Elevated Troponin- Is it Time to Consult A Cardiologist? A Case Series with Review of the Literature
Article Information
Priyanka Parajuli, MD1*, Manjari Rani Regmi, MD1, Odalys Estefania Lara-Garcia, MD1, Ruby Maini, MD1, Mukul Bhattarai, MD2, Alan Deckard, MD1, Abhishek Kulkarni, MD2
1Department of Internal Medicine, Southern Illinois University School of Medicine, 801 North Rutledge Street
Springfield, Illinois, 62703, USA
2Division of Cardiology, Department of Internal Medicine, Southern Illinois University School of Medicine, Springfield, IL 62702, USA
*Corresponding Author: Priyanka Parajuli, Department of Internal Medicine, Southern Illinois University School of Medicine, 801 North Rutledge Street Springfield, Illinois, 62703, USA
Received: 15 June 2020; Accepted: 25 June 2020; Published: 30 June 2020
Citation: Priyanka Parajuli, Manjari Rani Regmi, Odalys Estefania Lara-Garcia, Ruby Maini, Mukul Bhattarai, Alan Deckard, Abhishek Kulkarni. Elevated Troponin- Is it Time to Consult A Cardiologist? A Case Series with Review of the Literature. Cardiology and Cardiovascular Medicine 4 (2020): 268-277.
Share at FacebookAbstract
Cardiac troponin (cTn) is the preferred blood test utilized in the evaluation of acute coronary syndrome (ACS). Elevated cTn represents the presence of myocardial injury but not the cause. As new high sensitivity troponin assays become available, subtle cardiac injuries are being detected. The number of patients encountered with elevated troponin have therefore increased. It is now understood that non-coronary diseases can lead to elevated troponin. There are no specific management guidelines for patients with elevated troponin without a concomitant ACS. Treatment of underlying medical conditions remains the cornerstone of therapy in such patients. Therefore, differentiating elevated troponin secondary to ACS versus non-ACS causes is paramount in order to provide timely and appropriate intervention. In this paper, we discuss a series of cases presenting with elevated troponin, explore non-ACS troponin-elevating conditions along with their underlying pathophysiology, and provide a simple approach to determine the need for cardiology consultation.
Keywords
Troponin; Acute coronary syndrome; NSTEMI; STEMI; Cardiology; Inpatient
Article Details
Introduction
Cardiac troponin (cTn) replaced creatinine kinases (CK-MB) in 2000 and remains the preferred biochemical marker in aiding the diagnosis of myocardial ischemia (MI) [1]. cTn is the most sensitive and specific marker of myocardial injury and is routinely ordered for patients who present with symptoms of myocardial ischemia including chest pain, dyspnea, and syncope. Although elevated troponin denotes myocardial injury, it does not distinguish the underlying reason for the injury [1]. Multiple studies have discussed the various conditions leading to elevated troponin, including ACS and non-ACS diseases [1-4]. Consequently, it is vital that the elevated troponin level be interpreted in conjunction with symptoms, clinical findings, electrocardiography (EKG) results, and patients’ underlying comorbidities. Yet, in a hospital setting it is a common practice to request a cardiology consultation for elevated troponin which might not be warranted. In this paper, we will discuss differential diagnoses, expected clinical findings and diagnostic approaches in various medical conditions that present with elevated troponin. We hope our discussion will assist healthcare professionals in managing inpatients with elevated troponin. We will begin with brief clinical scenarios that will help demonstrate the heterogeneity of patients that present with elevated troponin.
Case 1: A 28-year-old male with no known past medical history was admitted with several days of diffuse constant chest pain that subsequently radiated to the neck for one day following recent upper respiratory symptoms. No diaphoresis, dyspnea, or nausea were reported. EKG revealed no acute ischemic changes. Erythrocyte sedimentation rate (ESR) and c-reactive protein (CRP) were elevated at 37 mm/hr and 44mg/L, respectively. Troponin was elevated at 13.4 ng/mL initially and peaked at 15 ng/mL. A transthoracic echocardiogram (TTE) revealed a decreased ejection fraction of 40-45% with global hypokinesis. Cardiac MRI showed abnormal delayed enhancement in a non-ischemic distribution within the anterior, lateral and inferior segments of the left ventricle with a pattern consistent with myocarditis. The patient received supportive management and made a complete recovery.
Case 2: A 59-year-old female with a past medical history of end stage renal disease (ESRD) and breast cancer, status post bilateral mastectomy two weeks prior to the date of admission presented with a 2-day history of constant left sided pressure-like chest pain radiating to her left arm and shoulder. The pain was rated as 6/10. Initial EKG revealed normal sinus rhythm. Troponin was elevated at 0.16 ng/mL that subsequently peaked at 1.5 ng/ml. A left heart catheterization revealed non-obstructive coronary artery disease without a culprit lesion. The patient’s elevated troponin was attributed to underlying ESRD. She was dialyzed and discharged on optimal medical therapy.
Case 3: A 94-year-old female with a past medical history of coronary artery disease (CAD), recent multivessel percutaneous intervention, severe aortic stenosis, severe mitral regurgitation and moderate tricuspid regurgitation presented with a one-day history of shortness of breath. Admission B-type natriuretic peptide (BNP) was noted to be elevated at 2030 pg/mL (reference range: 0-72 pg/mL). Troponin at presentation was 0.07 ng/ml. Subsequent measurement of troponin was stable at 0.05 ng/mL. EKG revealed normal sinus rhythm. Chest X-ray revealed pulmonary edema. A limited echocardiogram revealed severe aortic valve stenosis with an aortic peak valve velocity of 4.13 m/s, peak gradient of 68.1 mmHg, mean gradient of 43.4 mmHg and an aortic valve area of 0.76 cm2. Left ventricular ejection fraction (LVEF) was noted to be 60-65%. Vigorous diuresis resulted in relief of symptoms. Her elevated troponin was attributed to decompensated heart failure, which was medically managed. She underwent a transcatheter aortic valve replacement within a month of discharge.
Case 4: A 60-year-old female with a history of hypertension, type 2 diabetes mellitus, deep vein thrombosis, pulmonary embolism, and severe peripheral vascular disease was admitted for sepsis. EKG revealed atrial fibrillation with a heart rate of 118. The patient’s troponin was elevated at 0.21 ng/mL and subsequently trended down to 0.16 ng/mL. An echocardiogram revealed atrial fibrillation with LVEF of 54%. No wall motion abnormalities were noted. Her CHA2DS2-VASc score was calculated at 6 implying 9.7% annual risk of stroke. Her elevated troponin was attributed to atrial fibrillation, which was treated with beta-blockers to attain adequate rate control. Direct oral anticoagulant therapy was started given the elevated risk of cerebrovascular accident (CVA)/ transient ischemic attack (TIA).
Case 5: A 34-year-old female with a history of paraplegia secondary to granulocytic sarcomas (GS), type 2 diabetes mellitus, and neurogenic bladder with a chronic indwelling foley catheter presented to the emergency department with altered mental status. Upon initial evaluation she was found to have hypotension, tachycardia, hyperkalemia, and leukocytosis. Her initial troponin was elevated at 0.95 ng/mL and later peaked at 1.32 ng/mL. An EKG revealed sinus tachycardia and echocardiography was unremarkable. Urinalysis was positive for nitrites, leukocyte esterase, and bacteria and highly suggestive of an underlying urinary tract infection. The patient was admitted to the intensive care unit (ICU) and was treated for sepsis with fluids and antibiotics. Her elevated troponin was attributed to the underlying sepsis.
General pathophysiology of troponin elevation in individuals
Cardiac myocytes subjected to hypoxia from ischemic events leads to reversible myocyte injury in an early phase, and myocardial necrosis if ischemia is prolonged. Myofibril-bound cytosolic complexes are released through the necrosed myocyte cell membrane [5]. The underlying membrane damage to ischemic myocytes causes troponin to leak into the circulation. Although myocardial injury and necrosis remain the most common cause of significantly elevated troponin, it is important to acknowledge other mechanisms that lead to troponin release into the circulation. For instance, the patient described in case 5 above had an elevated troponin in the setting of sepsis without any evidence of wall motion abnormality on a TTE. It is theorized that sepsis results in the release of myocardial depressive factors causing increased myocyte membrane permeability [6]. Troponins, thus become detectable in blood of such patients. Similarly, heart failure increases preload. It is hypothesized that the increased preload causes increased turnover of myocytes and myocyte cell death (apoptosis) causing elevated troponin as described in case 3 above [7, 8]. Other mechanisms that have been explored to explain elevated troponin in various clinical scenarios include myocardial wall stress, increased release of inflammatory cytokines and catecholamines, and direct cellular injury [4]. Low levels of cardiac troponins can be found circulating in patients with stable ischemic heart disease (SIHD) and in populations who have high cardiovascular disease risk factors and comorbidities [9, 10]. A precise pathophysiology is not understood for the aforementioned diseases. Table 1 explains various types of troponin along with their detection values in the serum.
|
Types |
Activity |
Muscle |
Detection |
|
|
Troponin C |
Senses calcium and initiate muscle contraction |
Cardiac and skeletal muscles |
||
|
Cardiac Troponin (cTn) |
Troponin T (cTnT) |
Control calcium mediated interaction between actin and myosin |
Myocardium and small portion from skeletal muscle |
- Single assay (results can be compared among laboratories) -Cut off value of 0.1 mg/ L indicates myocardial injury |
|
Troponin I (cTnI) |
Only in myocardium |
-Several assays with differing sensitivities and cutoff values -Cut off value determined by each laboratory at the 99th percentile of normal |
||
Table 1: Various types of troponins along with their values for detection in the serum[11, 12]
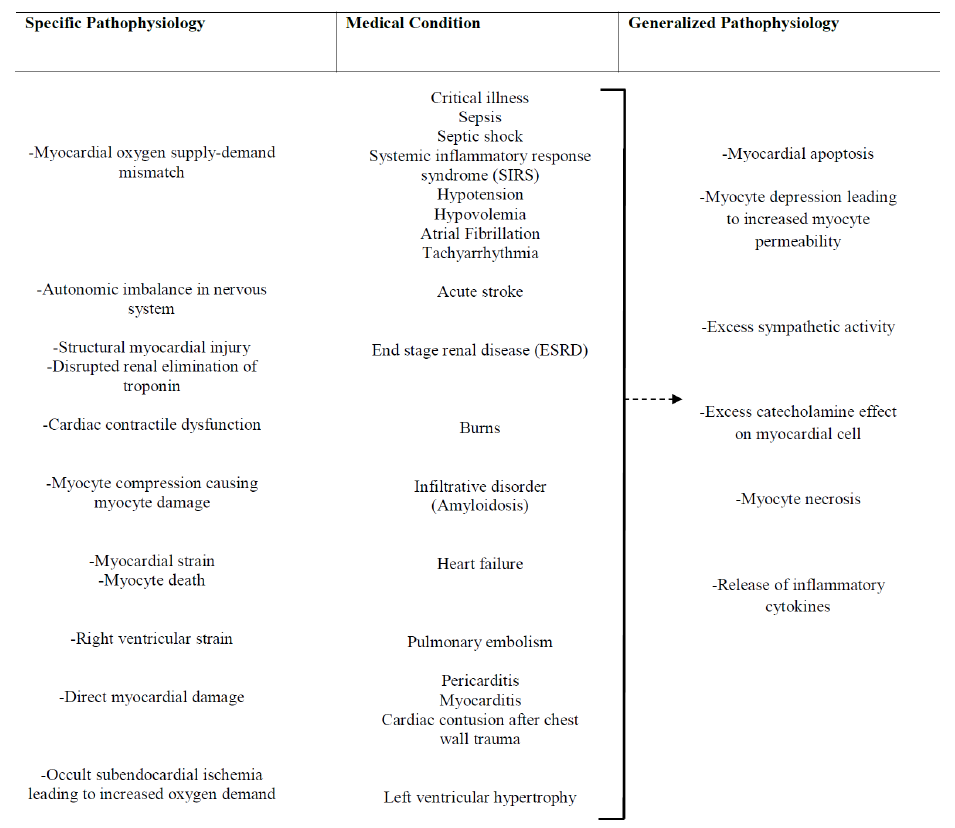
In table 2, we have diagrammed multiple non-ACS diseases that can present with elevated troponin with their underlying mechanisms for troponin release.
Management of elevated troponin
Elevated troponin should always be interpreted in a clinical context and emphasis should be placed on understanding the underlying pathology leading to it since intervention is based on the underlying cause. It is of utmost importance that when troponins are obtained and trended in an individual, the pretest probability of ACS is intermediate to high, so that appropriate and timely intervention can be performed. ACS, comprised of non-ST segment elevation myocardial infarction (NSTEMI), ST segment elevation myocardial infarction (STEMI), and unstable angina can cause elevated troponin. These conditions warrant immediate cardiology consultation for early evaluation and possible intervention, including reperfusion therapy. The non-ACS causes of elevated troponin comprise an extensive list of pathologies including pulmonary embolism, sepsis and septic shock, pericarditis, myocarditis, heart failure, and end stage renal disease (ESRD). Therapy should be individualized in such patients. In figure 1 we have presented a diagrammatic representation of management of elevated troponin in a clinical setting.
Future direction/ discussion
It is not uncommon to detect troponin in a presumably healthy person’s circulation [11]. In an otherwise healthy individual with elevated troponin, underlying risk factors such as hypertension, smoking, obesity, and structural heart diseases may be present. The presence of elevated troponin hints towards increased risk for worse prognosis in terms of heart failure, cardiovascular-related mortality, and all-cause mortality. Similarly, it is now established that individuals with elevated troponin in non-ACS diseases have poorer cardiovascular prognosis than those without elevated troponin [23, 28-32]. Hence, a cardiology consultation in the setting of an elevated troponin can provide significant collaborative expertise that can ultimately benefit patients.
When first analyzing a troponin value, it is imperative to consider the clinical situation in addition to understanding the patient’s underlying co-morbidities and baseline troponin value when available. Each time an order is placed for circulating troponin clinicians must have a high index of suspicion for ACS. In the setting of an uncertain diagnosis, further workup and consideration of other differential diagnoses is necessary. In patients who present with typical ACS and evidence of troponin elevation, prompt cardiology consultation is central to appropriate management. Correct interpretation of an elevated troponin is a critical step in recognizing disease and aids in triaging patients that may require urgent intervention. Another benefit of cardiology consultation for elevated troponin is to determine whether specific cardiac imaging may be helpful in diagnosing and treating uncommon infiltrative diseases such as amyloidosis. Any time clinicians order a laboratory test such as troponin, it should be guided by the presenting symptoms, signs, and pretest probability of coronary artery disease (CAD) and ACS.
Conclusion
Early diagnosis of a non-ACS disease in a patient's assessment of elevated troponin allows for prompt introduction of targeted management of the disease. Therefore, a clinician should be aware of non-ACS causes of elevated troponin along with the underlying pathophysiology to prevent delays in seeking expert opinion, intervention, and admission to a cardiac care unit.
Conflict of interest
The authors declare no conflict of interest.
References
- Korff S, Katus HA, Giannitsis E. Differential diagnosis of elevated troponins Heart 92 (2006): 987-93.
- Tanindi A, Cemri M. Troponin elevation in conditions other than acute coronary syndromes Vasc Health Risk Manag 7 (2011): 597-603.
- Agewall S, Giannitsis E, Jernberg T, Katus H. Troponin elevation in coronary vs. non-coronary disease Eur Heart J 32 (2011): 404-11.
- Eggers KM, Lindahl B. Application of Cardiac Troponin in Cardiovascular Diseases Other Than Acute Coronary Syndrome Clin Chem 63 (2017): 223-35.
- Higgins JP, Higgins JA. Elevation of cardiac troponin I indicates more than myocardial ischemia Clin Invest Med 26 (2003): 133-47.
- Wu AH. Increased troponin in patients with sepsis and septic shock: myocardial necrosis or reversible myocardial depression? Intensive Care Med 27 (2001): 959-61.
- Feng J, Schaus BJ, Fallavollita JA, Lee TC, Canty JM, Jr. Preload induces troponin I degradation independently of myocardial ischemia Circulation 103 (2001): 2035-7.
- Weil BR, Young RF, Shen X, Suzuki G, Qu J, Malhotra S, et al. Brief Myocardial Ischemia Produces Cardiac Troponin I Release and Focal Myocyte Apoptosis in the Absence of Pathological Infarction in Swine JACC Basic Transl Sci 2 (2017): 105-14.
- Omland T, de Lemos JA, Sabatine MS, Christophi CA, Rice MM, Jablonski KA, et al. A sensitive cardiac troponin T assay in stable coronary artery disease N Engl J Med 361 (2009): 2538-47.
- Apple FS, Ler R, Murakami MM. Determination of 19 cardiac troponin I and T assay 99th percentile values from a common presumably healthy population Clin Chem 58 (2012): 1574-81.
- Sharma S, Jackson PG, Makan J. Cardiac troponins J Clin Pathol 57 (2004): 1025-6.
- Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction J Am Coll Cardiol 36 (2000): 959-69.
- Ammann P, Fehr T, Minder EI, Gunter C, Bertel O. Elevation of troponin I in sepsis and septic shock Intensive Care Med 27 (2001): 965-9.
- Ammann P, Maggiorini M, Bertel O, Haenseler E, Joller-Jemelka HI, Oechslin E, et al. Troponin as a risk factor for mortality in critically ill patients without acute coronary syndromes J Am Coll Cardiol 41 (2003): 2004-9.
- Arlati S, Brenna S, Prencipe L, Marocchi A, Casella GP, Lanzani M, et al. Myocardial necrosis in ICU patients with acute non-cardiac disease: a prospective study Intensive Care Med 26 (2000): 31-7.
- Wright RS, Williams BA, Cramner H, Gallahue F, Willmore T, Lewis L, et al. Elevations of cardiac troponin I are associated with increased short-term mortality in noncardiac critically ill emergency department patients Am J Cardiol 90 (2002): 634-6.
- Bakshi TK, Choo MK, Edwards CC, Scott AG, Hart HH, Armstrong GP. Causes of elevated troponin I with a normal coronary angiogram Intern Med J 32 (2002): 520-5.
- Zellweger MJ, Schaer BA, Cron TA, Pfisterer ME, Osswald S. Elevated troponin levels in absence of coronary artery disease after supraventricular tachycardia Swiss Med Wkly 133 (2003): 439-41.
- Tung P, Kopelnik A, Banki N, Ong K, Ko N, Lawton MT, et al. Predictors of neurocardiogenic injury after subarachnoid hemorrhage Stroke 35 (2004): 548-51.
- Homma S, Grahame-Clarke C. Editorial comment--myocardial damage in patients with subarachnoid hemorrhage Stroke 35 (2004): 552-3.
- Cantwell RV, Aviles RJ, Bjornsson J, Wright RS, Freeman WK, Oh JK, et al. Cardiac amyloidosis presenting with elevations of cardiac troponin I and angina pectoris Clin Cardiol 25 (2002): 33-7.
- Nunes JP. Cardiac troponin I in systemic diseases. A possible role for myocardial strain Rev Port Cardiol 20 (2001): 785-8.
- Giannitsis E, Muller-Bardorff M, Kurowski V, Weidtmann B, Wiegand U, Kampmann M, et al. Independent prognostic value of cardiac troponin T in patients with confirmed pulmonary embolism Circulation 102 (2000): 211-7.
- Pruszczyk P, Bochowicz A, Torbicki A, Szulc M, Kurzyna M, Fijalkowska A, et al. Cardiac troponin T monitoring identifies high-risk group of normotensive patients with acute pulmonary embolism Chest 123 (2003): 1947-52.
- Hassan HC, Howlin K, Jefferys A, Spicer ST, Aravindan AN, Suryanarayanan G, et al. High-sensitivity troponin as a predictor of cardiac events and mortality in the stable dialysis population Clin Chem 60 (2014): 389-98.
- Murphy JT, Horton JW, Purdue GF, Hunt JL. Evaluation of troponin-I as an indicator of cardiac dysfunction after thermal injury J Trauma 45 (1998): 700-4.
- Edouard AR, Felten ML, Hebert JL, Cosson C, Martin L, Benhamou D. Incidence and significance of cardiac troponin I release in severe trauma patients Anesthesiology 101 (2004): 1262-8.
- ver Elst KM, Spapen HD, Nguyen DN, Garbar C, Huyghens LP, Gorus FK. Cardiac troponins I and T are biological markers of left ventricular dysfunction in septic shock Clin Chem 46 (2000): 650-7.
- La Vecchia L, Mezzena G, Zanolla L, Paccanaro M, Varotto L, Bonanno C, et al. Cardiac troponin I as diagnostic and prognostic marker in severe heart failure J Heart Lung Transplant 19 (2000): 644-52.
- Spies C, Haude V, Fitzner R, Schroder K, Overbeck M, Runkel N, et al. Serum cardiac troponin T as a prognostic marker in early sepsis Chest 113 (1998): 1055-63.
- Apple FS, Murakami MM, Pearce LA, Herzog CA. Predictive value of cardiac troponin I and T for subsequent death in end-stage renal disease Circulation 106 (2002): 2941-5.
- Dierkes J, Domrose U, Westphal S, Ambrosch A, Bosselmann HP, Neumann KH, et al. Cardiac troponin T predicts mortality in patients with end-stage renal disease Circulation 102 (2000): 1964-9.