discovered morphological abnormalities in 33 %, and just about 3 % of the gallbladders had true duplication [4]. No literature is available about the Epidemiological distribution of duplicated gallbladders. The incidence of the double gallbladder in adults during radiology is around 0.03% and at postmortem is 0.02% [5]. It is vital to consider the ductal and arterial anatomy of the biliary system preoperatively, as such malformations could cause significant morbidity [1]. Magnetic Resonance Cholangiopancreatography is the imaging modality that is best used to assess the biliary tree [6]. We present two cases of diverticulum of the gall bladder operated on, within 1 week, the first was possibly due to pressure from an impacted stone in the neck, and the second case had two separate fundus, with separate stones and common Hartman’s pouch, common cystic duct, and a posterior cystic artery. Laparoscopic cholecystectomy was completed successfully in both cases. The operation was performed using standard 4 port placement in both cases. Intraoperatively there were dense adhesions of the omentum to the Gall bladder in both cases, which were released carefully, the gall bladder was grasped at the fundus and retracted caudally to the right shoulder. The diverticulum was used as additional leverage to retract the gall bladder in both cases, careful dissection was used to define the hepatocytic triangle, a single cystic artery, and the duct was identified and clipped safely, gall bladder was safely dissected off the gall bladder fossa. Inspection of the gall bladder revealed a diverticulum at the region of the Hartman in the male patient and at the fundus in the female patient. The specimen had a single artery and a single cystic duct. The wall of the specimen in the male patient was thick and contained a large stone whilst the diverticulum was thin-walled and had no stones. The female patient had separate stones, one in the fundus and one in the Diverticulum. Both patients did well postoperatively and were discharged as day cases. The histopathology report confirmed the diagnosis of chronic cholecystitis with focal intestinal metaplasia in the male patient and chronic cholecystitis in the female patient.
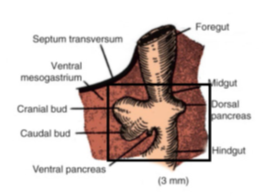
Chronic cholecystitis with focal intestinal metaplasia occurs due to friction of stones along the gall bladder wall, triggering an inflammatory response and resulting in gastric and intestinal metaplasia. Focal intestinal metaplasia is a risk factor for carcinoma of the gall bladder [7]. It is prudent to discern the embryology of the gall bladder to understand the pathogenesis behind a gall bladder diverticulum. During the 4th week of intrauterine life, a hepatic diverticulum arises from the ventral wall of the primitive midgut, this later divides into a cranial and a caudal bud, the cranial bud develops into the liver and the extrahepatic bile ducts, the caudal bud is further divided into the superior and an inferior bud. The superior bud develops into the gall bladder and the cystic duct [8], and the inferior bud gives rise to the pancreas [9,10]. The embryological explanation for the Duplication of gall bladder occurs during the fifth to sixth week. It arises due to improper differentiation or increased division of embryonic organs [11]. Embryonic organs like accessory vesicles and supernumerary buds that arise from the hepatic antrum persist and do not regress, also two individual cystic primordia are formed from the bile duct due to the bifurcation of cystic and accessory cystic primordium [5].
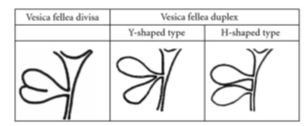
Duplication of the gall bladder is differentiated according to Boyden’s classification [14] as shown in figure 5:
- Vesica fellea divisa (double gall bladder with a common neck)
- Vesica fellea duplex (double gall bladder with two cystic ducts)
- Y-shaped (two cystic ducts join before uniting with the common bile duct)
- H-shaped (two cystic ducts enter individually into the biliary tree)
A newer differentiation of gall bladder duplication is the Harlaftis classification [15] as shown in figure 6:
- Type 1 – split primordial group (one cystic duct). (i) Septated (ii). V-shaped. (iii) Y shaped
- Type 2 – two individual cystic ducts
As shown in figure 6, type 1 gallbladders have a single cystic duct that drains into the common bile duct. This is further divided into v-shaped and Y-shaped gallbladders. In the former type, the gall bladders unite at the level of the neck and drain into a common cystic duct, whilst, in the latter, the gall bladders have separate cystic ducts, which then join into a common cystic duct which then drain into the gall bladder [16]. Cholecystectomy in the Y type is challenging and would require careful imaging or intraoperative cholangiograms to avoid common bile duct injuries [17]. The type 2 gall bladder duplications have accessory gall bladders with separate cystic ducts draining separately into the common bile duct, this is classically described by the H type and is described as the most common type after a review of 148 cases as described by Kawanishi M [18]. In the Trabecular type of Gall bladder duplication, the accessory duct connects to the RHD or the LHD as shown in figure 6 [15]. Carcinoma of the accessory gall bladder is documented in two studies [19,20]. Gall bladder duplication that does not fit into type 1 or type 2 is classified as type 3. Two studies describe triple gall bladders, Roders et al describe a triple gall bladder with two gall bladders removed, HPE revealed cholecystitis in one of the Gb and papillary adenocarcinoma in the other, and the third GB was found during post-operative imaging via T tube cholangiogram [21]. Schroeder et al also document a triple gall bladder of which two were identified during preoperative imaging, and the third one was seen preoperatively [22]. Both our cases were of Vesica fellea divisa as of Boyden’s classification or type 1, V-shaped GBD as per Harlafit's classification.GB duplication is also described in scimitar syndrome [23] and gastrointestinal atresia [24]. Patients with gall bladder duplication do not have any distinctive clinical presentation. They are usually incidental findings during imaging or autopsy or could be found intraoperatively [25]. In gall bladder duplication, even if only one of the gall bladders is involved with cholecystitis, it is prudent to remove both gall bladders [26]. Likewise, a duplicate gall bladder if not removed increases the chances of recurrent cholecystitis regardless of prior cholecystectomy [27]. GBD can be missed during initial imaging and most cases are encountered as an intraoperative finding [26]. MRCPor CT Cholangiography is the imaging of choice in suspected duplication of the gall bladder [28]. Intraoperative Cholangiogram or laparoscopic ultrasound may be used in intraoperative diagnosis with challenging anatomy [29]. Thus, patients with this rare congenital anomaly can be either asymptomatic or may present with gall bladder pathologies such as cholelithiasis, cholecystitis, cholangitis, and adenocarcinoma. In asymptomatic patients with GBD, surgery is not indicated and there is no evidence of an increased risk of cholecystitis [30].
4. Conclusion
In conclusion, duplication of the gall bladder is a rare congenital anomaly with an increased risk of complexities during laparoscopic cholecystectomy due to the altered anatomy of the biliary tree. It is vital to understand the anatomy of GBD in challenging cases. Intraoperative cholangiogram could be used safely in demanding circumstances.
References
- Pillay Y. Gallbladder duplication. Int J Surg Case Rep 11 (2015): 18-20.
- Vezakis A, Pantiora E, Giannoulopoulos D, et al. A Duplicated Gallbladder in a Patient Presenting with Acute Cholangitis. A Case Study and a Literature Review, Annals of Hepatology 18 (2019): 240-245.
- Sherren J. IX. A Double Gall-bladder Removed by Operation.Ann Surg 54 (1911): 204-205.
- Senecail B, Texier F, Kergastel I, et al. Anatomic variability and congenital anomalies of the gallbladder: an ultrasonographic study of 1823 patients. Morphologie: Bulletin de L'association des Anatomistes 84 (2000): 35-39.
- Subasinghe D, Guruge MH, Sivaganesh S. Double gallbladder-intraoperative finding at laparoscopic cholecystectomy: A literature review. SAGE Open Med Case Rep 10 (2022): 2050313X211068687.
- Boukoucha M, Dhieb F, Khelifa RB, et al. Cholecystitis on gallbladder duplication: A case report and literature review. Int J Surg Case Rep 72 (2020): 406-410.
- Fernandes JEV, Franco MIF, Suzuki RK, et al. Intestinal metaplasia in gallbladders: prevalence study: Sao Paulo Med J 126 (2008).
- Ando H. Embryology of the biliary tract. Dig Surg 27 (2010): 87-89.
- Bremer JL. Description of a 4 mm human embryo. Am J Anat 5 (1906): 459-480.
- Kanagasuntheram R. Some observations on the development of the human duodenum. J Anat 94 (1960): 231-240.
- Paraskevas GK, Raikos A, Ioannidis O, et al. Duplicated gallbladder: surgical application and review of the literature. Ital J Anat Embryol 116 (2011): 61-66.
- Saldinger PF, Bellorin-Marin OE. Chapter 106 - Anatomy, Embryology, Anomalies, and Physiology of the Biliary Tract, Editor(s): Charles J. Yeo, Shackelford's Surgery of the Alimentary Tract, 2 Volume Set (Eighth Edition), Elsevier (2019): 1249-1266.
- Maloney C, Huston J. Normal Biliary Anatomy and Pathophysiology of Gallstones. In: Eachempati, S., Reed, II, R. (eds) Acute Cholecystitis. Springer, Cham (2015).
- Maloney C, Huston J. Normal Biliary Anatomy and Pathophysiology of Gallstones. In: Eachempati, S., Reed, II, R. (eds) Acute Cholecystitis. Springer, Cham (2015).
- Cozacov Y, Subhas G, Jacobs M, et al. Total laparoscopic removal of the accessory gallbladder: A case report and review of the literature. World J Gastrointest Surg 7 (2015): 398-402.
- Ingegno AP, D’albora JB. Double gallbladder; roentgenographic demonstration of a case of the Y type; classification of the accessory gallbladder.Am J Roentgenol Radium Ther 61 (1949): 671-676.
- Guajardo-Salinas GE, Martinez-Ugarte ML, Abourjaily G. The use of intraoperative cholangiogram during laparoscopic double cholecystectomy..J Surg Case Rep (2010): 5.
- Kawanishi M, Kuwada Y, Mitsuoka Y, et al. A case of the double gallbladder with adenocarcinoma arising from the left hepatic duct: a case report and review of the literature.Gastroenterol Res Pract 2010 (2010).
- Kin Y, Yamaguchi A, Isogai M, et al. Duplication of the gallbladder with advanced adenocarcinoma: diagnostic value of MRI and angiography 43 (1996): 405-408.
- Raymond SW, Thrift CB. Carcinoma of a duplicated gall bladder.Ill Med J 110 (1956): 239-240.
- Roeder WJ, Mersheimer WL, Kazarian KK. Triplication of the gallbladder with cholecystitis, cholelithiasis, and papillary adenocarcinoma.Am J Surg 121 (1971): 746-748.
- Schroeder C, Draper KR. Laparoscopic cholecystectomy for triple gallbladder.Surg Endosc 17 (2003): 1322.
- Ormeci T, Gunluoglu MZ. Scimitar syndrome associated with gallbladder duplication. Clin Imaging 38 (2014): 346-349.
- Gupta R, Gupta S, Sharma P, et al. Gallbladder duplication associated with gastrointestinal atresia. J Neonatal Surg 5 (2016): 14.
- Alsharedah AH, Alotaibi SM, Khan BF, et al. Laparoscopic Management of Gallbladder Duplication: A Case Report. Cureus 12 (2020): e10675.
- Perez AR, Magcase M, Perez MEC. Gallbladder duplication complicated by cholecystitis and unsuspected choledocholithiasis: A case report and review of the literature. Int J Surg Case Rep 87 (2021): 106433.
- Pera SJ, Huh N, Orcutt ST. Duplicate gallbladder: A case report of a patient with cholecystitis after cholecystectomy. Int J Surg Case Rep 65 (2019): 156-160.
- Vezakis A, Pantiora E, Giannoulopoulos D, et al. A Duplicated Gallbladder in a Patient Presenting with Acute Cholangitis. A Case Study and a Literature Review, Annals of Hepatology 18 (2019): 240-245.
- Dili A, Bertrand C. Laparoscopic ultrasonography as an alternative to intraoperative cholangiography during laparoscopic cholecystectomy. World J Gastroenterol 23 (2017): 5438-5450.
- Apolo Romero EX, Gálvez Salazar PF, Estrada Chandi JA, et al. Gallbladder duplication and cholecystitis. J Surg Case Rep 2018 (2018): rjy158.