Equine Sialolithiasis of the Distal Parotid Duct. Retrospective Study on 4 Cases
Article Information
Diakakis N1*, Karadima V2
1Associate Professor, Equine Unit, Companion Animal Clinic, School of Veterinary Medicine, Aristotle University of Thessaloniki, Greece
2Practitioner, Equine Unit, Companion Animal Clinic, School of Veterinary Medicine, Aristotle University of Thessaloniki, Greece
*Corresponding Author: Nikolaos Diakakis, School of Veterinary Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki, 11 St. Voutyra str., 54627, Thessaloniki, Greece
Received: 14 February 2021; Accepted: 22 February 2020; Published: 08 March 2021
Citation: Diakakis N, Karadima V. Equine Sialolithiasis of the Distal Parotid Duct. Retrospective Study on 4 Cases. Archives of Veterinary Science and Medicine 4 (2021): 13-23.
Share at FacebookAbstract
Sialolithiasis is an infrequently encountered condition in equids, although it occurs more frequently in equine species than other domestic species. Sialoliths appear smooth or slightly spiculated, and gray, yellowish, or white. The most common presentation is within the parotid duct, usually at its most rostral portion, just before it opens into the vestibule opposite the third upper cheek tooth with very few cases affecting the mandibular duct. Typically, a non-painful, movable, firm structure is palpable on the lateral aspect of the face near the rostral end of the facial crest, and it can be present for many years before additional clinical signs develop and lead to veterinary attention. In total, three horses and one donkey (four equines) were included in this study. All animals were in good clinical condition. None of these cases showed signs of concurrent sialadenitis or had problems eating. A detailed teeth examination showed severe enamel overgrowths on all arcades. In all cases, diagnosis of sialolithiasis was based on clinical presentation and palpation and was confirmed by surgically removing the sialolith. All sialoliths were removed with the animals standing under sedation and local anesthesia. In one case, a decision was made to remove the sialolith through a transcutaneous approach with ligation of the parotid duct at its rostral end. For the remaining three cases the transoral technique was elected. Although the size of the removed sialoliths varied, they ranged from 6 to 8cm in length. All four sialoliths were dissected, with no evidence of a plant or any other foreign material found in any of them. The first horse, in which the transcutaneous excision was elected, developed a marked distention of the parotid duct. Although the incision wound closed nicely, a visible blemish was created because of the retrograde distention of the parotid duct. In the remaining three animals, which were operated via the transoral technique, improvement was immedi
Keywords
Equines; Sialolith; Sialolithiasis; Parotid; Duct
Article Details
1. Introduction
Sialoliths are hard concretions composed primarily of calcium carbonate and organic matter that develop within a salivary duct or much less commonly a gland [1]. Sialolithiasis is an infrequently encountered condition in equids [2] and is considered to have a higher incidence in donkeys [3, 4]. Still, it occurs more frequently in equine species than other domestic species [5]. The etiology of sialolith formation is unknown; however, it is believed that the inciting cause is presence of organic matter in the duct [5, 6]. It is not uncommon for plant material to be found as a nidus of the sialolith formation [1, 4, 7].
Sialoliths appear smooth or slightly spiculated, and gray, yellowish, or white [1]. They are rarely recognized, but when they occur, they tend to affect older equids. The most common presentation is within the parotid duct, usually at its most rostral portion, just before it opens into the vestibule opposite the third upper cheek tooth (Triadan 108 or 208) with very few cases affecting the mandibular duct [2, 3, 8]. Typically, a non-painful, movable, firm structure is palpable on the lateral aspect of the face near the rostral end of the facial crest, and it can be present for many years before additional clinical signs develop and lead to veterinary attention [2, 6, 7]. In some cases, the sialolith may be palpable orally [1]. In man, sialoliths are found most often in the submandibular and parotid glands and less commonly in their associated ducts [9].
Sialoliths usually occur singularly, with rare reports of bilateral and multiple occurrence [1]. Definitive treatment is by removal of the sialolith [1, 10]. Both transcutaneous and transoral surgical techniques have been described for removal of sialoliths in the horse [1, 10]. Transcutaneous removal of sialoliths has been associated with increased incidence of post-operative infection at the surgical site and fistula formation compared with transoral removal, and also presents a risk for iatrogenic damage to the maxillary branch of the facial nerve [2]. While transoral sialolith removal has been advocated in the literature, information about long-term outcome for only a small number of cases is available [2]. The purpose of this paper was to review cases of equine sialolithiasis from Greece, describing diagnostic findings, surgical techniques that can be performed with the horse standing and long-term outcomes for affected animals, adding information to the existing literature.
2. Materials and Methods
Medical records of horses referred to the Equine Unit, School of Veterinary Medicine, Aristotle University of Thessaloniki were reviewed for cases of sialolithiasis of the distal parotid duct from 2012-2016. The distal parotid duct was previously defined as the portion of the duct that passes along the rostral border of the masseter muscle and exits into the oral cavity at the level of the second or third maxillary premolar [2]. In total, four equines were included in this study: three horses and one donkey. One horse lived in a riding club and the remaining three animals were kept in arid conditions. Detailed information on these animals was presented in Table 1. In all cases, the swelling had been gradually increasing in size for more than 12 months.
|
Species |
Breed |
Gender |
Age (years) |
Clinical presentation |
Method of surgical excision |
Complications |
|
|
1 |
Horse |
WB |
Gelding |
15 |
Non-painful, firm, freely movable mass near the rostral aspect of the facial crest |
Transcutaneous |
Distention of the parotid duct |
|
2 |
Horse |
TB |
Gelding |
9 |
Non-painful, firm, freely movable mass near the rostral aspect of the facial crest |
Transoral |
None |
|
3 |
Donkey |
Greek Arcadian |
Gelding |
17 |
Non-painful, firm, freely movable mass near the rostral aspect of the facial crest |
Transoral |
None |
|
4 |
Horse |
WB |
Gelding |
14 |
Non-painful, firm, freely movable mass near the rostral aspect of the facial crest |
Transoral |
None |
Table 1: Data on animals that met the inclusion criteria of the study.
On clinical examination a unilateral, firm, freely movable, relatively pain-free mass near the rostral aspect of the facial crest (4/4) could be seen and be palpated from the oral mucosa (Figure 1). In all cases, diagnosis of sialolithiasis was based on clinical presentation and palpation and was confirmed by surgically removing the sialolith. All animals were in good clinical condition. None of these cases showed signs of concurrent sialadenitis or had problems eating. A detailed teeth examination showed severe enamel overgrowths on all arcades.
In the first case, as the owner did not wish the horse to be subjected to general anesthesia and also raised concerns about the use of a mouth speculum, a decision was made to remove the sialolith through a transcutaneous approach, with the horse standing. Following sedation with romifidine (Sedivet®, Boehringer Ingelheim) (0,06mg/kg intravenously) and local anesthesia with 10ml of lidocaine 2% (Xylozane®, Demo) that were percutaneously injected around the sialolith, the maxillary region was clipped and surgically prepared. An incision with a #15 scalpel blade was made on top of the sialolith and parallel to its longitudinal axis [5]. An effort was made to avoid iatrogenic damage to the facial artery and vein which course beside the proximal aspect of the parotid duct [2]. The incision extended through the skin and the subcutaneous tissue into the parotid salivary duct. Entrance into the duct was identified by the presence of the sialolith and the secretion of saliva. The sialolith was gently removed and the parotid duct was catheterized with a canine urinary catheter and lavaged with sodium chloride 0,9% in order to make sure that all liths and debris were removed. The parotid duct was then ligated with polyglactin (Vicryl®) No 2/0 in a Cushing pattern [5]. The subcutaneous tissue and skin were sutured in a routine manner.
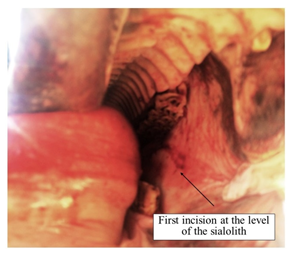
For the remaining three cases the transoral technique was elected. All operations took place with the animals standing. Each animal was sedated with detomidine (Detonervin®, Neocell) (0,01mg/kg intravenously). A full mouth speculum was fitted and 5ml of lidocaine 2% (Xylozane®, Demo) were injected into the buccal mucosa at the level of the sialolith [2, 3]. A #12 scalpel blade was used to create a linear incision through the buccal mucosa over the length of the sialolith (Figure 2).
Sharp dissection continued through the fibrotic capsule surrounding the sialolith within the duct[2, 3, 6]. Extra oral pressure over the sialolith aided in its removal into the oral cavity [2]. Following removal, the duct was carefully palpated and, following its catheterization with a canine urinary catheter, it was lavaged with sodium chloride 0,9% in order to make sure that all liths and debris were removed.
Finally, the incision of the oral mucosa was lavaged with povidone iodine 1% (Betadine mouthwash®, Lavipharm) and left open to heal by second intention [3]. Post-surgically, food was withheld for 24 hours and the mouth was lavaged daily with povidone iodine 1% (Betadine mouthwash®, Lavipharm) 3 times daily after meals for one week. Care was taken to remove all feed materials that were lodged within the wound.
Depending on the case, the sialoliths were removed either in one (Figure 3) or in several pieces (Figure 4). Although their sizes varied, they ranged from 6 to 8cm in length. It has to be stressed that an effort was made to remove every single fragment in order to avoid recurrence of the condition. Although all four sialoliths were dissected, a plant or any other foreign material was not found in any of them.
In all equines, post-operative treatment comprised of penicillin/streptomycin (20,000IU and 15mg/kg respectively, intramuscularly once per day) (Ilcocillin PS®, Norbrook) and phenylbutazone (4mg/kg intravenously once per day) (Stop-lac®, Provet) administration for 5 days.
3. Results
The first horse, in which the transcutaneous excision was elected, developed a marked distention of the parotid duct. Although the incision wound closed nicely, a visible blemish was created (Figure 5). In the remaining three horses, which were operated via the transoral technique, improvement was immediately seen following surgery and no blemishes or any other complications were noted. All four animals were able to masticate freely and showed no decrease in their appetite, no visible change in saliva production or predisposition to colic. On patient follow-up via telephone 3 years post-operatively, no signs of sialolith re-growth were noted by the owners.
4. Discussion
Sialolithiasis can cause partial or complete obstruction of the salivary duct, salivary gland dysfunction and oral mucosal ulceration. These conditions can lead to a significant degree of discomfort, dysphagia and possible gland atrophy [3]. Horses secrete copious amounts of saliva in comparison to other herbivores with a 500 kg horse producing an average of 12 liters daily with even higher volumes produced when fed dry or grain feed [11]. The production of saliva relies heavily upon mastication; feeds requiring more mastication induce greater saliva output. Saliva plays an important lubricating role, preventing esophageal obstruction and its high bicarbonate content (approximately 50 mmol/l) provides a gastric buffering function [12]. Obstruction of the salivary duct may, therefore, cause digestive disorders [3]. None of the animals included in this study had a history of digestive disorders. This could be explained by the fact that all these equines suffered from partial obstruction of the salivary duct, which is the most common form of the condition [1]. Moreover, none of the animals in this study suffered from any dental disease or had evidence of oral trauma; therefore, the ability for mastication and their appetite was normal. It is worth mentioning here, that animals in this study were in good clinical condition. Disease may remain subclinical, but acute obstruction of the salivary gland may lead to painful parotid distention and localized facial swelling with subsequent sialadenitis [2, 8]. None of the animals in this study had any signs of discomfort. Equids with obstruction of the parotid duct, especially at its proximal part, could show facial swelling, quidding, cutaneous draining track, fever, halitosis, inappetence, and facial nerve paralysis on the ipsilateral side of the sialolith or even worse, develop sialadenitis [1, 2, 4]. Concurrent sialadenitis usually follows proximal parotid duct sialolithiasis and is diagnosed based on the presence of warm, swollen, and painful salivary glands with definitive diagnosis made with cytology and culture of the saliva [2, 8]. None of our cases had sialadenitis, most probably because there were all cases of distal parotid duct sialolithiasis [2].
Although in the literature it is postulated that, sialolithiasis is more frequent in donkeys than in horses [3, 5], in this series of cases this tendency was not presented. It is unclear whether in Greece horses are more prone to developing sialoliths compared to donkeys. Perhaps that is related to the small number of cases. It is our feeling, though, that the major factor of this underrepresentation is the fact that Greek donkey owners seldom seek professional veterinary advice and even less often would be willing to transport their animal to a surgical center.
On the contrary, most of our animals (3/4) were kept in arid condition and were of advanced age, same as it has been proposed the literature [1, 2, 4, 8]. Although etiology is still unclear [13], formation of sialoliths has been related to organic nidus entering via the ostium and lodging in the duct, with or without concurrent bacterial infection; then, calcium salts (mostly carbonates) are deposited around it [3, 4, 8, 10]. Therefore, equids living in arid conditions are more susceptible to having organic debris lodging in the duct. Still, macroscopic dissection of the sialoliths in this study did not show the presence of a foreign body nidus. The lack of a nidus within the sialolith is not uncommon and has been related to the nidus being composed of cellular debris or dissolution of the nidus due to the chronicity of the condition [2, 8]. Unfortunately, excised sialoliths were not submitted for microscopic or mineral analysis. Therefore, the etiology is unknown, although it could be related to the enamel overgrowths [8]. The proximity between the opening of the distal parotid duct and the buccal aspect of the maxillary teeth allows more potential for trauma to the duct opening or surrounding tissue from sharp enamel points leading to subsequent opportunistic ascending infection by oral bacteria [8]. Inflammation and infection of the duct (of ascending, hematogenous, or traumatic origin) results in obstruction by exudates, desquamated cells, and mucus [1]. This material may provide the nidus necessary for a sialolith to form [1].
Formation of the liths could be related to the arid condition but also to saliva composition, dietary differences or water deprivation [3]. In human medicine, significant differences in saliva composition have been found in regard to salivary calcium, which was higher in the affected group, and salivary phytate concentration which was lower in the affected group [14]. These researchers concluded that a deficit of crystallization inhibitors such as myo-inositol hexaphosphate (phytate) could be a significant aetiological factor in the genesis of sialoliths [14]. Further work to measure salivary composition in affected and control groups in equine sialolithiasis would be beneficial, especially to investigate possible inter species differences between horses and donkeys [3].
Diagnosis of equine sialoliths is made easily based on physical examination alone, as clinical signs are quite characteristic [3, 6, 7, 4, 1]. Sialoliths are recognized by palpation of the characteristic hard, smooth, mobile and painless enlargements at the level of the upper arcade adjacent to the third or fourth cheek tooth [3, 10]. Although radiography and ultrasonography can aid in certain cases [10], such modalities were not used in this study, and diagnosis was based on clinical presentation and palpation. Moreover, in humans roughly 20% of submandibular sialoliths are not radiopaque or too small for identification by radiography [15]. Radiography and especially ultrasonography should be used in cases where sialolithiasis of the proximal duct is suspected [2]. Finally, sialoendoscopy may also be considered for imaging obstructive conditions of the salivary ducts [1, 16]. Possible differential diagnosis includes sialoadenitis, tooth abscess, buccal tumors, chronic fracture, metaplasia, ductal skin associated neoplasia, granulomatous lesions of skin or subcutis and dystrophic calcification [3, 4, 8, 10, 13].
In one case, a modification of the transcutaneous method of excision was elected because of the owner’s reservations. The distal parotid duct was ligated, knowing that the parotid duct would develop chronic distention. In recent years, and in order to avoid distention several techniques have been put forward that rely on the catheterization of the duct [2, 10]. Cannulation of the parotid duct via the parotid papilla can be helpful to locate the exact calculus position, and the catheter can act as a stent for suturing the duct if primary closure is performed [1]. Unfortunately, most of these techniques require general anesthesia and the owner was unwilling to give its consent. Therefore, the method described was elected and the possibility of the blemish was explained to the owner preoperatively. Although it left an obvious blemish, this technique could be used a last resort in field conditions, provided the owner is informed in advance. It is much simpler, more straight –forward and faster compared with the other methods. In retrospect, perhaps we should have thought about using the Poore et al. technique (2019), which was proposed much later. In literature, transcutaneous removal has a number of potential complications, such as post-operative infection at the surgical site, iatrogenic damage to the facial artery, vein and nerve and fistula formation [2, 3, 5]. None of these adverse reactions were seen in this case, possibly because of the ligation of the duct. Perhaps the transcutaneous technique should be considered only in cases of proximal parotid duct sialadenitis where the lith is inaccessible via the oral cavity [1, 2, 6, 8, 17].
The transoral technique is much more advantageous compared with the transcutaneous approach and is recommended by numerous authors [1-6, 13]. When using the intraoral approach, sialolith removal can be achieved by enlarging the parotid duct opening [4, 7] or by incising the oral mucosa over the sialolith [3, 4]. In this study the latter technique was chosen mainly because detecting the parotid duct papilla during surgery is not necessary and as a result surgical time is minimized [4] Complications of a transoral approach include focal cellulitis that resolves easily, difficulty in accessing the sialolith, infection at the unsutured surgical site, fistula formation at the surgical site and granulation tissue causing an obstruction at the buccal ostium [2, 4, 8]. No complications were noted in our cases.
Reported recurrence rates reach a percentage of approximately 24% [2] and it is observed in the same location and duct as the initial sialolith [2]. None of our cases showed signs of recurrence 3 years post-operatively. The etiology of sialolith formation is not clear in this study, as no nidus was found. Although the stabling conditions remained the same, no animal relapsed. The two main factors predisposing to recurrence is scar formation and incomplete initial removal of the sialolith [2]. It is possible that this positive outcome was related firstly to the minimal post-operative scar formation and secondly to the copious lavage following the removal of the sialolith.
5. Conclusions
Although, sialolithiasis of the distal parotid duct is relatively uncommon in horses, it occurs more frequently in equine species than in other species [5]. Therefore, the equine clinician should include this condition in the differential diagnosis of cases characterized by the presence of a hard, freely moveable mass located at the maxilla in the region of the third check tooth. In the current study, the clinical signs and successful surgical removal of sialoliths in 4 equids were presented. Both transcutaneous and transoral techniques that could be completed with the horse standing were used. Based on the results of this study, it is recommended that sialoliths should be identified as early as possible at the course of the disease, before they grow substantially in size and that the transoral surgical excision is the treatment of choice provided that the sialolith is accessible orally.
Acknowledgements
No funding has been received for the study.
Conflicts of Interest
There are no conflicts of interest.
References
- Gerard MP. Sialoliths. In: Auer, Stick, Kummerle and Prange Equine Surgery, 5th ed, Elsevier, Missouri (2019): 468-469.
- Carlson N, Eastman T, Winfield L. Sialolithiasis in horses: A retrospective study of 25 cases (2002-2013). Can Vet J 56 (2015): 239-1244.
- Kay G. Sialolithiasis in equids, a report on 21 cases. Equine Vet Educ 18 (2006): 333-336.
- Oreff GL, Shiraki R, Kelmer G. Removal of sialoliths using the intraoral approach in 15 horses. Can Vet J 57 (2016): 647-650.
- Al-Sobayil FA, Ibrahim IM. Parotid duct sialolithiasis in horses. J Equine Vet Sci 28 (2008): 437-439.
- MacLean YT. Chronic sialolithiasis in a Trakehner mare. Can Vet J 47 (2006): 480-482.
- Haralambus RMA, Simhofer H, Zappe H. Removal of a sialolith by an intraoral surgical approach in a Warmblood gelding. Vet Rec 161 (2007): 354-356.
- Kilcoyne I, Watson JL, Spier SJ, et al. Septic sialoadenitis in equids: A retrospective of 18 cases (1998–2010). Equine Vet 47 (2015): 54-59.
- Hong, KH, Yang, YS. Sialolithiasis in the sublingual gland. J. Laryngol. Otol 117 (2003): 905-907.
- Poore L, Smit Y, Williams J, et al. Standing transcutaneous surgical excision of a sialolith in an11-year-old Thoroughbred mare. Equine Vet J 31 (2019): 343-347.
- Kohnke J, Kelleber F, Trevor-Jones P. Feeding Horses in Australia: A Guide for Owners and Managers, 1st edn., CSIRO Publishing, Collingwood (1999): 17-18.
- Frape D. Equine Nutrition and Feeding, 3rd edn., Blackwell, Publishing Ltd. (2004): 4.
- Baskett A, Parks A, Mahaffey M. Sialolith and sialadenitis associated with a foreign body in a mare. Equine Vet. Educ 7 (1995): 309-312.
- Grases F, Santiago C, Simonet BM. Sialolithiasis, mechanism of calculi formation and etiologic factors. Clin. Chima Acta 334 (2003): 131-136.
- Marchal F, Dulguerov P. Sialolithiasis management. Arch Otolaryng Head Neck Surg 129 (2003): 951-956.
- Prutton JSW, Bonadio C, Vaughan B, et al. Sialoendoscopy as a treatment for an obstructed mandibular salivary duct in a horse. Can Vet J 57 (2016): 869-872.
- Schumacher J, Schumacher J. Diseases of the salivary glands and ducts of the horse. Equine Vet Educ 7 (1995): 313-319.