Employment of 3D rotational fluoroscopy for neuro-navigated screw placement in the cervical spine
Article Information
Nora Conrads 1,*, Timo Michael Heintel1, Philipp Feldle1, Andreas Steven Kunz1, Katharina Grunz1, Thorsten Alexander Bley1, Stefan Köhler1, Thomas Westermaier1, Jan-Peter Grunz1
1University Hospital Wuerzburg
*Corresponding Author: Nora Conrads, University Hospital Wuerzburg, Germany
Received: 19 October 2022; Accepted: 27 October 2022; Published: 09 December 2022
Citation: Nora Conrads, Timo Michael Heintel, Philipp Feldle, Andreas Steven Kunz, Katharina Grunz, Thorsten Alexander Bley, Stefan Köhler, Thomas Westermaier, Jan-Peter Grunz. Employment of 3D rotational fluoroscopy for neuro-navigated screw placement in the cervical spine. Journal of Surgery and Research 4 (2022): 114-120.
Share at FacebookAbstract
Purpose:
Pinpoint instrumentation is pivotal in cervical spine surgery in order to protect sensitive structures such as spinal cord or vertebral arteries. The aim of this study was to investigate the accuracy of neuro-navigated rotational fluoroscopy-guided screw positioning in the cervical spine employing a novel classification system.
Methods:
In procedures of dorsal cervical spine stabilization screw positions documented by rotational fluoroscopy were retrospectively evaluated. Accuracy of screw placement was analyzed using a new eight-grade scoring system with particular attention to the spinal canal, neuroforamina, and vertebral arteries. In addition, intra- and postoperative revision rates, as well as clinical and neurological outcome were evaluated.
Results:
One-hundred-forty-five patients with dorsal stabilization of the cervical spine were included. Of the 925 screws placed, 877 (94.8%) showed optimal positioning in the primary 3D image control. Differentiating between less and more than 50% of the screw diameter, 15 (1.6%) and 2 screws (0.2%) protruded into the transverse foramen. The pedicle or lateral mass were exceeded craniocaudally by 8 (≤50%: 0.9%) and 3 screws (>50%: 0.3%), respectively. Laterally, the pedicle or mass was exceeded substantially by 6 screws (0.6%). Medially, 8 (≤50%: 0.9%) vs. 6 screws (>50%: 0.6%) exceeded the wall of the pedicle or lateral mass. No patient underwent secondary surgery due to initial screw mispositioning. An improvement of the preoperatively indicated pain levels was documented in 87 of 114 patients (76.3%) with adequate follow-up.
Conclusions:
Neuro-navigation based on intraoperative 3D fluoroscopy facilitates high accuracy of screw positioning for posterior stabilization of the cervical spine.
Keywords
pedicle screws; lateral mass screws; fluoroscopy; neuro-navigation; cervical spine
pedicle screws articles pedicle screws Research articles pedicle screws review articles pedicle screws PubMed articles pedicle screws PubMed Central articles pedicle screws 2023 articles pedicle screws 2024 articles pedicle screws Scopus articles pedicle screws impact factor journals pedicle screws Scopus journals pedicle screws PubMed journals pedicle screws medical journals pedicle screws free journals pedicle screws best journals pedicle screws top journals pedicle screws free medical journals pedicle screws famous journals pedicle screws Google Scholar indexed journals lateral mass screws articles lateral mass screws Research articles lateral mass screws review articles lateral mass screws PubMed articles lateral mass screws PubMed Central articles lateral mass screws 2023 articles lateral mass screws 2024 articles lateral mass screws Scopus articles lateral mass screws impact factor journals lateral mass screws Scopus journals lateral mass screws PubMed journals lateral mass screws medical journals lateral mass screws free journals lateral mass screws best journals lateral mass screws top journals lateral mass screws free medical journals lateral mass screws famous journals lateral mass screws Google Scholar indexed journals fluoroscopy articles fluoroscopy Research articles fluoroscopy review articles fluoroscopy PubMed articles fluoroscopy PubMed Central articles fluoroscopy 2023 articles fluoroscopy 2024 articles fluoroscopy Scopus articles fluoroscopy impact factor journals fluoroscopy Scopus journals fluoroscopy PubMed journals fluoroscopy medical journals fluoroscopy free journals fluoroscopy best journals fluoroscopy top journals fluoroscopy free medical journals fluoroscopy famous journals fluoroscopy Google Scholar indexed journals neuro-navigation articles neuro-navigation Research articles neuro-navigation review articles neuro-navigation PubMed articles neuro-navigation PubMed Central articles neuro-navigation 2023 articles neuro-navigation 2024 articles neuro-navigation Scopus articles neuro-navigation impact factor journals neuro-navigation Scopus journals neuro-navigation PubMed journals neuro-navigation medical journals neuro-navigation free journals neuro-navigation best journals neuro-navigation top journals neuro-navigation free medical journals neuro-navigation famous journals neuro-navigation Google Scholar indexed journals cervical spine articles cervical spine Research articles cervical spine review articles cervical spine PubMed articles cervical spine PubMed Central articles cervical spine 2023 articles cervical spine 2024 articles cervical spine Scopus articles cervical spine impact factor journals cervical spine Scopus journals cervical spine PubMed journals cervical spine medical journals cervical spine free journals cervical spine best journals cervical spine top journals cervical spine free medical journals cervical spine famous journals cervical spine Google Scholar indexed journals neoplasms articles neoplasms Research articles neoplasms review articles neoplasms PubMed articles neoplasms PubMed Central articles neoplasms 2023 articles neoplasms 2024 articles neoplasms Scopus articles neoplasms impact factor journals neoplasms Scopus journals neoplasms PubMed journals neoplasms medical journals neoplasms free journals neoplasms best journals neoplasms top journals neoplasms free medical journals neoplasms famous journals neoplasms Google Scholar indexed journals traumatic articles traumatic Research articles traumatic review articles traumatic PubMed articles traumatic PubMed Central articles traumatic 2023 articles traumatic 2024 articles traumatic Scopus articles traumatic impact factor journals traumatic Scopus journals traumatic PubMed journals traumatic medical journals traumatic free journals traumatic best journals traumatic top journals traumatic free medical journals traumatic famous journals traumatic Google Scholar indexed journals cervical screw placement articles cervical screw placement Research articles cervical screw placement review articles cervical screw placement PubMed articles cervical screw placement PubMed Central articles cervical screw placement 2023 articles cervical screw placement 2024 articles cervical screw placement Scopus articles cervical screw placement impact factor journals cervical screw placement Scopus journals cervical screw placement PubMed journals cervical screw placement medical journals cervical screw placement free journals cervical screw placement best journals cervical screw placement top journals cervical screw placement free medical journals cervical screw placement famous journals cervical screw placement Google Scholar indexed journals pedicle screw articles pedicle screw Research articles pedicle screw review articles pedicle screw PubMed articles pedicle screw PubMed Central articles pedicle screw 2023 articles pedicle screw 2024 articles pedicle screw Scopus articles pedicle screw impact factor journals pedicle screw Scopus journals pedicle screw PubMed journals pedicle screw medical journals pedicle screw free journals pedicle screw best journals pedicle screw top journals pedicle screw free medical journals pedicle screw famous journals pedicle screw Google Scholar indexed journals neuro-navigation articles neuro-navigation Research articles neuro-navigation review articles neuro-navigation PubMed articles neuro-navigation PubMed Central articles neuro-navigation 2023 articles neuro-navigation 2024 articles neuro-navigation Scopus articles neuro-navigation impact factor journals neuro-navigation Scopus journals neuro-navigation PubMed journals neuro-navigation medical journals neuro-navigation free journals neuro-navigation best journals neuro-navigation top journals neuro-navigation free medical journals neuro-navigation famous journals neuro-navigation Google Scholar indexed journals
Article Details
Introduction
Due to demographic change, with a growing proportion of older people and a longer life expectancy, an increase in the incidence of spinal diseases is anticipated, especially in elderly patients who are particularly susceptible to pathologies of the spine. In addition to degenerative changes, local and systemic inflammation, as well as neoplasms, traumatic injuries in particular can be the cause of instability in the cervical spine, often necessitating surgical intervention [1,2]. The primary goal of cervical spine surgery, in addition to restoring stability, is to protect sensitive structures like the spinal cord, exiting nerve roots or the vertebral arteries. To minimize the risk of misplacement and subsequently higher incidence of neurological and vascular complications, a high degree of intraoperative precision is required [3,4]. Native x-ray diagnostics (2D or biplanar fluoroscopy) continue to represent the standard of reference for intraoperative imaging in a variety of procedures, including spinal instrumentation [5]. Although conventional radiographic imaging allows for identification of the surgical area of interest and of the targeted insertion points, intraoperative verification of correct implant positioning can pose a significant challenge [5]. The fundamental advantage of navigated spinal surgery lies in the ability to track the surgical instrument in "real time" and to constantly visualize its position by fusion with preoperative CT or MRI, including three-dimensional visualization of critical structures. In combination with the use of anatomical landmarks, neuro-navigation provides a valuable orientation aid for the positioning of pedicle (PS) and lateral mass screws (LMS) [6,7].
We employed a novel classification system to investigate the accuracy of neuro-navigated rotational fluoroscopy for guiding screw positioning in the cervical spine. We hypothesized that the use of intraoperative 3D imaging would allow for excellent accuracy, while allowing for immediate revision of misplaced screws instead of secondary surgery.
Material and Methods
Approval for this retrospective study was obtained from the local institutional review board. Additional written informed consent was not required due to the retrospective nature of the investigation. The clinical information system (i.s.h. med., Cerner Corporation, North Kansas City, USA) provided data regarding patient history and the corresponding surgical intervention, which were subsequently anonymized for further evaluation. Preoperative and postoperative pain scores and information on the presence or absence of neurologic symptoms were extracted from available outpatient clinic notes. For this analysis, patients who underwent dorsal cervical spine stabilization by screw-rod system using 3D fluoroscopic navigation (O-arm, Medtronic, Dublin, Ireland) at our neurosurgical department between June 2010 and June 2015 were eligible. Surgical indications resulted from spinal instability due to degenerative, traumatic, inflammatory, or tumor-related conditions. Inclusion criteria for this study were an open surgical technique (± additional fusion) and at least one intraoperative 3D fluoroscopy scan after screw-rod system insertion to verify screw positions. The lack of a 3D scan after dorsal instrumentation constituted an exclusion criterion from this study.
3D image acquisition
The scanner architecture of the O-arm allows for preoperative planning, intraoperative imaging and postoperative evaluation by using 3D rotational fluoroscopy. The gantry-based scanning unit consists of an x-ray source (B100, Varian Medical Systems, Palo Alto, USA) and a 30 cm x 40 cm flat panel detector (PaxScan 4030D, Varex, Palo Alto, USA). In 3D mode, the O-arm generates projection data during a full 360° rotation. The system rotates at 30° per second ("standard mode") or 15° per second ("high-definition mode") and produces up to 400 or 750 images, respectively, over the course of a 360° rotation. By means of navigation system integration (StealthStation S7, Medtronic), images acquired intraoperatively can be used directly for neuro-navigation. This allows for identification of the targeted entry points, while also facilitating detailed visualization of adjacent anatomical structures. Furthermore, the position control of the stabilization system after instrumentation and thus the technical success of the surgical intervention can be documented while the patient is still in the operating room.
Classification system
Adapting the established classification of Zdichavsky et al. for the thoracic and lumbar spine, this study evaluates screw positions after dorsal stabilization of the cervical spine with an eight-score system [8,9]. The proposed classification system describes the screw placement in the pedicle or lateral mass with particular focus on medial, lateral, caudal, or cranial deviation from the optimal position.
|
Grading |
Criteria |
|
Ia |
³ half of the screw diameter within the pedicle or lateral mass |
|
Ib |
> half of the screw diameter laterally outside of the pedicle or lateral mass |
|
IIa |
£ half of the screw diameter within the transverse foramen |
|
IIb |
£ half of the screw diameter within the transverse foramen£ half of the screw diameter exceeds the pedicle or lateral mass cranially or caudally |
|
IIc |
£ half of the screw diameter medially outside of the pedicle or lateral mass |
|
IIIa |
> half of the screw diameter within the transverse foramen |
|
IIIb |
> half of the screw diameter exceeds the pedicle or lateral mass cranially or caudally |
|
IIIc |
> half of the screw diameter medially outside the pedicle or lateral mass |
Table 1: Classification for cervical screw placement
For grading of screw positions in the cervical spine, the established classification of Zdichavsky et al. for
thoracic and lumbar spine instrumentation was modified[8,9]
The individual scores are explained in Table 1 and for visualization purposes, schematic illustrations of each grading are presented in Figure 1. Screws classified as Ia were deemed to be in excellent position and provide optimal stability, whereas screws classified as IIIa, IIIb, and IIIc were considered to be severely mispositioned. Due to potentially resulting in neurological symptoms and decreased spinal stability, surgical revision is usually advised in grade III screw placement [10].
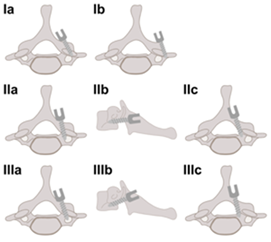
Figure 1
Schematic drawing of the proposed classification system for grading screw placement in the cervical spine with lateral mass screws. Classification of pedicle screw positioning was performed analogously
In addition to evaluating the position in the pedicle or lateral mass, relative screw length was expressed as a percentage of the total transosseous access length up to the respective bone margin or limiting structure (transverse foramen, spinal canal, vertebral artery). A relative transosseous screw length between 85% and 100% was considered as satisfactory (Figure 2) [11].
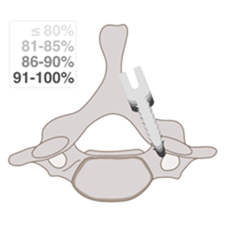
Figure 2 : Schematic display of relative screw length. Screw lengths between 100% and 85% are classified as "good”
Data evaluation and statistical analysis
The evaluation of intraoperative imaging in terms of screw position and length was performed using dedicated DICOM viewer software (OsiriX, Bernex, Switzerland). Data analyses were performed with statistical software (IBM SPSS Statistics, Armonk, USA). Normal distribution was ascertained by means of the Kolmogorov-Smirnov test. Normally distributed data are reported as mean value and standard deviation, otherwise results are presented as absolute values and percentage distribution.
One-hundred-forty-five patients (99 men, 68.3%) underwent dorsal instrumentation of the cervical spine by screw-rod system using O-arm-controlled neuro-navigation. On average, 3.2 ± 1.3 vertebral bodies were fused, with the cervical vertebra C3 being the most frequently one stabilized (84 times) and the cervical vertebra C7 (52 times) the rarest. At the time of surgery, mean patient age was 65.3 ± 14.1 years. The most common cause indicating surgical treatment was traumatic injury (71 patients, 47.3%). Other conditions requiring screw-rod stabilization comprised degeneration (55 patients, 36.7%), malignancy (22 patients, 14.7%), and inflammatory diseases (2 patients, 1.4%).
Screw positioning in 3D rotational fluoroscopy is visualized in Figure 3.
Of 925 screws inserted, 739 were lateral mass screws (79.9%) and 186 pedicle screws (20.1%). Overall, 877 (94.8%) showed an optimal position (grade Ia according to the proposed classification system) in the primary 3D fluoroscopy control. Discerning between screw protrusion into the transverse foramen of less (IIa) versus more than 50% of the screw diameter (IIIa), 15 (1.6%) versus 2 screws (0.2%) fulfilled the respective criteria. Craniocaudal displacement of less than (IIb) and more than one half of the screw diameter (IIIb) was ascertained in 8 (0.9%) and 3 screws (0.3%), respectively. Laterally, the pedicle or lateral mass was exceeded by more than 50% (Ib) of 6 screws (0.7%). Medial protrusion of less than one half of the screw diameter (IIc) was documented in 8 screws (0.9%), whereas 6 screws (0.7%) showed full medial displacement (IIIc). The average screw length in relation to the maximum possible transosseous access length was 89.5% ± 9.5%, with 603 (65.2%) of the evaluable screws being classified as "good" (between 85-100% of maximum possible length). After intraoperative revision of 33 screws, 31 were classified as Ia (93.9% of revised screws), one screw as IIa (prior to revision: IIIa), and one as IIc (prior to revision: IIIc). Six screws with mispositioning in relation to the neuroforamen (4 times IIb, 2 times IIIb) could be revised intraoperatively to result in optimal placement. After revision, 615 screws (66.5%) screws had a good relative length. Figure 4 and Figure 5 summarize the classification of screw positions and screw length before and after intraoperative revision. No patient required follow-up surgery due to primary screw mispositioning.
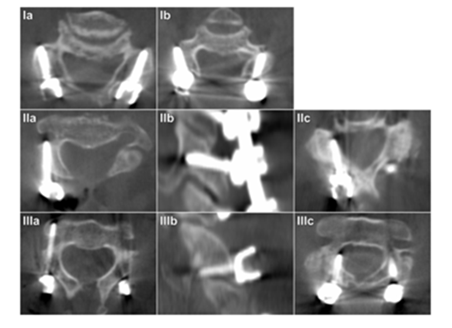
Figure 3
Intraoperative fluoroscopy images of lateral mass screw placement in the cervical spine. In each of the presented cases, the right screw represents the respective classification entry.
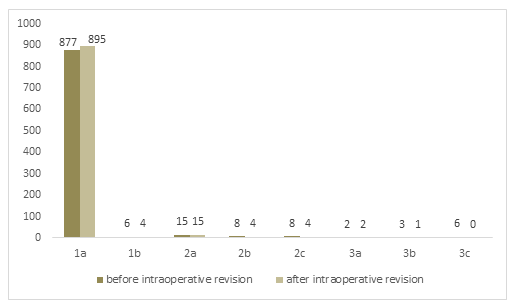
Figure 4
Absolute frequencies of screw position grading in dorsal instrumentation of the cervical spine before and after intraoperative revision of 33 screws
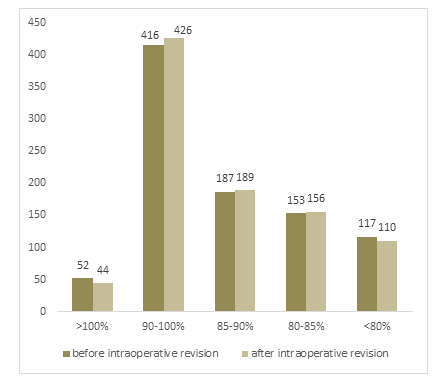
Figure 5
Evaluation of relative screw length before and after intraoperative revision of 33 screws. Screw length between 100% and 85% is considered "good"
As 36 patients did not undergo clinical follow-up, clinical outcome could be determined in 119 patients with a mean follow-up period of 14.4 ± 8.9 months. Of these, 83 patients reported 114 pain events in the form of neck, arm or back pain. In 76.3% of the cases, pain was reported to have disappeared completely or at least to have improved significantly after surgery. In 4 cases, pain was recorded to have aggravated or to have newly developed after surgery. Within the 79 individuals with dedicated neurologic follow-up, 50 patients reported no or significantly improved neurologic symptoms postoperatively.
Discussion
In this investigation, the accuracy of pedicle and lateral mass screw positioning with neuro-navigation based on intraoperative 3D rotational fluoroscopy in the cervical spine of 145 patients was analyzed retrospectively. Within the complex and in part miniscule anatomy that surgeons are faced with, excellent precision regarding implant positioning and screw length could be shown.
To our knowledge, there is neither an established classification system for screw positions in the cervical spine nor a consistent definition of screw mispositions in the context of cervical stabilization. Especially regarding screw displacement, various attempts within the published literature have introduced different descriptions of "correct" screw positioning. While some authors report only the absolute extent of screw deviation regardless of orientation, others describe only the presence or absence of misplacement in dichotomous fashion. In some studies, only screws causing a postoperative neurological deficit or requiring postoperative revision are considered to be inaccurately positioned [12–14]. This inconsistency limits comparability of the literature and complicates the discussion of individual results. The classification of Zdichavsky et al. is among the most established grading systems for determining the accuracy of screw placement in the thoracic and lumbar spine. While excluding stabilization of the cervical spine, this classification takes into account that information regarding stability and the risk for neurological and vascular complications can be derived from both the orientation and the extent of screw malpositioning [8,9]. Acknowledging the advantages of multidirectional screw position assessment, we modified Zdichavsky's classification for application in the cervical spine, thus rendering it applicable not only for PS but also for LMS.
In the present study, particular emphasis was placed on the assessment of clinical and neurological effects of cervical spine surgery. With a mean follow-up period of 14.4 ± 8.9 months, long-term postoperative symptom relief could be demonstrated in the vast majority of patients. In combination with an extensive proportion of optimally placed PS and LMS screws, this underlines the added value of intraoperative rotational 3D fluoroscopy on the clinical outcome. Although Rajan et al. reported the absence of neurological or vascular complications despite suboptimal screw positioning under neuro-navigation in 9.2% of their cohort [15], this observation does not diminish the value of obtaining precise information regarding the implant’s position while the patient is still in the operating room. With 33 screws revised intraoperatively based on imaging results in our study, we believe that the prevention of secondary surgeries or symptom deterioration due to persisting screw misplacement constitutes a major advantage for patients.
Limitations
Several limitations have to be acknowledged for the presented work. Due to the retrospective study design and patient data being collected over a five-year period, the quality and quantity of clinical and neurological follow-up was heterogenous. Since the time interval of data inclusion contained the introductory phase of the rotational fluoroscopy system, intraoperative revision rates may be different in the present day. Finally, the combination of screw-rod fixation with cervical fusion in a portion of the study group may have affected the patient outcome.
Conclusion
Neuro-navigation based on rotational 3D fluoroscopy for posterior stabilization of the cervical spine facilitates high accuracy for screw placement and satisfactory patient outcome. Intraoperative access to cross-sectional image information allows for identification and revision of incorrect screw positions while the patient remains in the operating room, thus preventing repeated surgical procedures.
Declarations
Ethics approval and consent to participate
The local institutional review board approved this retrospective study and waived the need for additional written informed consent (reference number 20160925 01). This work was carried out in accordance with the ethical standards of the institutional and national research committee and with the 1975 Declaration of Helsinki.
Consent for publication
Not applicable.
Availability of data and materials
The datasets generated and/or analyzed during this study are not publicly available as DICOM headers contain patient information. Data can be obtained on reasonable request from the corresponding author.
Conflicts of interest/Competing interests
The authors declare that they have no competing interests.
Funding
JPG was funded by the Interdisciplinary Center of Clinical Research Würzburg, Germany [grant number Z-2/CSP-06]. This publication was supported by the Open Access Publication Fund of the University of Wuerzburg.
Author Contributions
NC analyzed all data and prepared the manuscript. 3D fluoroscopy imaging was assessed by SK and TW. KG provided the schematic drawings and supported figure preparation. PF and JPG conducted statistical analyses. ASK supported data acquisition and revised the manuscript. TMH contributed to the preparation of the manuscript. TMH and TAB provided quality control. JPG supervised the study and was a major contributor to the preparation of the manuscript. All authors read and approved the final manuscript.
References
- Boskey A L, Imbert L (2017) Bone quality changes associated with aging and disease: a review. Ann N Y Acad Sci 1410: 93.
- Sobottke R, Csécsei G, Kaulhausen T, et al (2008) Wirbelsäulenchirurgie bei patienten in höherem lebensalter. Sind operative eingriffe an der alternden wirbelsäule komplikationsträ chtig? Orthopade 37: 367-373.
- Ghasem A, Sharma A, Greif D N, et al (2018) The Arrival of Robotics in Spine Surgery. Spine (Phila Pa 1976) 43: 1670–1677.
- Kothe R, Richter M (2018) Relevanz der spinalen Navigation in der rekonstruktiven Halswirbelsäulenchirurgie. Orthopade 47: 518–525.
- von Rüden C, Trapp O, Augat P, et al (2020) Evolution of imaging in surgical fracture management. Injury 51:S51–S56.
- Scheufler K M, Franke J, Eckardt A, Dohmen H (2011) Accuracy of image-guided pedicle screw placement using intraoperative computed tomography-based navigation with automated referencing, part I: Cervicothoracic spine. Neurosurgery 69: 782-795.
- Ishikawa Y, Kanemura T, Yoshida G, et al (2010) Clinical accuracy of three-dimensional fluoroscopy-based computer-assisted cervical pedicle screw placement: A retrospective comparative study of conventional versus computer-assisted cervical pedicle screw placement - Clinical article. J Neurosurg Spine 13: 606–611.
- Zdichavsky M, Blauth M, Knop C, et al (2004) Accuracy of pedicle screw placement in thoracic spine fractures - Part I: Inter- and intraobserver reliability of the scoring system. Eur J Trauma 30: 234-240.
- Zdichavsky M, Blauth M, Knop C, et al (2004) Accuracy of pedicle screw placement in thoracic spine fractures - Part II: A retrospective analysis of 278 pedicle screws using computed tomographic scans. Eur J Trauma 30: 241-247.
- Mao J Z, Agyei J O, Ghannam M M, et al (2021) Navigation-Guided Subaxial Cervical Pedicle Screws in Revision Spine Surgery: 2-Dimensional Operative Video. Oper Neurosurg 20: 312-313.
- Heintel T M, Berglehner A, Meffert R (2013) Accuracy of percutaneous pedicle screws for thoracic and lumbar spine fractures: A prospective trial. Eur Spine J 22: 495-502.
- Rath S A, Moszko S, Schäffner P M, et al (2008) Accuracy of pedicle screw insertion in the cervical spine for internal fixation using frameless stereotactic guidance. J Neurosurg Spine 8: 237-245.
- Kotani Y, Abumi K, Ito M, Minami A (2003) Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg 99: 257-263.
- Shi H, Zhu L, Ma J, et al The accuracy of a novel pedicle screw insertion technique assisted by a special angular scale in the subaxial cervical spine using lateral mass as a reference marker.
- Rajan V V, Kamath V, Shetty A P, Rajasekaran S (2010) Iso-C3D navigation assisted pedicle screw placement in deformities of the cervical and thoracic spine. Indian J Orthop 44: 163-168.
