Electronic Medical Community: What Rules, What Specifications?
Article Information
Mishlanov V1*, Chuchalin A2, Chereshnev V3, Poberezhets V4, Kostikas K5, Zuev A6,7
1E.A. Vagner Perm State Medical University, Perm, Russia
2N.I. Pirogov National Research Medical University, Moscow, Russia
3Institute of Physiology and Immunology, Ural Branch of Russian Academy of Science, Ekaterinburg, Russia
4National Pirogov Memorial Medical University, Vinnytsya, Ukraine
5University Hospital of Ioannina, Greece
6Institute of Continuous Media Mechanics of the Ural Branch of Russian Academy of Science, Perm, Russia
7Perm National Research Polytechnical University, Perm, Russia
*Corresponding author: Vitaliy Mishlanov, PhD MD Professor, Corr.-member of RAS, Group Secretary 01.04. m-Health/e-Health of the European Respiratory Society, Head of Propaedeutic of internal diseases Department №1 of E.A. Vagner Perm State Medical University; Pushkin str., 13, fl. 260. Perm, Russia
Received: 09 July 2021; Accepted: 19 July 2021; Published: 29 July 2021
Citation:
Mishlanov V, Chuchalin A, Chereshnev V, Poberezhets V, Kostikas K, Zuev A. Electronic Medical Community: What Rules, What Specifications?. Archives of Clinical and Biomedical Research 5 (2021): 581-597.
Share at FacebookAbstract
The aim of the review is to summarize our knowledge in digital medicine today and present a structural scheme with different perspectives for its development. The electronic medical community is forming spontaneously due to technological progress, the present epidemiological status of the community and tendency for electronic cooperation.
The clinical review includes methodology, the relevance of telemedicine development during the Covid-19 pandemic era, an overview of the instruments for remote home-based medicine, the presentation of new methods for remote preliminary diagnostics making. It also considers the role of artificial intelligence achievements in the field of remote medical monitoring, the discussion on randomized clinical trials needs in telemedicine and personal data protection as a biomedical problem.
Keywords
Electronic medical community; Artificial intelligence; Evidence-based medicine; Diagnosis; Randomized clinical trials and Covid-19
Article Details
1. Introduction
The intriguing slogan of “electronic medical community” has emerged due to many current challenges with Covid-19 being one of them [1]. Today people need to consider potential contagious danger of the face to face contact with medical personnel. Many medical devices have become accessible at home and primary diagnostic procedures are available without a medical visit. However, the secret of physician decision-making process remains complicated. Many patients need remote physician’s advice. The “electronic medical community” (EMC) includes doctor-patient, doctor-doctor, doctor-pharmacy, doctor-nurse/other healthcare professionals and doctor-industry interaction.
This means different electronic technologies using for early medical diagnosis, treatment, rehabilitation and prevention of exacerbations or adverse event as well as for primary prevention of diseases. However, there are a lot of issues to be addressed. These are: 1) what rules provide correct diagnosis; 2) what personal medical devices are approved; 3) what protocols for patient management will be better, and many other issues.
2. Methodology
We analyzed PubMed, ClinicalKey and RSCI articles using search on the key words: digital medicine, telemedicine, remote monitoring, artificial intelligence diagnostics, telerehabilitation, Covid-19 pandemic added by the “ERS literature update” prepared by V. Poberezhets (Chair of group 01.04 - m-Health/e-health ERS) et al., (2021). Then we examined the articles dated 2010-2020 and combined the similar articles. Finally, we analyzed 85 publications for the review.
3. The Problem of Medical Diagnosis Influenced by the New Coronavirus Pandemic
Due to the rapid spread of Covid-19 pandemic of infrared thermometers became commonly used [2]. But much before a lot of other well-known electronic devices had been applied for monitoring of respiratory patient status in physiotherapy such as pulse oximeter, peak flow meter and others [3]. The significant difference between the past and the present practice consists of choosing and mass using only one kind of them for the contactless thermometry as the preliminary diagnostic test for Covid-19 infection. Why is it so? It was not in accordance with evidence-based medicine but it is, in fact, a contactless technique which has become the most popular at present during the Covid-19 pandemic. Therefore, the new era of distant medical technologies based on contactless devices has started.
The majority of well-known physical methods of medical diagnosis became unusable since special medical protection wear is not very suitable for percussion or auscultation. How do we make medical diagnosis today? The traditional scheme consist of anamnesis data collecting, physical patient’s examination, construction of leading clinical syndrome and preliminary diagnosis, conducting additional laboratory tests and instrumental examinations with further differential diagnosis. Instead of these, the coronavirus pandemic and special work conditions require different procedure. The first step consists of epidemiological anamnesis data collecting, then, laboratory viral testing and HRCT making for Covid-19 exclusion/confirming. The third step is to be performed either wearing protective gear or not depending on the viral testing result. If the patient is not contagious physical examination can be performed. Alternatively, only instrumental contactless examination can be done in the case of Covid-19 confirm [4, 5]. The accuracy of only anamnesis or classical combination of a patient’s survey and physical examination was evaluated by several studies. The meta-analysis of Marchello C.S. et al. (2020) [6] is one of them. This meta-analysis confirmed that some physical data can improve the diagnostic accuracy from Likelihood Ratio (LR) of 0.24 (95% CI, 0.17 to 0.34) and a sensitivity of 0.89 (95% CI, 0.79 to 0.94) up to 0.10 (95% CI, 0.07 to 0.13) with an area under the receiver operating characteristic (ROC) curve of 0.92. These signs include decreased breath sounds, rales, crackles, changed vesicular breath sound among others. Therefore, only auscultation findings were analyzed in the studies and the difference was significant, the minimal accuracy was achieved by anamnesis alone. Is it now the case that a physician is not needed for diagnostic process yet because his/her medical professional skills are not required now?
Additionally, there are new recommendations to use chest HRCT prior to a physician’s examination of the patient evaluated in a hospital environment, based on the high accuracy of chest HRCT for Covid-19 screening [7]. NICE recommendations are targeting those patients who can stay at home isolation under video monitoring. In such patients the wide use of HRCT is not applicable and, therefore, we have to discuss other diagnostic tools which are available at home.
4. Medical Devices for Home Using
First tools are for video monitoring. Video camera surveillance is the simplest way to contact a patient on a daily basis, ask him about his condition, analyze his status and monitor his reactions to a physician’s recommendations [8, 9]. This method has advantages and some disadvantages. It is cost effective; it improves medical care and may prevent patient deterioration. The disadvantage in this case might be the difficulties to protect privacy and data security of patients. For example, the result of video monitoring is not absolute and requires the additional options. This approach has been used in recent years to TB patients in a form of video (virtually) observation therapy (VOT) to control the use of medication. VOT uses Smartphone or other mobile devices for video treatment support [10].
Some more detailed Information can be obtained by different interactive questionnaires. It can be used for monitoring as well as both preliminary diagnosis and monitoring. Normally, patient surveys are used in the complex tools and they are very successful in COPD or Covid-19 home patient monitoring [11-13].
There is a lot of different simple medical equipment for home using. For example, clever shirt for lung volume measurement [14], electronic inhalers [15, 16], electronic peak flow meter [17, 18], portable electronic spirometers [19, 20], sleep respiratory rate monitor [21], cough assessment mobile platforms [21-26], exhaled NO monitoring for the follow up and evaluation of adherence of patients with asthma [27], laboratory express tests [28] and others. As usual, they are recommended for patient monitoring at home but not for diagnostic purposes.
Thereby, the usage of home medical devices and their active development for remote patient preliminary diagnostics and monitoring is key feature of modern healthcare. Remote electronic monitoring significantly improves the healthcare system. Nevertheless, the preliminary diagnosis for remote patients remains a serious medical problem.
5. New Methods for Preliminary Remote Medical Diagnosis and their Accuracy
Medical diagnosis is very difficult to comprehend and it is based on several principles. The required diagnostic skills include collecting patients’ complaints, anamnesis evaluation, physical examination, using high specify laboratory and instrumental methods. The high accuracy of diagnostic result is dependent on the quality of all mentioned above methods. Let us analyze which method is of a greater significance on the list of patient examination methods?
We suggest that there is a number of different confirming data of the diagnosis. These data do not dependent on the method that they can be achieved. The hypothesis consists of that any definite number of certain clinical signs will have the comparative specificity to the diagnosis in the case if every test is specified. It is required to define the number of specific clinical features for different disease entities or syndromes. For example, let’s suggest for the first step that seven specific signs are enough to diagnose bronchial obstructive syndrome. May be only 2-3 symptoms are enough for bronchitis and 5-6 signs are required for lung parenchyma damage syndrome.
The second step is to choose the diagnostic methods. The simplest one is patient questioning which is used for remote consultations in some countries and for patient monitoring including the new coronavirus cases [29]. It will be different from the traditional diagnostic mode, because we will not use the combination of patient survey and physical methods. It is requiring a comparative study of two methods of diagnosis making; they are new and traditional modes. There are some other variants of diagnostic mode using different instruments, devices or laboratory tests. For example, some scientists suggest home self-auscultation with computer analysis of chest sounds [30, 31] or self-performed home spirometry [21, 32], smart watch using [33] and other medical diagnostic devices.
The accuracy of a single test is rather low but the combination of several diagnostic methods can provide data needed to perform accurate diagnostic results. The key factor ? is to choose the most specific tests, signs and symptoms. Therefore, we may hypothesize that the combination of simple monitoring methods can bring the required accuracy in the case of the number of specific clinical signs is satisfactory.
What kinds of simple medical home tests do we have today? They are: Smart watch (HR, BP, sleep time, physical activity), smart shirt (lung volume, RR), portable spirometer (airflow velocity and respiratory volumes), auscultation system for home using (rales, crackles, wheezing), cough monitor (cough registration and analysis), weight meter (BMI calculation), dynamometry and some others including express laboratory ones [34-38]. Many parameters can be monitored and a number of medical tasks can be solved by using them.
For example: activity monitoring, heart rate monitoring, speech therapy adherence, diabetes self-management, and detection of seizures, tremors, scratching, eating, and medication-taking behaviors. Are these tests specific for any particular diagnoses?
Yes, some of the listed above tests are specific for respiratory diseases or syndromes. One very well-known criterion of COPD severity is the BODE index [39]. It consists of the values of body mass index, dyspnea, distance of 6-MWT and FEV1. Therefore, the combination of patient regular survey, weight and FEV1 measurement plus aerobic exercise capacity and endurance evaluation can be useful for COPD patient status estimation. Recently our own data have confirmed that the number of night symptoms correlates with the number of year COPD exacerbations [40]. It suggests using the smart watch to analyze the sleep structure of COPD patients as an effective test for a rehabilitation program.
However, the single test is useful only for the monitoring and it is not sufficient for preliminary diagnosis. How many score points are necessary for the preliminary patient examination? Our own study shows that it is not less than 30-50 parameters [41]. It does not mean that the general number of questions may be 30-50 because the same clinical sign can be felt differently. The total number of questions to detect one medical problem should be up to 200 in order to achieve the accurate result.
The number of questions will be lesser when other clinical signs are revealed by any techniques. The best sequencing of modern medical diagnostics consists of two steps. The first one is patient survey approach. The second step includes additional instrumental or laboratory tests for specific clinical signs and confirmation of the primary hypothesis. The accuracy of this approach is from 89 to 92% and above.
6. Medical Monitoring
This medical task can be solved easier than preliminary diagnostics in different ways. The mobile electronic monitoring systems are more perspective and attract great attention [42]. What goals can they achieve? First of all, they induce physical activity of a patient and patient participation in healthcare programs [43]. Another goal is an attempt to prevent exacerbations of chronic disease [44, 45]. The simplest decision of these tasks is mobile app using with the possibility to analyze walk distance, energy expenditure, heart rate, and heart rate variability. Through the monitoring mobile software a patient receives more information about his/her health status. The App is feasible for most of the patients but it does not confirm the direct influence on the exacerbation frequency. The meta-analysis of 13 trials did not reveal significant differences between traditional management and mobile APP using, but the great heterogeneity between the trials did not allow the authors to reach certain conclusion [46].
Heterogeneity of different digital solutions is possibly the main cause of uncertain results in home COPD patient monitoring. This difference consists of monitor tools, in a case of decision making system, physical activity management devices and others. So, the decision of possible COPD patient self-management is not adopted today and it needs an additional study [47]. It is absolutely clear, that we need classification of different digital solutions to make appropriate meta-analysis and evidence based results. One of possible solution was presented in our paper previously [48]. The classification of digital medicine has to include tele-monitoring, tele-rehabilitation, tele-consultation, tele-diagnosis and other separate parts. So, any study can be aimed only at one of these parts. However, at present there are many papers which combine tele-monitoring and tele-rehabilitation or sometimes additional kinds of telemedicine. For example, it is difficult to understand the cause of positive results in the study of H.L. Persson et al. because we do not have information about basic treatment program as for COPD as for CHF patients [49]. It is possible that the authors are not able to combine two different groups of patients with unknown severity and basic therapy. Additionally, this study is not comparative research. Further study has to demonstrate only standard sources of patient status assessment, recommended classification of COPD or other nosological form classification.
7. Bioethics as the Instrument of Technological Society Progress. The Role of Randomized Clinical Trials
Bioethics is the science of industrial society development. It makes new reality feasible for people through the specific rules, standards well-defined principles of the new technologies implementation and their consequences [41, 50]. One of the most significant bioethics postulates is the principle of evidence-based medicine. It needs to help people make well-informed decisions about health care by preparing, maintaining and promoting the accessibility of systematic reviews of the effects of healthcare interventions [51]. Now we see the rapid development of the telemedical science. The speed of its development depends on the accuracy of clinical research principles applied [52-56].
In accordance to the evidence-based medicine it is recommended to choose only one task in a problem to be resolved as we cannot choose an appropriate study design and randomize the patients if they present different clinical conditions [54]. So, the recommendation for future clinical research will include not only classification of the telemedicine purpose (tele-monitoring, tele-rehabilitation, tele-consultation, tele-diagnosis and others [41]) but also standardization demand for certain clinical status of including patient group, characteristics of treatment program, social group including education and computer skills, and many other parameters.
8. Electronic Medical Community
The “electronic medical community” (EMC) is in the process of spontaneous formation due to technological progress, actual epidemiological status of society and tendency of people to communicate and cooperate electronically [57]. This presents several goals: as early medical diagnosis, patient treatment, rehabilitation and disease prevention. Every task can be subdivided into 3 levels: rules, devices and medical protocols (methods).
8.1 Medical diagnosis
8.1.1 Rules and principles: There are two possibilities to realize it. The first – with personal data security protection and the second – sharing personal information to use community or artificial intelligence. The 1st can be based only on an algorithmic method of intellectual system. The 2nd may use both algorithm and artificial intelligence. Today the accuracy of intelligence diagnostics algorithms is near 90-92% [41], the artificial intelligence presents very high accuracy in restricted tasks solving only such as CT visual pictures analysis and other images techniques up to 90% and more [58]. Among them there are two main devices in artificial intelligence – machine learning and deep neural networks (DNNs), where structured data (i.e. images, electrophysiological and genetic data, etc.) are analyzed and natural language processing, where unstructured data are analyzed [59-63]. As a rule, artificial intelligence and machine learning are particularly helpful in the areas where the diagnostic information provided by the doctor’s examination is already in the digital form, such as:
- Thoracic imaging (detecting lung cancer, malignant pulmonary nodules, congestive cardiac failure, tuberculosis, pneumonia, pneumothorax, pulmonary embolism, interstitial lung disease, and even accurately diagnose airways disease such as bronchiectasis, asthma or COPD)
- Histopathology and cytology (lung cancer and TB diagnosis).
- Physiological measurements and biosignals (spirometry, body plethysmography, forced oscillation, SpO2, breath analysis, lung sounds, cough sounds, polysomnography).
8.1.2 Devices and software: As it was speculated above there are two basic approaches, devices and software which realize intelligence decision making system or artificial intelligence for medical diagnostics. For example, “Electronic polyclinic” (Russia) [41] presents possible algorithmic diagnostic process. Some scientists state the advantages of algorithm since it provides us with easily interpreted results [64]. We also have to understand that artificial intelligence use is possible and it is needed to analyze big data. So, in the case of individual diagnosis the system is necessary in previous learning or collecting the same parameters in the standard patient group. In the last two decades a lot of publications have demonstrated different applications of deep machine learning approach [62, 65]. The technique of natural language processing or deep learning consists of multilevel network using and it is designed to identify appropriate words, questions or answers in a text or a patient’s verbal report. Based on previous experience the system of natural language processing uses some special indices of clinical data interactions. Therefore, the natural language processing system needs sufficient database which is stored in the cloud or a computer server network. Data processing of makes personal data unprotected. That represents another bioethical problem.
The next unfavorable feature of artificial intelligence usage is necessity of lowering of high-dimentional data to use machine learning [62]. This principle is referred to as “convolution neural network” and it uses different variants of data classification to combine them. In this case the problem of data missing is present. The same principle is used in classical medical diagnosis more than the last century and it is referred as to “a syndrome diagnostics” or hypothesis-deductive method. A syndrome is a combination of clinical symptoms of the same pathogenesis [41]. This principle is very effective and is used in “Electronic polyclinic” algorithm construction. The convolution neural network is applied in such products as Caffe from Berkeley AI Research [66], CNTK from Microsoft [67], TensorFlow from Google [68] and some others. But if we can find the appropriate words and patients using personal medical record, we will not be able to find appropriate patient among other people, because we do not use special terms in every day practice.
8.1.3 Medical protocol: Today we do not have enough clinical evidence and recommendations to realize remote medical diagnosis. But clinical data obtained through using different modules of the computer program “Electronic polyclinic” included more than 3000 healthy people and patients with respiratory, cardiovascular, gastroenterological and oncological diseases [41]. Artificial intelligence is effectively used in medical records analysis only [69].
Patient treatment and rehabilitation base on medical monitoring, electronic education and physical training of a patient indoor department or at home.
8.2 Rules and principles
The task of automatically choosing treatment or rehabilitation program is simpler than the diagnostic one. The number of data needed is less. So, this task can be effectively performed either by algorithmic or different variants of artificial intelligence software [70]. Structured data is preferable for this purpose. Now we have a lot of diagnostic scales for a treatment program to choose from clinical recommendations and guidelines: GOLD, GINA, ACS, etc. [71-73]. Nowadays, the results of randomized clinical trials are the instruments to find the best clinical indicator for any clinical tasks and all clinical scales are constructed of these indexes. The era of artificial intelligence presents us the new mechanisms that are based on data interactions investigation [74]. The artificial intelligence not only finds the right indices at ones but makes this process regularly during every test processing. Sometimes artificial intelligence makes an opposite decision at first and presents an understandable result. It is possible if some new conditions influence the system but demand a needed number of clinical observations (the power of study). The database of artificial intelligence can be changed. In every case of new result taken we can ask ourselves: is the database (the power of study) enough to make a serious decision or not, is control group comparable to the experience one or not? We will consider only that system which includes needed criteria in according to the principles of evidence based medicine. But we have not found such information evaluating the scientific publications on clinical results of artificial intelligence implementation. So, the next problem of artificial intelligence clinical using is a variety and the difficulty of explaining results. This problem can be solved by restricting the number of new observations for decision changing. In this case the artificial intelligence will become an algorithmic program.
8.2.1 Devices and software: The advantage of artificial intelligence consists of different combination of personal electronic devices for clinical remote monitoring. The number of medical techniques includes validated questionnaires, heart rate, respiratory rate, blood pressure, electrocardiogram, and body composition and sleep monitors [75]. They can work on-line or off line with data accumulation and analysis on personal computer with special medical algorithm. Physical training program such as video with adaptation to the patient’s health status can be presented by computer monitoring [76, 77] or may be implemented by a humanoid robot [78]. Machine learning could also be used in smoking secession programs for screening associated with adherence to nicotine-replacement therapy and cessation programs, which will help to develop targeted intervention strategies to promote adherence [79].
Medical protocol of different home or wearable monitors using can be in accordance to nosological form and disease severity or phenotype. For example, ECG and blood pressure monitors were implemented in clinical practice by the procedure of standardization [80, 81]. It is well understandable that a patient with arterial hypertension needs blood pressure monitoring. The modern rehabilitation demands different monitors using at the same time. For example, the patient with chronic obstructive pulmonary disease needs physical activity measurement, psychical status evaluation, thigh strength control, body mass index determine and other parameters monitoring [82].
Disease prevention, primary and secondary prophylaxis includes early risk factor diagnosis, genetics, physical training and vaccination. Interactive questioning is one of the best decisions but it may be used predominantly as health care system oblique recommendation. It is more interesting to use an artificial intelligence to analyze patient habits, HR, RR, BP, and sleep monitoring using different individual devices [83, 84].
The electronic diary may remind a patient about useful vaccination with a certain educational program. The best decision of medical education is to implement it to the patient diary but in a schematic connection with diagnostic algorithm in order to make it personalized.
All mentioned above tasks of Electronic medical community stimulate new clinical trials, scientific discussions using electronic communication tools, group formation and cooperation of medics with digital specialists, societies and engineering companies. We suggest that “electronic medical community” (EMC) could be the basis for Global Initiative for Telemedicine Advance (GITA).
9. Perspectives of Clinical Trials
Today the electronic medical community is spontaneously developing human interaction. But the nearest future seems to be more structured, using special rules, and in accordance to some specifications. The task of recommendation construction is one of the main aims of international medical societies such as the European respiratory society. The development is dependent on technical progress and coordination between the new devices construction and principles of medical care is very important as well. We have to spread the evidence based medicine into telemedicine. Every intellectual or telemonitoring system needs randomized clinical trial (RCT) in comparison with existing techniques. They will be special RCT for any autonomous device or the new medical technology using new equipment for medical treatment or rehabilitation at home.
However, one can think that low-cost Big Data analyses could replace traditional RCT taking into account that machine learning is able to create virtual controls to reach the same outcomes as RCT. According to Pépin, Jean?Louis, Sébastien Bailly, and Renaud Tamisier Obstructive sleep apnea could be a good candidate for assessing because of large amount of data from the patients that can be easily collected via telemonitoring and currently existing large registries [85]. But replacement RCT by artificial intelligence system isn’t possible because it isn’t comparative and makes bioethics problem of personal data sharing protection. Everyone who wants to use the artificial intelligence system has to agree to data sharing. The artificial intelligence system is only the method of medical goal achievement. So, the 1st rule is RCT for every device and medical technology. The artificial intelligence needs larger population to be examined. Hence, their implementation will be more expensive and it will take more time to be proved.
The 2nd rule is the priority of personal data protection. We have two ways to achieve that. The first one is special software saving. But this way is not absolutely safe. The second way is to add algorithmic intellectual technology. This way does not need sharing the personal data which can be analyzed in a closed system or even by a single computer equipped with special software. A potential option could be the personal patient’s computer at home. The artificial intelligence development has priority in closed corporations, for example, in insurance companies, in large factories and so on, which prevents unauthorized using of personal patient data.
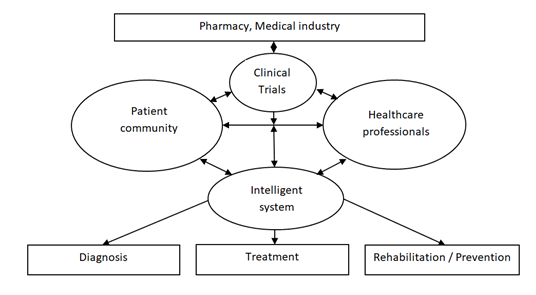
The 3rd rule consists of developing the communication via using medical personal data. It can be shared or closed using special protect systems. Both options have to use only adopted criteria, indexes and specific clinical signs in according to clinical guidelines and recommendation of medical community. The recommendation for future clinical trials consists of medicine effectiveness study in the intellectual system based on the special treatment algorithm. The presence of this electronic intellectual algorithm (software) let us guarantee an appropriate recommendation in using a particular drug to special diagnostic criteria. So, the intellectual program must be diagnostic and treatment or diagnostic and rehabilitation. The best results can be achieved by using combination of patient’ survey and devises implementation for regular patient monitoring. As science is a great force of society development, how can it stimulate the electronic medical community arising? The task consists of performance of the rules, stated above and communication stimulation. As an option, the following scheme can be presented based on a science review (Figure 1).
10. Conclusion
The electronic medical community is currently on demand and it is developing spontaneously by stimulating of technical progress. The present medicine needs guideline for this process.
The main directions are as follows: randomized clinical trials for every electronic device, software and clinical status; the priority of personal data protection which will be best by algorithmic technology using; and future clinical trials must include electronic model construction and studying how to use the primary clinical results.
The basis on electronic medical community will be randomized clinical trials of new electronic medical equipment including software and diagnostic systems. One of the important statements is that any new devices, computer scales, monitoring systems have to be incorporated in one analytical system which lets to classify and identify a patient in a large population accounting for all included and excluded data of the clinical case.
This review highlights the property of an interactive questionnaire “Electronic polyclinic” that demonstrates the most comprehensive specifications for patient status evaluation.
Acknowledgement (Funding)
The reported study was funded by RFBR and Perm Territory, project number 20-415-596008.
Authors gratefully acknowledge Ph.D. Svetlana Polyakova, associate Professor of the Department of English Language and Intercultural Communication and Department of Linguodidactics of the Faculty of Modern Foreign Languages and Literatures of the Perm State National Research University and Elena Yakovleva, Professor assistant of the Department of Linguodidactics of the Faculty of Modern Foreign Languages and Literatures of the Perm State National Research University, for the English revision of the manuscript.
Authors’ Contributions
Vitaliy Mishlanov, general idea, 45% of text; other part was formed by authors in equal rates.
Conflict of Interests
No potential conflict of interest was reported by the authors.
References
- Keshvardoost S, Bahaadinbeigy K, Fatehi F. Role of Telehealth in the Management of COVID-19: Lessons Learned from Previous SARS, MERS, and Ebola Outbreaks [published online ahead of print, 2020 Apr 23]. Telemed J E Health 10 (2020).
- Infrared Thermometer. DT8018D // Shenzhen Shunhe Electric Technology CO., LTD web site (2020).
- Aliverti A. Wearable technology: role in respiratory health and disease. Breathe (Sheffield, England) 13 (2017): e27-e36.
- Pluddemann A, Hobbs R, Mahtani KR, Heneghan C. Rapid diagnosis strategy of community-acquired pneumonia for clinicians (2020).
- NICE Covid-19 rapid guideline on managing symptoms (including at the end of life) in the community. The BMJ Visual summary. Covid-19: remote consultations. // National Institute for Health and Care Excellence (Nice) web site (2020).
- Marchello CS, Ebell MH, Dale AP, Harvill ET, Whalen CC. Signs and Symptoms That Rule out Community-Acquired Pneumonia in Outpatient Adults: A Systematic Review and Meta-Analysis. J Am Board Fam Med 32 (2019): 234-247.
- Li Y, Xia L. Coronavirus Disease 2019 (COVID-19): Role of Chest CT in Diagnosis and Management. AJR 214 (2020): 1-7.
- Cournan M, Fusco-Gessick B, Wright L. Improving patient safety through video monitoring. Rehabilitation Nursing 43 (2018): 111-115.
- Braeken A, Porambage P, Gurtov A, Ylianttila M. Secure and Efficient Reactive Video Surveillance for Patient Monitoring. Sensors (Basel) 16 (2016): 32.
- Falzon D, Timimi H, Kurosinski P, Migliori GB, Van Gemert W, et al. Digital health for the End TB Strategy: developing priority products and making them work. The European respiratory journal 48 (2016): 29-45.
- Webster P. Virtual health care in the era of COVID-19. Lancet 395 (2020): 1180?1181.
- Pan XB. Application of personal-oriented digital technology in preventing transmission of COVID-19. Ir J Med Sci (2020): 1?2.
- Jiang Y, Liu F, Guo J, Sun P, Chen Z, et al. Evaluating an Intervention Program Using WeChat for Patients With Chronic Obstructive Pulmonary Disease: Randomized Controlled Trial. Journal of medical Internet research 22 (2020): e17089.
- Mannée D, De Jongh F, Van Helvoort H. Tidal volumes during tasks of daily living measured with a smart shirt. European Respiratory Journal 54 (2019): PA2228.
- Chan AHY, Harrison J, Black PN, Mitchell EA, Foster JM. Using Electronic Monitoring Devices to Measure Inhaler Adherence: A Practical Guide for Clinicians. J Allergy Clin Immunol Pract 3 (2015): 349.e2.
- Cazzola M, Cavalli F, Usmani OS, Rogliani P. Advances in pulmonary drug delivery devices for the treatment of chronic obstructive pulmonary disease. Expert Opin Drug Deliv 17 (2020): 635?646.
- BMedical products. https://bmedical.com.au/product-category/treatment-products/smart-peak-flow (2020).
- Ferrer Pharma Company Pty Ltd. https://ferrerpharma.com.au/ smart-peak-flow-meter (2020).
- Bluetooth spirometers. The Online Medical Device Exhibition (2020).
- Zhou P, Yang L, Huang YX. A Smart Phone Based HandheldWireless Spirometer with Functions and Precision Comparable to Laboratory Spirometers. Sensors 19 (2019): 2487.
- Dietz-Terjung S, Geldmacher J, Brato S, Linker CM, Welsner M, et al. A novel minimal-contact biomotion method for long-term respiratory rate monitoring [published online ahead of print, 2020 Apr 15]. Sleep Breath (2020).
- Sterling M, Rhee H, Bocko M. Automated Cough Assessment on a Mobile Platform. J Med Eng (2014): 951621.
- Cho PSP, Birring SS, Fletcher HV, Turner RD. Methods of Cough Assessment. The Journal of Allergy and Clinical Immunology: In Practice 7 (2019): 1715-1723.
- Menzies-Gow A, Mansur AH, Brightling CE. Clinical utility of fractional exhaled nitric oxide (FeNO) in severe asthma management. Eur Respir J (2020).
- Chung KF. Measurement of cough. Respir Physiol Neurobiol 152 (2006): 329?339.
- Mills CS. Measuring Voluntary and Reflexive Cough Strength in Healthy Individuals. The University of Canterbury (2016): 77
- Menzies-Gow A, Mansur AH, Brightling CE. Clinical utility of fractional exhaled nitric oxide (FeNO) in severe asthma management European Respiratory Journal 55 (2020): 1901633.
- Dark Daily. Serving Clinical Labs and Pathology groups (2020).
- Ohannessian R, Duong TA, Odone A. Global Telemedicine Implementation and Integration within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Health Surveill 6 (2020): e18810.
- Grønnesby M. Automated Lung Sound Analysis. Master Thesisin Computer Science, INF-3981, Spring (2016): 75
- Pramono RXA, Bowyer S, Rodriguez-Villegas E. Automatic adventitious respiratory sound analysis: A systematic review. PLoS One 12 (2017): e0177926.
- Zhou P, Yang L, Huang YX. A Smart Phone Based HandheldWireless Spirometer with Functions and Precision Comparable to Laboratory Spirometers. Sensors 19 (2019): 2487.
- Reeder B, David A. Health at hand: A systematic review of smart watch uses for health and wellness. J Biomed Inform 63 (2016): 269-276.
- Suh MK, Chen CA, Woodbridge J, Tu MK, Kim JI, et al. A remote patient monitoring system for congestive heart failure. Journal of medical systems 35 (2011): 1165-1179.
- Mohammadzadeh N, Safdari R. Patient monitoring in mobile health: opportunities and challenges. Med Arch 68 (2014): 57-60.
- Sundaram P. Patient monitoring system using android technology. IJCSMC 2 (2013): 191-201.
- Birring SS, Fleming T, Matos S, Raj AA, Evans DH, et al. The Leicester Cough Monitor: preliminary validation of an automated cough detection system in chronic cough. European Respiratory Journal 31 (2008): 1013-1018.
- Shelagh D. The technology, devices, and benefits of remote patient monitoring in the healthcare industry (2019).
- Ansari K, Keaney N, Kay A, Price M, Munby J, et al. Body mass index, airflow obstruction and dyspnea and body mass index, airflow obstruction, dyspnea scores, age and pack years-predictive properties of new multidimensional prognostic indices of chronic obstructive pulmonary disease in primary care // Ann Thorac Med 11 (2016): 261-268.
- Bekker KN. The specifies of clinical picture and treatment results of patients with comorbidities of chronic bronchial obstructive and cardiovascular diseases. Issue of candidate thesis. [Published in russian]. Perm (2019): 20.
- Chuchalin AG, Chereshnev VA, Mishlanov VJu, Mishlanov YaV, Nikitin AE, et al. Bioethics, artificial intelligence and medical diagnosis / Trans. by V. Alekseev. Perm: E.A. Vagner, PSMU (2019): 184.
- Sharman A, Zhussupov B, Sharman D, Kim I. Evaluating Mobile Apps and Biosensing Devices to Monitor Physical Activity and Respiratory Function in Smokers With and Without Respiratory Symptoms or Chronic Obstructive Pulmonary Disease: Protocol for a Proof-of-Concept, Open-Label, Feasibility Study. JMIR Res Protoc 9 (2020): e16461.
- Nyenhuis SM, Balbim GM, Ma J, Marquez DX, Wilbur J, et al. A Walking Intervention Supplemented With Mobile Health Technology in Low-Active Urban African American Women With Asthma: Proof-of-Concept Study. JMIR formative research 4 (2020): e13900.
- Rodriguez Hermosa JL, Fuster Gomila A, Puente Maestu L, Amado Diago CA, Callejas González FJ, et al. Compliance and Utility of a Smartphone App for the Detection of Exacerbations in Patients With Chronic Obstructive Pulmonary Disease: Cohort Study. JMIR mHealth and uHealth 8 (2020): e15699.
- Vasilopoulou M, Papaioannou AI, Kaltsakas G, Louvaris Z, Chynkiamis N, et al. Home-based maintenance tele-rehabilitation reduces the risk for acute exacerbations of COPD, hospitalisations and emergency department visits. Eur Respir J 49 (2017): 1602129.
- Shaw G, Whelan ME, Armitage LC, Roberts N, Farmer AJ. Are COPD self-management mobile applications effective? A systematic review and meta-analysis. NPJ Prim Care Respir Med 30 (2020): 11.
- Gaveikaite V, Grundstrom C, Lourida K, Winter S, Priori R, et al. Developing a strategic understanding of telehealth service adoption for COPD care management: A causal loop analysis of healthcare professionals. PloS One 15 (2020): e0229619.
- Mishlanov V, Chuchalin A, Chereshnev V, Poberezhets V, Vitacca M, et al. Scope and new horizons for implementation of m-Health/e-Health services in pulmonology in 2019. Monaldi Archives for Chest Disease 89 (2019): 1112.
- Persson HL, Lyth J, Lind L. The Health Diary Telemonitoring and Hospital-Based Home Care Improve Quality of Life Among Elderly Multimorbid COPD and Chronic Heart Failure Subjects. Int J Chron Obstruct Pulmon Dis 15 (2020): 527?541.
- Berwick D, Hiatt H, Janeway P, Smith R. An ethical code for everybody in health care. BMJ 315 (1997): 1633-1634.
- Volmink J, Siegfried N, Robertson K, Gülmezoglu AM. Research synthesis and dissemination as a bridge to knowledge management: the Cochrane Collaboration. Bulletin of the World Health Organization 82 (2004): 778-783.
- Cochrane AL 1931-1971: A critical review, with particular reference to the medical profession. In: Teeling-Smith G, Wells N, editors. Medicines for the year 2000. London: Office of Health Economics (1979): 1-11.
- Gallin GI, Ognibene FP, Johnson LL. Principles and Practice of Clinical Research, Fourth Edition. Academic Press (2017): 824.
- Sackett DL, Wennberg JE. Choosing the best research design for each question. BMJ (Clinical research ed.) 315 (1997): 1636.
- Sibbald B, Roland M. Understanding controlled trials: Why are randomized controlled trials important? BMJ 316 (1998): 201.
- Sibbald B, Roland M. Why are randomized controlled trials important? BMJ 316 (1998): 201.
- Dundon A, Cipolla D, Mitchell J, Lyapustina S. Reflections on Digital Health Tools for Respiratory Applications [published online ahead of print, 2020 Mar 16]. J Aerosol Med Pulm Drug Deliv (2020).
- Li Y, Xia L. Coronavirus Disease 2019 (COVID-19): Role of Chest CT in Diagnosis and Management. AJR 214 (2020): 1-7.
- Artificial Intelligence in Medicine (2020).
- Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J 6 (2019): 94-98.
- Kamdar JH, Jeba Praba J, Georrge JJ. Artificial Intelligence in Medical Diagnosis: Methods, Algorithms and Applications. In: Jain V., Chatterjee J. (eds) Machine Learning with Health Care Perspective. Learning and Analytics in Intelligent Systems. Springer, Cham 13 (2020).
- Jiang F, Jiang Y, Zhi H, Dong Y, Li H, et al. Artificial intelligence in healthcare: past, present and future. Stroke and Vascular Neurology 2 (2017).
- Gonem S, Janssens W, Das N, Topalovic M. Applications of artificial intelligence and machine learning in respiratory medicine. Thorax 75 (2020): 695-701.
- Sikchi SS, Sikchi S, Ali MS. Artificial intelligence in medical diagnosis. International Journal of Applied Engineering Research 7 (2012): 1539-1543.
- Gomez-Gonzalez E, Gomez E, Marquez-Rivas J, Guerrero-Claro M, Fernández-Lizaranzu I, et al. Artificial Intelligence in Medicine and Healthcare: a review and classification of current and near-future applications and their ethical and social impact (2020).
- Singh, Sanjay and Jindal, Stuti. Designing Deep Learning Neural Networks using Caffe (2015).
- Machine Learning in Python: Main Developments and Technology Trends in Data Science, Machine Learning, and Artificial Intelligence. Information 11 (2020): 44.
- Abadi M, Agarwal A, Barham P, et al. TensorFlow: large-scale Machine Learning on heterogeneous distributed Systems (2016).
- Castro VM, Dligach D, Finan S, Yu S, Can A, et al. Large-scale identification of patients with cerebral aneurysms using natural language processing. Neurology 88 (2017): 164-168.
- Bashi N, Fatehi F, Mosadeghi-Nik M, Askari MS, Karunanithi M. Digital health interventions for chronic diseases: a scoping review of evaluation frameworks. BMJ Health Care Inform 27 (2020): e100066.
- Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease (2020).
- Global Initiative for Asthma Management and Prevention. Updated 2020 (GINA, 2020 Report) (2020).
- ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC) (2015).
- Vecoven N, Ernst D, Wehenkel A, Drion G. Introducing neuromodulation in deep neural networks to learn adaptive behaviours. Introducing neuromodulation in deep neural networks to learn adaptive behaviours. PLOS ONE 15 (2020): e0227922.
- Dias D, Paulo Silva Cunha J. Wearable Health Devices-Vital Sign Monitoring, Systems and Technologies. Sensors (Basel) 18 (2018): 2414.
- Vitacca M, Fumagalli LP, Borghi G, Colombo F, Castelli A, et al. Home-based telemanagement in advanced COPD: Who uses it most? Real-life study in Lombardy. COPD 13 (2016): 491-498.
- Fitzsimmons DA, Thompson J, Bentley CL, Mountain GA. Comparison of patient perceptions of Telehealth-supported and specialist nursing interventions for early stage COPD: a qualitative study. BMC Health Serv Res 16 (2016): 420.
- Robot-diagnost. Promobot LLC (2020).
- Nayoung K, McCarthy DE, Loh WY, Cook JW, Baker TB. Predictors of adherence to nicotine replacement therapy: Machine learning evidence that perceived need predicts medication use. Drug and alcohol dependence 205 (2019): 107668.
- Ataman SL, Cooper R, Rotimi C, McGee D, Osotimehin B, et al. Standardization of blood pressure measurement in an international comparative study. J Clin Epidemiol 49 (1996): 869-77.
- Tolonen H, Koponen P, Naska A, Männistö S, Broda G, et al. EHES Pilot Project. Challenges in standardization of blood pressure measurement at the population level. BMC Med Res Methodol 15 (2015): 33.
- Benzo R. Activity monitoring in chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev 29 (2009): 341-347.
- Celli BR. Part 5. Management Guiderlines for Cronic obstructive pulmonary disease. In: Hanania NA, Sharafkhaneh A. COPD: a guide to diagnosis and clinical management. Respiratory medicine. Springer Science+Buisiness Media, LLC (2011): 82-83.
- Vitacca M, Holland A. Telethelth in pulmonary rehabilitation. In: Clini E. Textbook of pulmonary rehabilitation. Springer International Publishing AG 23 (2018): 307-315.
- Pépin JL, Sébastien B, Renaud Tamisier. Big Data in sleep apnoea: Opportunities and challenges. Respirology 25 (2020): 486-