Financial Toxicity and Strain among Veteran and Civilian Men with Prostate Cancer
Article Information
Adam B. Sumlin1, PhD, Ali Houjaij2, MD, Oussama M. Darwish2, MD, Susan Camacho1, BA, Adrienne Groman3, MS, Zahra Fayazi1 DVM, PhD
1 Department of Cell Stress Biology, Roswell Park Comprehensive Cancer Center, Elm and Carlton St, Buffalo, NY 14263
2 Department of Surgery, Division of Urology, WNY Healthcare System, Buffalo VA Hospital, 3495 Bailey Ave, Buffalo, NY 14215
3 Department of Biostatistics and Bioinformatics, Roswell Park Comprehensive Cancer Center, Elm and Carlton St, Buffalo, NY 14263
*Corresponding author: Adam B. Sumlin, PhD, Department of Cell Stress Biology, Roswell Park Comprehensive Cancer Center, Elm and Carlton St, Buffalo, NY 14263, USA
Received: 30 March 2023; Accepted: 10 April 2023; Published: 09 May 2023
Citation: Adam B. Sumlin, PhD, Ali Houjaij, MD, Oussama M. Darwish, MD, Susan Camacho1, BA, Adrienne Groman, MS, Zahra Fayazi DVM, PhD. Financial Toxicity and Strain among Veteran and Civilian Men with Prostate Cancer. Archives of Clinical and Biomedical Research. 7 (2023): 301-305.
Share at FacebookAbstract
Purpose: The goal of this study was to examine financial toxicity and strain among Veterans and civilians in two different healthcare facilities. This study was based for the concerns for the rising cost of cancer care which can lead to societal financial toxicity. Societal financial toxicity is discussed at many levels of healthcare policy.
Method: A questionnaire was administered to 115 participants (11 Veterans and 104 civilians) for Veteran and civilian men who have been diagnosed with prostate cancer and who may have experienced financial difficulty with treatment or diagnosis. Descriptive statistical analyses (as appropriate: n, percent, mean, median, min and max) will be used to summarize participant characteristics. Factors influencing survival such as PCa diagnosis, treatment, financial toxicity, and Quality of Life (QoL) measures will be examined using a logistic regression model.
Results: Men will sustain financial burdens from treatment of prostate cancer, medications, and side effects. Men who have less socioeconomic reserves and poorer ability to interact with the American healthcare system will suffer unreasonably. These men are more likely to be African Americans or Veterans. Therefore, locating the extent of financial burden and developing new interventions to alleviate financial toxicity and thereby financial stress will impact men with socioeconomic disadvantages and reduce disparity.
Conclusion: There is a difference among healthcare systems that translate to later diagnosis and more treatments with the outcome not being as favorable to some. Greater cost and intensity of treatment can translate into a greater financial burden and strain, which will impact those with less insurance, financial reserves, and Veteran men specifically who suffer from PCa.
Keywords
Prostate cancer, financial toxicity, Veterans, civilians, quality of life
Prostate cancer articles, financial toxicity articles, Veterans articles, civilians articles, quality of life articles
Article Details
Introduction:
Prostate Cancer (PCa) is the leading cause of non-skin cancer among males in the United States across all races [1]. Men in the United States have 14% lifetime chance of being diagnosed with PCa and a 3% chance of dying from the disease within 5 to 7 years of diagnosis once they reach age 65 or older [2]. Race is both a risk factor and a prognostic factor for PCa diagnosis and death [3]. Cancer has become a major public health quandary in the United States and throughout the world [4].
Multiple factors (clinical, socioeconomic, and pathologic) have been shown to account for 15% of the increased risk of PCa mortality in men [5]. Complexities that exist among insurance coverage, Medicare reimbursement policies, increase in co-payments for medication, and the difference in the availability of financial assistance from pharmaceutical companies for new agents pose a challenging financial toxicity for the treatment of advanced stage PCa among all parties, but especially the poor [6].
Greater cost and intensity of treatment translates to greater financial toxicity and stress that may impact more individuals with lower insurance coverage, financial reserves, and medical system intricacy [7]. More non-treatment resources may be required to support men, in general, and Veterans, specifically, who suffer from PCa, but survivorship deficits require better and data-driven delineation for precise intervention.
Additionally, economic burden is incurred by the healthcare system in the ongoing treatment of PCa-related problems and survivorship issues, which require out-of-pocket payments and lost productivity, that impact quality of life (QoL). PCa survivors are known to pay more out-of-pocket expenses for the care of their disease than those who may have other chronic diseases which increases their financial burden and/or stress [8]. The financial stress may be associated with less perceived QoL, time lapse in treatment of the disease, or lack of medication [9]. Some other forms of financial toxicity and/or strain may come from unreimbursed costs of medication and drugs, insurance co-pays, travel for treatment or hospital visits. Dealing with cost of care may be affected by one’s socioeconomic status, income, and amount of savings. Consequently, PCa treatment costs may cause withdrawal from bank accounts, selling of homes and other assets, skipping of treatments, borrowing from family members, and depleting of retirement plans. Financial strain may impact the patient, and/or family. A survey that was administrated nationally to patients with cancer reported that approximately 25% of the insured lost most of their savings dealing with cancer, and 33% could not pay the cancer care bills [10].
Methods:
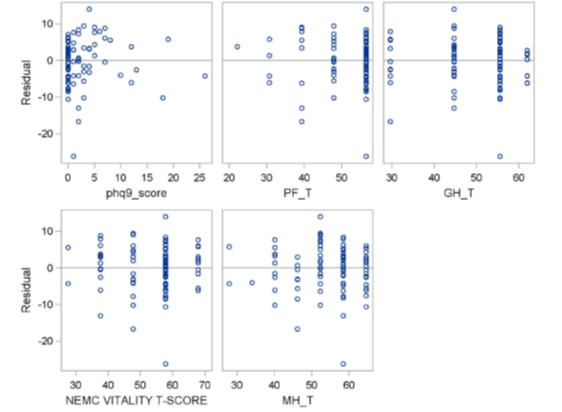
Financial toxicity was measured by the Comprehensive Score for financial Toxicity (COST) measure. The higher the score, the better the Financial Well-Being. The Expanded Prostate Cancer Index Composite Short Form (EPIC-26) was used to measure quality of life. The higher the score, the better the QOL, 0 (worst) to 100 (best). The PHQ-9* Questionnaire for Depression Scoring was used to measure mental health. The higher the score, the higher the severity of depression. Patient characteristics, QOL and COST were summarized with mean, std and range for numeric variables and frequencies and relative frequencies for categorical variables. Associations between the COST and QOL and demographic factors were assessed using multivariable analyses with COST as the dependent variable and the QOL and demographic factors as potential explanatory variables. Backwards elimination was used to find significant predictors. Variables considered were, PHQ-9 Depression Scoring (phq9_score), Physical functioning T-score (PF_T), epic26_hormonal, epic26_bowel, epic26_sexual, epic26_urinary_obs, epic26_urinary_inc, Role limitation physical (RP_T), Pain T-score (BP_T), General health T-score (GH_T), Vitality T-score (VT_T), Role limitation emotional T-score (RE_T), Social functioning T-score (SF_T), and Mental health T-score (MH_T). The significant predictors were PHQ-9 Depression Scoring (phq9_score), Physical functioning T-score (PF_T), General health T-score (GH_T), Vitality T-score (VT_T), and Mental health T-score (MH_T) [11].
For every one unit increase in the Physical functioning T-score (PF_T) the predicted Financial Toxicity Score decreases by 0.22 (p-value=0.0264). For every one unit increase in the General health T-score (GH_T) the predicted Financial Toxicity Score increases by 0.24 (p-value= 0.0146). For every one unit increase in the Vitality T-score (VT_T) the predicted Financial Toxicity Score increases by 0.20 (p-value=0.0331). For every one unit increase in the Mental health T-score (MH_T) the predicted Financial Toxicity Score increases by 0.30 (p-value=0.0146).
Initially we wanted to recruit 300 participants from the Urology, Radiation Oncology, or Medical Oncology clinics, of RPCCC, and VA which will consist of 150 Veteran and 150 civilian men to provide a comparison cohort. The number of participants may vary from facility to facility, but the overall goal is to recruit 300 divided evenly between the two facilities. At present we have recruited 115 men total, of which 11 are Veterans and 104 are civilians.
An exploratory study will collect PCa treatments received quality of life, and financial toxicity and stress. Total cost of illness will be compared among healthcare systems and between Veterans and civilians for ongoing treatment of PCa related problems and survivorship issues, with focus on out- of- pocket expenses, private health insurance, QoL, taking into consideration the difference in the cohorts’ sample size.
Result:
Approach to suitable, high-quality, patient-centered cancer care is of critical importance to patients with cancer and their families. Nevertheless, patients should have access to a provider network that has experienced oncology experts and multidisciplinary cancer centers. However, there are challenges to accessing high quality cancer care, which leads to future studies and innovative services.
Preliminary data demonstrated in this early trial asked the subjects, have you or your family had to make any other kinds of financial sacrifices because of their cancer, treatments, or lasting effects from the treatments. The data represented from this group is demonstrated in (Table 1), which relates to the questionnaire on have you ever worried about having to pay large medical bills related to cancer.
Model: MODEL1
Dependent Variable: Financial_Toxicity_Score
|
Number of Observations Read |
115 |
|
Number of Observations Used |
92 |
|
Number of Observations with Missing Values |
23 |
Backward Elimination: Step 0
All Variables Entered: R-Square = 0.5452 and C(p) = 15.0000
The model is not of full rank. A subset of the model which is of full rank is chosen.
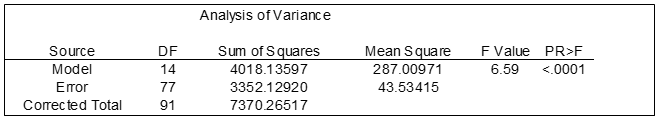
Table 1: Financial toxicity hardship by Variance
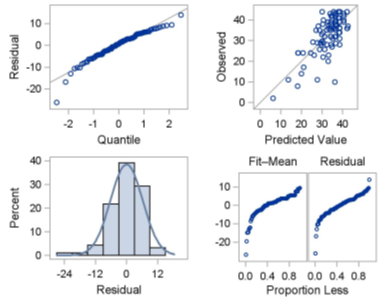
Both figures suggest that a financial toxicity may exist between the variances although more subjects are needed to confirm results. The predicted value suggest that all variances should fall on the line. This test whether a regression line is a significant upgrade over the mean as a prediction tool.
The preliminary work was designed to show the need for pharmaceutical and insurance mandates to eliminate the high cost of healthcare along with treatment for PCa for a better QoL in patients who suffer from this disease. The findings from this study may generate the ability for clinical relevance by formulating treatments for PCa patients that will meet their economic ability and reduce their financial toxicity and/or strain leading to a better QoL and continued knowledge growth that may lead to a healthier lifestyle. One of the pitfalls of this type of study is that one cannot reach all PCa patients in a timely manner and may miss those who have passed away from other illnesses that were unrelated to PCa. At present we were only able to receive 11 surveys from the 32 Veteran men who were consented to take part in this study. Another drawback could be the higher PCa incidence among AA men are not fully understood and have received inadequate attention. It is also critical to understand the potential psychological and social factors that may be additional underlying sources that could generate or intensify these disparities. Socioeconomic status is the societal standing of an individual or group, use to measure education, income, wealth and occupation, multiple groupings of these factors.
Discussion:
Notwithstanding policies may be introduced to reduce out-of-pocket costs for Veteran patients with prostate cancer, however, patients have reported significant financial toxicity which we have shown in the data collected. With the passing of the Pact Act for Veterans, Veterans who meet the certain service criteria more education is needed to assure that their financial toxicity will be reduced. Prostate cancer is one of the 20 presumptive conditions that was added to this legislative pact for their healthcare and benefits. With the continued undertaking for value-based care centered data on patient care delivery, identifying persistent financial toxicity for defenseless cancer patients is important data as we try and improve the infrastructure to impact quality of life and healthcare delivery for this population.
Conclusion:
Financial toxicity is increasingly recognized as a serious prospective concern of prostate cancer diagnosis and treatment. Focusing on prostate cancer, next steps should include potential studies using tools to assess the magnitude of financial distress and identify specific prognosticators of risk. These efforts would assist the clinicians with prominent information to deliver to their patients on how to address financial toxicity and make a better decision on their treatment or care.
Our efforts accentuate educating patients to assist them in understanding the costs of their medical care and linking patients with patient advocates to facilitate them in obtaining supplemental support and resources to cover out-of-pocket expenses. Patient advocates will provide Veterans with information and tools to improve their health and make better decisions on their QOL. They would also provide information on the healthcare services provided by the VA organization. The most important function of the patient advocate is to act as a liaison between the Veteran and the treatment team to effectively resolve problems.
There is a difference in racial balance among healthcare systems that translate to later diagnosis and more treatments with the outcome not being as favorable to some. Greater cost and intensity of treatment can translate into a greater financial toxicity and strain, which will impact those with less insurance, financial reserves, and veteran men specifically who suffer from PCa. This cross-sectional study was intended to acquire data to characterize financial toxicity to enable future longitudinal studies (long term goal).
Acknowledgement:
Biostatistics services were provided by the Biostatistics and Statistical Genomics Shared Resource at the Roswell Park Comprehensive Cancer Center which is supported in part by the NCI Cancer Center Support Grant 5P30 CA016056.
Statement and Declarations:
Adam Sumlin declares he has no conflict of interest. Ali Houjaij declares he has no conflict of interest. Oussama Darwish declares he has no conflict of interest. Susan Camacho declares she has no conflict of interest. Adrienne Groman declares she has no conflict of interest. Zahra Fayazi declares she has no conflict of interest.
References
- Hoffman RM, Gilliland FD, Eley JW, Harlan LC, Stephenson RA, Stanford JL, et al. Racial and ethnic differences in advanced-stage prostate cancer: the Prostate Cancer Outcomes Study. J Natl Cancer Inst. 2001; 93(5): 388-395.
- Aetna. Clinical policy bulletin: Prostrate cancer screening (No. 0521). . Secondary Clinical policy bulletin: Prostrate cancer screening (No 0521) 2002.
- Brawley OW. Prostate cancer epidemiology in the United States. World J Urol. 2012; 30(2): 195-200.
- Smith RA, Cokkinides V, Brooks D, Saslow D, Brawley OW. Cancer screening in the United States, 2010: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin. 2010; 60(2): 99-119.
- Oliver JS. Attitudes and beliefs about prostate cancer and screening among rural African American men. J Cult Divers. 2007; 14(2): 74-80.
- Chang P. Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP): Development and Validation of a Practical Health-Related Quality of Life Instrument for Use in the Routine Clinical Care of Prostate Cancer Patients. JUrol. 2011;186(3).
- Fletcher CN LF. Structural Influences on the Relationship between Objective and Subjective Indicators of Economic Well-Being. . Social Indicators Research 1985; 16: 333-345.
- Bachner YG, O'Rourke N, Carmel S. Psychometric properties of a modified version of the Caregiver Reaction Assessment Scale measuring caregiving and post-caregiving reactions of caregivers of cancer patients. J Palliat Care. 2007; 23(2): 80-86.
- Hanratty B, Holland P, Jacoby A, Whitehead M. Financial stress and strain associated with terminal cancer--a review of the evidence. Palliat Med. 2007; 21(7): 595-607.
- USA Today KFF, Harvard School of Pubic Health. National survey of households affected by cancer. USA Today KFF, 2006.
- Kroenke K. The PHQ-9. J Gen Intern Med. 2001; 16(9): 606-613.
- Zafar, S.Y., et al., Population-based assessment of cancer survivors' financial burden and quality of life: a prospective cohort study. J Oncol Pract, 2015. 11(2): p. 145-50.
- Fenn, K.M., et al., Impact of financial burden of cancer on survivors' quality of life. J Oncol Pract, 2014. 10(5): p. 332-338.
- Freeman, V.L., et al., Racial differences in survival among men with prostate cancer and comorbidity at time of diagnosis. Am J Public Health, 2004. 94(5): p. 803-808.
- MARVIN DELGADO-GUAY, et al., Financial Distress and Its Associations With Physical and Emotional Symptoms and Quality of Life Among Advanced Cancer Patients. The oncologist, 2015. 20(9): p. 1092-8.
- Madden, J., The problem of distress in patients with cancer: more effective assessment. Clin J Oncol Nurs, 2006. 10(5): p. 615-619.
- Agency for Health Care Research and Quality (AHRQ): Sample Design of the 1997 Medical Expenditure Panel Survey Household Component.
- Miller, D.C., et al., Long-term outcomes among localized prostate cancer survivors: health-related quality-of-life changes after radical prostatectomy, external radiation, and brachytherapy. J Clin Oncol, 2005. 23(12): p. 2772-80.
- Sanda, M.G., et al., Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med, 2008. 358(12): p. 1250-1261.
- Jung, O.S., et al., Out-of-pocket expenses and treatment choice for men with prostate cancer. Urology, 2012. 80(6): p. 1252-1257.
- Carpenter, W.R., et al., Racial differences in trust and regular source of patient care and the implications for prostate cancer screening use. Cancer, 2009. 115(21): p. 5048-5059.
- Ellis, S.D., et al., Receipt of National Comprehensive Cancer Network guideline-concordant prostate cancer care among African American and Caucasian American men in North Carolina. Cancer, 2013. 119(12): p. 2282-2290.
- Song, L., et al., Who makes the decision regarding the treatment of clinically localized prostate cancer--the patient or physician?: results from a population-based study. Cancer, 2013. 119(2): p. 421-428.
- Defense, D.o., Evaluation of the TRICARE Program—Access, Cost, and Quality. Fiscal Year 2014 Report to Congress (March 2014), 2014.
- Landwehr, M.S., et al., The cost of cancer: a retrospective analysis of the financial impact of cancer on young adults. Cancer Med, 2016. 5(5): p. 863-870.