Epidemiological, Therapeutic and Evolutive Aspects of Bladder Cancer in Douala
Article Information
Jean Paul Engbang1,2*, Hervé Moby1, Falonne Daoudou Soumaï1, Boris Amougou3,4, Makon Nwaha2,5, Marcelin Ngowe Ngowe1,5
1Faculty of Medicine and Pharmaceutical Sciences, The University of Douala, Douala, Cameroon
2Douala Laquintinie Hospital, Douala, Cameroon
3Faculty of Medicine and Pharmaceutical Sciences, The University of Dschang, Dschang, Cameroon
4Niete Central Hospital, Niete, Cameroon
5Faculty of Medicine and Biomedical Sciences,The University of Yaounde I, Yaounde, Cameroon
*Corresponding author: Jean Paul Engbang, Faculty of Medicine and Pharmaceutical Sciences, The University of Douala, Douala, Cameroon
Received: 26 February 2022; Accepted: 04 March 2022; Published: 14 March 2022
Citation: Jean Paul Engbang, Hervé Moby, Falonne Daoudou Soumaï, Boris Amougou, Makon Nwaha, Marcelin Ngowe Ngowe. Epidemiological, Therapeutic and Evolutive Aspects of Bladder Cancer in Douala. Archives of Nephrology and Urology 5 (2022): 9-23.
Share at FacebookAbstract
Bladder cancer can be defined as the uncontrolled proliferation of bladder cells, leading to the formation of a heterogeneous lesion. These bladder cells have variable sizes with no clear boundaries and potential to invade or spread to other parts of the body. This pathology is ranked second among genito-urinary cancers after prostate cancer. Our goal is to study the epidemiological, therapeutic and evolution aspects of bladder cancer in three hospitals in the city of Douala.
Methodology: We carried out a descriptive study on the medical files of the patients during a period of 10 years, from January 1st 2011 to December 31st 2020. We retrieved medical reports of patients with bladder cancer in three hospitals in the city of Douala and included medical reports that provided information on age, sex, patient’s or guardian’s phone number and the pathology results. Our results were analyzed using SPPS 25.0 software.
Results: We included a total of 122 medical reports in our study. There were 74 men and 48 women. The mean age was 58.0±13.3 years with extremes between 24 years and 91 years. The most affected professions were housewives and farmers with 34 cases (27.8%) and 27 cases (22.1%) respectively. The mean consultation period of patients to the urologist was 2.2 months. The most frequent symptom reported by patients was macroscopic hematuria in 80 cases (65.6%). Past medical history of active smokers was the most frequent in 36 patients (29.5 %), followed by recurrent urinary tract infection. At the histology level, urothelial carcinoma was the most common finding with 60 cases (49.2%). Medical and surgical treatment was established according to the tumoral stage. In stage II, transurethral resection associated with local chemotherapy after surgery was performed in 69 patients (66.3%). In stages III and IV, 66.6
Keywords
Cancer of the bladder; Douala; Global survival; Treatment
Cancer of the bladder articles; Douala articles; Global survival articles; Treatment articles
Cancer of the bladder articles Cancer of the bladder Research articles Cancer of the bladder review articles Cancer of the bladder PubMed articles Cancer of the bladder PubMed Central articles Cancer of the bladder 2023 articles Cancer of the bladder 2024 articles Cancer of the bladder Scopus articles Cancer of the bladder impact factor journals Cancer of the bladder Scopus journals Cancer of the bladder PubMed journals Cancer of the bladder medical journals Cancer of the bladder free journals Cancer of the bladder best journals Cancer of the bladder top journals Cancer of the bladder free medical journals Cancer of the bladder famous journals Cancer of the bladder Google Scholar indexed journals Douala articles Douala Research articles Douala review articles Douala PubMed articles Douala PubMed Central articles Douala 2023 articles Douala 2024 articles Douala Scopus articles Douala impact factor journals Douala Scopus journals Douala PubMed journals Douala medical journals Douala free journals Douala best journals Douala top journals Douala free medical journals Douala famous journals Douala Google Scholar indexed journals Global survival articles Global survival Research articles Global survival review articles Global survival PubMed articles Global survival PubMed Central articles Global survival 2023 articles Global survival 2024 articles Global survival Scopus articles Global survival impact factor journals Global survival Scopus journals Global survival PubMed journals Global survival medical journals Global survival free journals Global survival best journals Global survival top journals Global survival free medical journals Global survival famous journals Global survival Google Scholar indexed journals Insulin dose articles Insulin dose Research articles Insulin dose review articles Insulin dose PubMed articles Insulin dose PubMed Central articles Insulin dose 2023 articles Insulin dose 2024 articles Insulin dose Scopus articles Insulin dose impact factor journals Insulin dose Scopus journals Insulin dose PubMed journals Insulin dose medical journals Insulin dose free journals Insulin dose best journals Insulin dose top journals Insulin dose free medical journals Insulin dose famous journals Insulin dose Google Scholar indexed journals Treatment articles Treatment Research articles Treatment review articles Treatment PubMed articles Treatment PubMed Central articles Treatment 2023 articles Treatment 2024 articles Treatment Scopus articles Treatment impact factor journals Treatment Scopus journals Treatment PubMed journals Treatment medical journals Treatment free journals Treatment best journals Treatment top journals Treatment free medical journals Treatment famous journals Treatment Google Scholar indexed journals bladder cancer articles bladder cancer Research articles bladder cancer review articles bladder cancer PubMed articles bladder cancer PubMed Central articles bladder cancer 2023 articles bladder cancer 2024 articles bladder cancer Scopus articles bladder cancer impact factor journals bladder cancer Scopus journals bladder cancer PubMed journals bladder cancer medical journals bladder cancer free journals bladder cancer best journals bladder cancer top journals bladder cancer free medical journals bladder cancer famous journals bladder cancer Google Scholar indexed journals diabetes articles diabetes Research articles diabetes review articles diabetes PubMed articles diabetes PubMed Central articles diabetes 2023 articles diabetes 2024 articles diabetes Scopus articles diabetes impact factor journals diabetes Scopus journals diabetes PubMed journals diabetes medical journals diabetes free journals diabetes best journals diabetes top journals diabetes free medical journals diabetes famous journals diabetes Google Scholar indexed journals
Article Details
1. Introduction
Cancer is a pathology resulting from both the inability of cells to control their division and the loss of the cell death programming mechanism [1]. Bladder cancer ranks ninth in the world, with 430,000 new cases each year [2]. This pathology is ranked second amoung genito-urinary cancers after prostate cancer [3]. Multiple risk factors are incriminated. The most common are smoking, occupational exposure, infections and chronic irritation of the bladder [4]. It is estimated that a bladder tumor is diagnosed or treated in 2.7 million people every year worldwide [5, 6]. In the United States of America and France, there are respectively 79,000 and 12,305 new cases of bladder cancer each year [7]. The diagnosis of a bladder tumor will be evoked clinically in the presence of macroscopic hematuria or a bladder mass and the histology will confirm it [8]. Depending on the histopathology of epithelial tumors, a distinction is made between benign lesions or papillomas and malignant lesions or carcinomas [9]. Only the latter will be the subject of our work. Thus, by the painful nature of its symptoms and the often mutilating nature of its therapy, this pathology is formidable [10]. Nowadays, depending on whether or not the muscle is infiltrating, the surgical management of bladder tumors ranges from simple resection to radical treatment. Thanks to improved exploration techniques, 7 out of 10 cases of bladder cancer can be detected at an early stage [11]. Thus, bladder tumors that do not infiltrate the muscle are generally removed by transurethral resection and intravesical cytotoxic treatment can be added [12]. In addition, for the 30% of patients with cancer infiltrating the muscle, management remained exclusively surgical for a long time (total cystectomy followed by urinary diversion or reconstruction), with a probability of survival at 5 years for all stages combined in only 60%. The development of chemotherapy has made it possible to be offered in cases of invasive cancer in combination with surgery, as an alternative to surgery or for symptomatic purposes in the event of metastatic tumor from the outset [13]. Although survival rates have improved with earlier diagnosis, innovative surgical techniques and the introduction of immunotherapy, bladder cancer remains a significant and growing contributor to cancer worldwide [14]; and in particular in Africa where cancer is a public health problem and much progress remains to be made [15,10]. In Cameroon, bladder cancer ranks nineteenth, representing 1% of all cancers [16]. The epidemiological and histological aspect of bladder cancer have been the subject of numerous studies. In 2006, in the central region, Sow et al found bladder cancer second among all urogenital cancers with a prevalence of 19.2%. In 2014, in the coastal region, Engbang et al noted a prevalence of 16.3% of this cancer with a predominance of transitional carcinomas, i.e., 81.48% [17]. However, there is a scarcity of studies on the therapeutic and evolutionary aspects of bladder cancer. We have found it appropriate to devote scientific attention to this area.
2. Materials and Method
This was a retrospective, descriptive study concerning patients suffering from malignant tumors of the bladder, in the period from January 1st 2011 to December 31st 2020, in the Laquintinie and general hospitals of Douala and at the Medical-Surgical Center of Douala. We screened records and registers from surgery, oncology, operating theatre, pathology and outpatient departments at the different study sites for data on patients with bladder cancer. During our study period. Data collection began with the identification of the various patients registered in the registers and the search for the corresponding files. After finding the files, we proceeded to fill in the collection sheets from the files of the patients who met our inclusion criteria. Missing information, in particular that relating to survival was obtained by making telephone calls to patients or their relatives. The variables collected concerned socio demographic, clinical, paraclinical and therapeutic data. The variables were entered and analyzed using the SPSS version 25.0 software.
3. Results
During our study period, we identified 1018 urogenital tumors including 135 bladder tumors. Subsequently, we excluded 13 files including 7 benign tumors, 9 incomplete files and 3 cases of secondary invasion. Thus, our study population had 122 files. Bladder cancer ranked second among urogenital malignancies with a hospital prevalence of 16.1% (122 cases) behind prostate cancer. In our study population, there was a male predominance with 74 cases (61%) with a sex ratio of 1.5. The ages varied between 24 and 91 years for an average age of 58.0 ± 13.3 years. The most represented age group was between 50 and 59 years old with 42 cases (34.4%). it was noted that 95 patients (77.9%) lived in urban areas. Housewives and farmers were the most represented with respectively 34 cases (27.8%) and 27 cases (22.1%). Married people with 76 cases (62.3%) were the most encountered. Arterial hypertension and diabetes were the most common medical histories with 31 cases (25.4%) and 23 cases (18.9%) respectively. Recurrent urinary tract infection found in 33 patients (27.0%) and urinary schistosomiasis in 9 patients (7.3%) were the most common urological history findings. Active smoking was the most common toxicological history in 36 patients (29.5%). Passive smoking was also noted in 23 patients (18.8%). Swimming in rivers in childhood or adolescence was practiced by 67 patients (54.9%). Also, a sedentary lifestyle, the consumption of vegetables and fruits could not be specified in most of our patients with accuracy. Regarding work history, 6 of our patients had worked as farmers in industrial plantations and 1 employee in a metal factory. The duration in these structures varied between 4 and 11 years. Cardiovascular diseases (diabetes and hypertension) with 13 cases (10.6%) and prostate neoplasia 4 cases (3.2%) were the most found family history.
Macroscopic hematuria was the most common reason for consultation with 80 cases (65.6%). Dysuria present in 30 patients (24.6%) and the presence of a bladder mass on ultrasound of the urinary tract in 20 patients (16.4%) were the other reasons for consultation or referral. In 102 patients (83.6%), good general condition was found. In addition, 20 patients had a general condition marked by asthenia in 14 patients (11.5%), weight loss in 13 patients (10.7%) and anorexia in 5 patients (4.1%). In the systemic survey, voiding disorders ranked first: first came dysuria with 89 cases (73.0%); then pollakiuria with 56 cases (45.9%) and urinary burns with 49 cases (40.2%). The majority of our patients had a normal physical examination (70 patients; 57.3%); however, pathological digital rectal examination was found in 34 patients (27.9%) and lower limb edema in 21 patients (17.2%).
In 73 patients (82.0%), the ultrasound appearance revealed a single mass (43 cases; 58.9%). The lesions predominated on the bladder dome in 15 patients; the impact on the upper urinary tract was present in 38 patients (42.6%). The presence of a prostatic adenoma in 19 patients (25.5%) and urolithiasis in 13 patients (17.5%) were the other anomalies encountered. The cystoscopy carried out in 57 patients, made it possible to highlight the budding aspect in 43 patients and for the most part the implantation base was sessile (22 cases; 38.4%). The tumors were mostly single and predominant on the bladder dome. Urinary cytology was performed in 18 patients, half of whom revealed the presence of suspicious cells and the rest the presence of neoplastic cells. The IVU made in only 3 patients (2.4%) showed a lateral lesion with an impact on the upper urinary tract in all our patients. CT uroscan was performed in 23 patients, 11 of whom (47.8%) presented with a bladder mass. pelvic with 9 cases (39.1%). The thoraco-abdominal CT scan found a bladder mass in 35 patients (54.5%) and parietal thickening in 22 patients (34.3%). Lymph node metastases were the most common secondary location with 28 cases (43.7%). Chest X-ray revealed lung metastases in 7 patients (43.7%). Severe anemia was found in 4 patients (3.2%), the leukocyte count of 115 patients (94.3%) was normal, however, 7 patients (5.7%) had neutrophilic polynuclear leukocytosis. Platelet lineage was the same for any abnormalities. All our patients had a urine culture, of which 16 samples (14.1%) found a germ; Escherichia coli was the most common germ. In our series, 31 patients (25.4%) had elevated serum creatinine, the majority of men (39 patients 63.9%) had a normal total PSA level. In addition, the urinary pellet of a single patient found eggs of schistosoma haematobium. In our series, 104 samples (85.2%) were samples from transurethral resection of the bladder (TURB). Cystoscopy provided only 15 samples (12.2%). The most common histological type was urothelial carcinoma in both sexes with 60 cases (49.2%). Squamous cell carcinoma was also found (22 cases; 59.5%). The 50 to 59 age group was the most affected by all histological types, with 42 cases (34.4%). Squamous cell carcinoma and squamous cell carcinoma with urothelial differentiation were most commonly found in people under 30 years old. Regarding differentiation, grade III was the most encountered with 48 cases (39.5%), followed by grade II - 47 cases (38.5%). Stage II was found the most with 75 cases (61.4%), followed by stages III and IV with respectively 22 cases (18.0%) and 18 cases (14.7%).
All our patients had received symptomatic medical treatment at the time of the first consultation. In this study, 117 patients (95.9%) benefited from a surgical act against 5 (4.1%) who opted for a therapeutic abstention. Treatment was based on tumor stage. At stage II, 70 patients (61.4%) had benefited from RTUV, while intravesical chemotherapy was used in 28 patients (96.6%). In stages III and IV, respectively 4 patients (50.0%) and 3 patients (37.5%) benefited from radical surgical treatment. While respectively 13 patients (43.3%) and 14 (46.7%) had received general chemotherapy. this difference in treatment distribution according to stage was significant (p=0.000). Thus, in total, conservative surgery was used in 114 patients (97.4%), including RTUV in 104 patients (91.2%), partial cystectomy in 5 patients (4.3%) and cystectomy with Ureterovesical reimplantation also in 5 patients. As for radical surgery, 8 patients benefited from it, including 4 patients with vesiculocystoprostatectomy (50.0%); 2 patients had previous pelvectomy (25.0%) and 2 had cystoprostatectomy (25.0%) Urinary diversion by transintestinal cutaneous ureterostomy was performed in 5 patients (62.5%). (Tables 1, 2).
|
Variables |
Effective (%) |
p |
||||
|
Stage 0&1 |
Stage 2 |
Stage 3 |
Stage 4 |
Total |
||
|
Surgery N=117 |
||||||
|
Conservative |
7 (6,1) |
70 (61,4) |
22 (19,3) |
15 (13,2) |
114 (97,4) |
0,63 |
|
Radical |
- |
1 (12,5) |
4 (50,0) |
3 (37,5) |
8 (6,8) |
0,09 |
|
Surgical abstention |
- |
2 (40,0) |
- |
3 (60,0) |
5 (4,1) |
0,63 |
|
Chimiotherapy N=59 |
||||||
|
General |
- |
3 (10,0) |
13 (43,3) |
14 (46,7) |
30 (50,8) |
0,000 |
|
Postoperative intravesical |
1 (3,4) |
28 (96,6) |
- |
- |
29 (-49.2) |
0,000 |
|
TURB -Transurethral resection of the bladder |
||||||
Table 1: Distribution of specific treatment according to tumor stage.
|
Variable |
Effective |
Percentage(%) |
|
Conservative surgery N=114 |
||
|
TURB |
104 |
91,2 |
|
Partial cystectomy |
5 |
4,3 |
|
Partial cystectomy + UV reimplantation |
5 |
4,3 |
|
Radical surgery + lymph node dissection N=8 |
||
|
Vesiculocystoprostatectomy |
4 |
50,0 |
|
Anterior pelvectomy |
2 |
25,0 |
|
Cystoprotectomy |
2 |
25,0 |
|
Urinary diversion and replacement N=8 |
||
|
External: trans-intestinal ureterostomy |
5 |
62,5 |
|
Internal: Sigmoid ureterostomy Neobladder |
1 |
12,5 |
|
Hautman enterocystoplasty |
1 |
12,5 |
|
Studer enterocystoplasty |
1 |
12,5 |
|
Surgical abstention |
5 |
4,1 |
|
U.V reimplantation = Ureterovesical reimplantation |
||
Table 2: Distribution according to the different therapeutic modalities
The general chemotherapy protocol was administered according to the tumor stage. In stage III, MVAC was the most used in 7 patients (50.0%). In addition, at stage IV, protocols containing cisplatin salts including Gemcitabine-cisplatin and Cisplatin-Paclitaxel were used in 6 patients (50.0%) and 3 patients (75.0%) respectively. This difference in distribution was not significant (P-value = 0.69). However, 21 patients (70%) had received only 2 cycles of chemotherapy. Regarding postoperative local chemotherapy, overall it was more used in stage II in 28 patients (96.6%) and weekly instillation of MMC was the most used protocol in 18 patients (94.7%). In addition, 19 patients had benefited from a treatment of 1 cycle of chemotherapy. This difference in distribution was not significant (P-value = 0.9) (Table 3).
|
Variables |
Effective (%) |
P |
||||
|
Stage 0&1 |
Stage 2 |
Stage 3 |
Stage 4 |
Total |
||
|
General chemotherapy N=30 |
0,69 |
|||||
|
MVAC |
- |
2 (14, 2) |
7 (50, 0) |
5 (35,7) |
14 (46,7) |
|
|
Gemcitabin-Cisplatin |
- |
1 (8, 3) |
5 (41, 6) |
6 (50,0) |
12 (40,0) |
|
|
Cisplatin – paclitaxel |
- |
- |
1 (25,0) |
3 (75,0) |
4 (13,3) |
|
|
Number of cycles N=30 |
0,8 |
|||||
|
2 |
- |
2 (9,5) |
9 (42,8) |
10 (47,6) |
21 (70,0) |
|
|
3 |
- |
1 (11,2) |
4 (4,44) |
4 (44,4) |
9 (30,0) |
|
|
Postoperative chemotherapy |
0,46 |
|||||
|
MMC weekly |
1 (5,3) |
18 (94,7) |
- |
- |
19 (65,5) |
|
|
IPOP |
- |
10 (100,0) |
- |
- |
10 (34,4) |
|
|
GC |
- |
- |
- |
2 (6,66) |
2 (6,66) |
|
|
Number of cycle |
0,9 |
|||||
|
1 |
1 (5,2) |
18 (94,7) |
- |
- |
19 (89,6) |
|
|
2 |
9 (90,0) |
1 (10,0) |
- |
- |
10 (34,4) |
|
|
MVAC= Methotrexate -Vinblastin – Doxorubicin - Cisplatin |
||||||
Table 3: Distribution according to the type of chemotherapy received.
|
Variables |
Effectivr (%) |
P |
||||
|
Stage 0&1 |
Stae 2 |
Stage 3 |
Stage 4 |
Total |
||
|
RTUV N=104 |
||||||
|
Only |
6 (12,0) |
39 (78,0) |
3 (14,0) |
2 (4,0) |
50 (48,0) |
0,000 |
|
Combined with local chemotherapy |
1 (3,4) |
28 (96,5) |
- |
- |
29 (27,8) |
|
|
Cystectomy T/P N=122 |
||||||
|
Combined with general chemotherapy |
- |
1 (11,1) |
6 (66,6) |
2 (22,2) |
9 (7,3) |
0,000 |
|
Without general chemotherapy |
- |
1 (11,1) |
7 (77,8) |
1 (11,1) |
9 (7,3) |
|
|
General chemotherapy only N=122 |
- |
- |
- |
1 (100,0) |
1 (0,8) |
0,000 |
|
In our series, the postoperative course was marked in 15 patients (12.8%), including 4 cases (3.4%) of persistent hematuria and 3 cases (2.5%) of parietal and urinary infections. This corresponds to a comorbidity rate of 12.8%. |
||||||
Table 4: summarizes the different therapeutic combinations used.
Tableau XLVI : répartition selon les combinaisons thérapeutiques.
|
Post operative follow-up |
Effective N=117 |
Percentage(%) |
|
Simple |
104 |
88,8 |
|
Complications |
15 |
12,8 |
|
Persistence of hematuria |
4 |
26,6 |
|
Parietal infections |
3 |
20,0 |
|
Urinary tract infections |
3 |
20,0 |
|
Anemia |
2 |
13,3 |
|
Thromboembolic |
1 |
6,7 |
|
Abutment Lithiasis |
1 |
6,7 |
|
Eventration |
1 |
6,7 |
Table 5: Répartition selon les suites opératoires.
The median survival in our series was 59.9 months with a CI: [42.622-75.378] the overall survival rate varied between 1 year, 3 years and at 5 years were respectively 85.2%, 41.0 % and 12.3% (Figure 1)
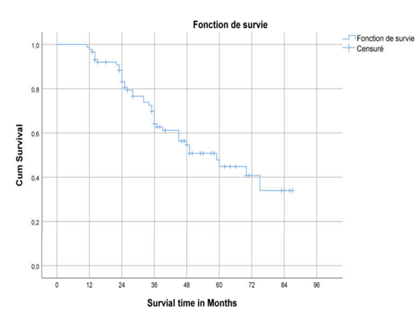
Figure 1: 5-year overall survival curve.
4. Discussion
In our series of 122 patients, bladder cancer ranks second among urogenital malignancies with a hospital prevalence of 16.1% behind prostate cancer. This result is close to that of Engbang et al in Cameroon in 2014, Daré et al in Togo in 2014 and Badiaga et al in Mali in 2018, who respectively found 16.3%, 14.1% and 14.0 % [17-19]. On the other hand, this prevalence is lower than that found in the countries of North Africa. Indeed, Salah et al in Algeria in 2015 and Hebat et al in Egypt in 2019 found 60.3% and 75.0% respectively [20, 21]. This result can be justified by the presence of a high technical platform and cancer registries in these North African countries guaranteeing the quality of the data and a better approach to estimate the incidences and the different epidemiological parameters of cancers. Moreover, according to a WHO report published in 2015, urinary schistosomiasis, which is one of the actors of this cancer, is an endemic parasitosis in more than 78 countries in the world, including 42 African countries [22]. This higher rate in North Africa and particularly in Egypt is also linked to the proximity to the Nile region, where Schistosoma haematobium infection is endemic [23]. In our population, we found a male predominance of 61%. This observation is made in many literatures, such as by Saurabh et al in Central and Eastern Europe, Hebat et al in Egypt in 2019, and Touré in Mali in 2020 with respectively 77.9%, 91.1% and 63, 2%. [21, 24, 25]. This could be explained by the more frequent exposure of men to known risk factors; including smoking and environmental conditions related to the occurrence of this neoplasia. In addition, some studies mention the involvement of a failure of the Y chromosome due to the action of carcinogens [26, 27]. The ages varied between 24 and 91 years for an average age of 58.0 ± 13.3 years. This result is higher than those found by Amiroune et al in Morocco in 2012 and Sow et al in Cameroon 2006 where the average age was 35 years [16, 28]. This could be justified by the early infestation with Schistosoma haematobium in children and adolescents during play activities and field work, which will be responsible for bladder neoplasia in adulthood [21].
Furthermore, some authors incriminate a hereditary predisposition in the occurrence of bladder tumors in young subjects, in particular genetic mutations on chromosomes 7 and 17, however these results are still preliminary [29,30]. On the other hand, in the series of Engbang et al in Cameroon in 2016, of Traore et al in Senegal in 2018 and of Lebret in France and other European series in 2020, the average age was respectively 52.3 years, 55 and over 60 [31-34]. It is true that bladder tumors can occur at a young age, but more than 90% of new cases appear in people over the age of 55 [35]. Indeed, aging promotes carcinogenesis by potentiating genetic abnormalities induced by risk factors and by reducing the performance of the immune system that can destroy cancer cells [35]. This explains the high frequency of bladder tumors in the elderly.
In our series, the most common antecedents found were active and passive smoking in 29.5% and 18.8% of patients, respectively, then recurrent urinary tract infections in 27.9% and urinary schistosomiasis in 7.3% of patients. Indeed, smoking is the most common risk factor encountered worldwide, and is attributed to 50% in the occurrence of cancer in Europe [36]. In 2016, in Cameroon, Engbang et al already pointed out that active smoking, but also passive smoking, are linked to the occurrence of bladder cancer [31]. In fact, tobacco contains more than 43 recognized carcinogenic compounds including 4-aminobiphenyl and o-toluidine which are excreted in the urine causing local changes. Other products of amine pyrolysis such as 2-naphthalamine would also modify the urinary environment [37]. Thus, some authors estimate that the risk of developing bladder cancer is 2 to 4 times higher in smokers compared to non-smokers and this risk increases with the intensity and/or duration of smoking [37]. On the other hand, for authors from countries with high endemicity of urinary schistosomiasis, like Touré in Mali in 2020 with 73.5% of cases and Traoré et al in Senegal in 2018 with 36.0% of cases, the Schistosoma haematobium infection is the first incriminated in the occurrence of this type of cancer [25,32]. Indeed, the chronic presence of the eggs of this parasite in the bladder environment leads to a significant granulomatous reaction responsible for intravesical lesions of the ulceration type, polyploid growths and fibrosis which in the long term will lead to bladder dysfunction [38,39]. The sedentary lifestyle, the consumption of vegetables and fruits could not be specified in most of our patients with accuracy, it would be necessary to carry out prospective studies to specify their implication in the occurrence of bladder cancer. Cardiovascular diseases (diabetes and hypertension) and prostate cancer were the most common family history in 10.6% and 3.2% respectively. No family history of bladder cancer was found. This could be explained by the fact that bladder cancer would have more of an origin linked to environmental factors than to genetics. Regarding the consultation time, it was 2.1 ± 1.4 weeks with a general practitioner and 2.2 ± 1.4 months with a specialist. This promptness in consulting the general practitioner would be explained by the accessibility of the latter compared to urologists who are found only in metropolitan areas. On the other hand, this consultation time with the urologist was early compared to that of Traoré et al in Senegal in 2018 and Touré in Mali in 2020 where the average time was respectively 7 and 28.6 months justified by the high cost of health Care service which referred most patients to traditional medicine at first and it was only at an advanced stage of the disease that they presented to the hospital [25, 32]. Gross hematuria was the most common reason for consultation in 65.5% of patients. This figure is similar to that of most published series, including those of Messing et al in 2006, Niang et al in 2014 in Senegal and Boureima et al in Burkina Faso in 2020, which respectively found 85.0%, 77.5% and 61.1% [35,40,41].
These results are also found in European studies where macroscopic haematuria, often terminal, is the most frequent clinical sign associated with signs of bladder irritation in the absence of urinary infection, are observed in 4 to 20% of cases [42,43]. On the other hand, this observation is different from Diao et al, where irritative signs represented the most frequent reason for consultation with voiding disorders in 94.5% of cases and hematuria was in second position in 88% [44]. On admission, the general condition was preserved in 83.6% of patients, as in the series by Traoré et al in Senegal in 2018, where he found an identical result in 61.0% of cases [32]. On the other hand, it differs from those of Touré in 2020 and Dembélé in 2012 in Mali where weight loss was present respectively in 75.2% and 54.3% [25,45]. This could be explained by the average late consultation time in their different series [25,45]. However, our result was consistent with the literature which states that the physical examination is uninformative [8].
In order to make the diagnosis, our patients benefited from a check-up including an ultrasound of the urinary tract, a cystoscopy, a urinary cytology and an UIV. Urinary tract ultrasound was made in 73,0%. Touré found the same result in Mali in 2020 [25]. Whereas in the series by Traoré et al in 2018, cystoscopy was the key diagnostic examination [32]. Regarding the extension assessment, the thoraco-abdominal CT scan showed that lymph node and pelvic metastases were the most common secondary locations in 43.7% and 26.5% respectively. These results are in agreement with some authors in the literature who claim that metastases are infrequent in bladder cancer [32,34]. Furthermore, since TAP CT cannot assess parietal infiltration early on, it is recommended to perform a uroscan at the time of the initial diagnosis of DVT [46]. Thus, 18.8% of our patients had a uroscan. The most common histological type was urothelial carcinoma at 49.2%, as in the Boureima et al series in Burkina Faso and most European series [33, 35]. This result is different from those found in Senegal by Traoré et al in 2018 and Touré in Mali where the predominance of squamous cell carcinoma is noted in 50.2% and 57.9% [25, 32]. Our finding could be explained by the greater exposure to smoking, favoring the type of urothelial cancer. Moreover, urothelial carcinoma with squamous cell differentiation has not been found in any other literature. Further studies should be carried out to identify the factors favoring the occurrence of this histological type. Grade III differentiation was present in 39.3% and stage 2 was encountered in 60.4%. In our series, the surgical management was done within an average of 3.1 months. This long surgical delay could be explained by the inability of our population, which is mostly housewives and farmers, to afford certain health services. The specific treatment was based on the tumor stage. At stages 0 and I, 12.0% of our patients had received only RTUV. In addition, at stage II, 66.3% of patients had undergone transurethral resection of the bladder, 96.6% of which was associated with postoperative local chemotherapy. This result differs from the series of Saadoune in 2019, and Mohammed in 2018 in Morocco where respectively 57% and 42.8% of patients benefited from BCG immunotherapy after transurethral resection [46, 47]. This divergence of practice would be justified by the unavailability of the attenuated form of BCG for instillations in our context. However, the use of mitomycin C for instillations is not always within reach of patients. At stage III, 66.6% of patients had undergone partial or total cystectomy associated with general chemotherapy, 50.0% of which was the MVAC protocol. As for stage IV, 22.2% of patients had undergone partial or total cystectomy associated with general chemotherapy. Protocols containing cisplatin salts including Gemcitabine-cisplatin and Cisplatin-Paclitaxel were used in 50.0% and 75.0% of these patients, respectively. This rate is higher than those of Kamissoko in 2014 in Mali and Abelhad in Morocco in 2011 where respectively 4.05% and 12.1% of patients had undergone polychemotherapy [10,48]. This practice is in full agreement with the recommendations of the Cancerology Committee of the French Association of Urology and the Association of Canadian Urologists [34, 49].
However, 70% of patients could not benefit from 3 complete cycles as recommended, this would be justified either by an altered general condition preventing continuation of this chemotherapy or by the expensive cost of chemotherapy in our context, although it is subsidized. No patient received radiotherapy. Regarding conservative surgery, 97.4% of patients benefited from it, and transurethral resection was the most used in 91.2% of patients. As for radical surgery, 8 patients benefited from it, of which 50.0% of cases were vesiculocystoprostatectomy. It was followed by a trans-intestinal ureterostomy in 83.3%. This technique was also the most used in the Hajjoubi series in Morocco in 2010 [50]. However, it was noted that 4.1% of patients chose to abstain from surgery either for impaired general condition and advanced tumor stage (2 patients) or for lack of financial means (3 patients). Palliative care was administered to patients with an impaired general condition. Touré, for his part, found surgical abstention also for the very poor general condition in 10.26% [25]. In our series, we recorded a comorbidity rate of 12.8% including 2 cases of grade IIIb according to Clavien-Dindo. Traoré et al in Senegal in 2018 and Touré in Mali in 2020 found a rate of 7.8% and 18.0% [25, 32]. This observation was different from that of Dehayni et al in Morocco in 2018 who found complications in 23.7% of patients [51]. This would be explained by the presence of numerous comorbidities in its study population, which for the most part was people over 65 years of age.
The median survival in our study was 59.9 months with a CI: [42.622-75.378]. Overall survival at 1 year was 83.1% with a mortality rate of 2.5%. At 3 years, overall survival was 59.8% with a mortality rate of 46.7%. This result is lower than that found by Ziani et al in Morocco in 2021 where the assessment of overall survival was 70.3% at 3 years [52]. At 5 years the overall survival was 12.3% with a mortality rate of 75.4%. This result is much lower than that of Giacalone et al in 2017 in the United States of America, Nagao et al 2017 and Ziani et al in Morocco in 2021 respectively 75%, 65% and 60.6% [52-54]. In general, it is clear that this aspect has been addressed by few developing countries, yet the prevalence there is also high. In our series, we note that overall survival is low and gradually regresses over time. This difference could be explained by the unequal availability of therapeutic modalities, difficult socioeconomic conditions and the insufficiency of an adequate technical platform. While these shortcomings are absent in developed countries.
References
- Simo RT, Cheunieu CN, Ahmadou M, et al. Influence of Prostate Cancer on Erectile Dysfunction in Northern Cameroon and Its Management. J Cancer Tumor Int 10 (2020): 7-15.
- Antoni S, Ferlay J, Soerjomataram I, et al. Bladder Cancer Incidence and Mortality: A Global Overview and Recent Trends. Eur Urol 71 (2017): 96-108.
- Colombel M, Soloway M, Hideyuki A, et al. Epidemiology, Staging, Grading, and Risk Stratification of Bladder Cancer European. Urology supplements 7 (2008): 618-626.
- Pfister C, Roupret M, Wallemand H, et al. Recommandations du comité de l’association française d’urologie AFU : recommandations en onco-urologie 2010. Tumeurs urothéliales. Prog urol 20 (2010): 255-274.
- Rebecca L, Siegel RL, Miller KD, et al. MPH et al. Cancer statistics, 2016. CA Cancer J Clin 66 (2016): 7-30.
- Uhry Z, Remontet L, Colonna M, et al. Cancer incidence estimation at a district level without a national registry: a validation study for 24 cancer sites using French health insurance and registry data. Cancer Epidemiol 37 (2013): 99-114.
- Rouprêt M, Neuzillet Y, Masson-Lecomte A, et al. CCAFU french national guidelines 2016-2018 on bladder cancer. Prog en Urol 27 (2016): 67-92.
- Roupret M, Seisen T. Tumeurs vésicales. Dans : Roupret M, Seisen T. Kb urologie. 4e Paris: Editions Vernazobres-grégo (2013): 123-130.
- Cussenot O, Ravery V. Classification et facteurs pronostiques des tumeurs épithéliales de la vessie. Encycl. Med Chir Néphrologie-Urologie mise a jour 18 (1995): 243.
- Kamissoko I. Epidemiological, clinical and therapeutic aspects of bladder tumors in the urology department of CHU Point G. [Thèse de médecine]. Bamako : University of Sciences, Techniques and Technologies of Bamako. N° 92 (2014).
- Mushtaq J, Thurairaja R, Nair R. Bladder Cancer. Surgery 37 (2019): 529-537.
- Saginala K, Barsouk A, Sukumar AJ, et al. Epidemiology of Bladder Cancer. Medical sciences 8 (2020): 15.
- Fiard G, Pavillet J. Le role de la, chimiothérapie dans le cancer de la vessie. Progres en urologie 25 (2015): 907-911.
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J Clin 68 (2018): 394-424.
- Ndahindwa V, Ngendahayo L, Vyankandondera J. Aspects epidemiologiques et anatomopathologiques des cancers dans les Centres Hospitaliers Universitaires (CHU) du Rwanda. Revue médical rwandaise 69 (2012): 40-49.
- Sow M, Nkégoum BB, Essame OJL, et al. Aspects épidémiologiques et histopathologiques des tumeurs urogénitales au Cameroun. Prog Urol 16 (2006): 36-39.
- Ndamba EPJ, Beyeme S, Moby HE, et al. Cancers urogénitaux dans la région du Littoral-Cameroun: épidémiologie et histopathologie. Revue de Médecine et de pharmacie 4 (2014): 440-446.
- Darre T, Amegbor K, Kpatcha M, et al. Urologic cancers in Togo: histo epidemiological profile of 678 cases. J Afr Cancer 6 (2014): 27-31.
- Badiaga C, Doumbia L, Sissoko F, et al. Epidemiological aspects of bladder tumors in the urology department of the CHU du point G about 185 cases.Uro’andro11 (2018).
- Salah R, Harir N, Zeggai S, et al. Cancers urologiques en Algérie : profil histoépidémiologique à propos de 348 cas. afri cancer 7 (2015): 126-131.
- Amin HAA, Kobaisi MH, Samir RM. Schistosomiasis and bladder cancer in Egypt: Truths and myths. Open Access Maced J Med Sci 7 (2019): 4023-4029.
- Inobaya MT, Olveda RM, Chau TN, et al. Prevention and control of schistosomiasis: a current perspective. Research and reports in tropical Medicine 5 (2014): 65-75.
- Fedewa SA, Soliman AS, Ismail K, et al. Incidence analyses of bladder cancer in the Nile delta region of Egypt. Cancer Epidemiol 33 (2009): 176-181.
- Saurabh Ch, Freddie B, Lortet-Tieulent J, et al. International Variations in Bladder Cancer Incidence and Mortality. European urology association 66 (2013): 57-73.
- Toure A. Aspects epidemiology, diagnosis and therapy of bladder tumors in the general surgery department of the Sominé Dolo hospital in Mopti. [Thèse de médecine]. Bamako : Université des Sciences, des Techniques et des Technologies de Bamako ; N°: (2020) :129.
- McBeth L, Grabnar M, Selman S, et al. Involvement of the Androgen and Glucocorticoid Receptors in Bladder Cancer. Int J Endocrinol 2015 (2015): 384860.
- Khaled HM, Aly MS, Magrath IT. Loss of Y Chromosome in Bilharzial Bladder Cancer. Cancer Genetics and cytogenetics 117 (2000): 32-36.
- Amiroune D. Cystectomies for bladder cancer: anatomopathological and operative data, oncological results, mortality and morbidity. medical thesis Rabat: faculty of medicine N° 1615 (2012).
- Owen HC, Giedl J, Wild PJ, et al. Low-frequency of epigenetic events in urothelial tumors in young patients. J Urol 184 (2010): 459-463.
- Iori F, De Dominicis C, Liberti M, et al. Superficial bladder tumours in patients under 40 years of age: Clinical, prognostic and cytogenetic aspects. Urol Int 67 (2001): 224-227.
- Engbang NPJ, Beyeme S, Moby HE, et al. Urinary bladder cancer in Cameroon: histoepidemiological aspects of 81 cases. Journal of medecine 2 (2016): 145-148.
- Traore MT, Jalloh M, Yevi M, et al. La résection transurétrale des tumeurs de vessie a l’hôpital général du Grand Yoff : à propos de 141 cas, Uro’Andro 1 (2018): 463-467.
- Lebret T, Herve JM, Yonneau L, et al. Etude de la survie après cystectomie pour cancer de vessie. A propos de 504 cas. Progrès en urologie 10 (2000): 553-560.
- Roupret M, Neuzillet Y, Pignot G, et al. Recommandations francaises du Comité de Cancérologie de l ’ AFU- Actualisation 2018-2020 : tumeurs de la vessie. Prog en Urol 28 (2020): 46-78.
- Boureima O, Tiennou H, Karama H, et al. Aspects Cliniques et Histologiques des Cancers de la Vessie au Centre Hospitalier Universitaire de Tengandogo (Ouagadougou) Clinical and histological presentation of bladder cancer : at the Tengandogo University Teaching Hospital (Ouagadougou) 21 (2020): 22-25.
- Bartlett JMS, Watters AD, Ballantyne SA, et al. Is chromosome 9 loss a marker of disease recurrence in transitional cell carcinoma of the urinary bladder? Br J Cancer 77 (1998): 2193-2198.
- Diao B, Amath T, Fall B, et al. Les cancers de vessie au Sénégal : particularités épidémiologiques, cliniques et histologiques Progrès en urologie. Prog Urol 18 (2008): 445-448.
- Berry A, Iriart X, Fillaux J, et al. Schistosomose urogénitale et cancer Urinary Schistosomiasis and Cancer. Bull Soc Pathol Exot 110 (2017): 68-75.
- Kadouri Y, Boualaoui I, Lachkar S, et al. Article Case series Carcinome épidermoïde de la vessie : expérience rétrospective dans un hôpital universitaire marocain et revue de la littérature 37 (2020): 1-7.
- Messing EM, Ralph M, Terry Y, et al. Long-term outcome of hematuria home screening for bladder cancer in men. Cancer 107 (2006): 2173-2179.
- Niang L, Ndoye M, Labou I, et al. Aspects épidémiologiques, cliniques et thérapeutiques des tumeurs de vessie à l’hôpital général de Grand Yoff de Dakar. Afr J Urol 20 (2014): 116.
- Pfister C, Roupret M, Neuzillet Y, et al. Recommandations en onco-urologie 2013 du CCAFU : Tumeurs de la vessie. Prog Urol 23 (2013): 105-125.
- Dobbs RW, Hugar LA, Revenig LM, et al. Incidence and clinical characteristics of lower urinary tract symptoms as a presenting symptom for patients with newly diagnosed bladder cancer. Int Braz J Urol 40 (2014): 198-203.
- Cherif M, Chakroun M, Bouzouita A, et al. Caractéristiques épidémiologiques du cancer de la vessie chez la femme en Tunisie. African Journal of Urology 22 (2016): 71-75.
- Management of bladder tumors in the urology department of the CHU Gabriel Toure. [Medical thesis] Bamako: Faculty of Medicine, Pharmacy and Odontostomatology. N° 101 (2012).
- Mohammed O. Bladder tumors in women (about 35 cases). [Medical thesis]. Morocco. Sidi Mohammed Ben Abdellah University. N° 024 (2018): 211.
- Saadoune M. Very high risk non-muscle infiltrating bladder tumors treated by cystectomy. [Medical thesis]. Marrakech: Cadi Ayyad University: Faculty of Medicine and Pharmacy. N° 212 (2019): 145.
- Abelhad M, Moudouni MS, Sarf I. Prognostic factors of infiltrating bladder tumours: comparison between 2 groups. [Medical thesis]. Marrakech: Cadi Ayyad University: Faculty of Medicine and Pharmacy. N° 212 (2011).
- Girish SK, Peter CB, Srikala SS, et al. Guide de pratique de l’Association des urologues du Canada: Cancer de la vessie avec envahissement musculaire. Can Urol Assoc J 13 (2019): 230-238
- Hajjoubi D, urinary diversions after cystectomy for infiltrating tumors of the bladder (about 41 cases). [Medical thesis] Rabat: Mohammed V University faculty of medicine and pharmacy -Rabat. No 177 (2010).
- Dehayni Y, Tetou M, Khdach Y, et al. L’âge avancé est-il un facteur de mauvais pronostic pour les patients atteints de tumeur de vessie infiltrant le muscle et traités par cystectomie ? Progres urologie 28 (2018): 166-172.
- Ziani I, Lahlou L, Ibrahimi A, et al. Etude de survie dans les tumeurs de la vessie infiltrant le muscle vésical chez la population marocaine en 2020. Revue d’épidémiologie et de santé publique 69 (2021): 46.
- Giacalone NJ, Shipley WU, Clayman RH, et al. Long-term outcomes after bladder-preserving trimodality therapy for patients with muscleinvasive bladder cancer: an updated analysis of the Massachusetts General Hospital experience. Eur Urol 71 (2017): 952-960.
- Nagao K, Hara T, Nishijima J, et al. The efficacy of trimodal chemoradiotherapy with cisplatin as a bladder-preserving strategy for the treatment of muscle-invasive bladder cancer. Urol Int 99 (2017): 446-452.
