Effectiveness of Core Stabilization Exercise along with Conventional Physiotherapy on Pain, Proprioception and Disability in Patients with Chronic Low Back Pain: A Randomized Control Trial Protocol
Article Information
Md Waliul Islam1, Md Tanzir-Uz-Zaman1, Md Golam Kibria2, Md Mostafijur Rahman3, Md Jubair Hassan4, Saddam Hossain5, Md Kutub Uddin6, Mohammad Ainur Nishad Rhajib1, Md Zakir Hossain3, Abdullah Ibn Abul Fazal3 and Mohammad Anwar Hossain7*
1Senior Clinical Physiotherapist, Centre for the Rehabilitation of the Paralised, Bangladesh
2Junior Consultant of Physiotherapy, Centre for the Rehabilitation of the Paralised, Bangladesh
3Clinical Physiotherapist, Centre for the Rehabilitation of the Paralised, Bangladesh
4Physiotherapist and Rehabilitation officer, Handicap International (Humanity and Inclusion)
5Consultant Asia Digital Physiotherapy and Orthopedic Rehabilitation Centre, Bangladesh
6Lecturer, SAIC College of Medical Science & Technology, Dhaka, Bangladesh
7Associate professor, Bangladesh Health Professions Institute (BHPI), Dhaka, Bangladesh
*Corresponding Author: Mohammad Anwar Hossain, Associate Professor, Bangladesh Health Professions Institute (BHPI), Dhaka, Bangladesh.
Received: 20 July 2022; Accepted: 26 July 2022; Published: 28 July 2022
Citation: Md Waliul Islam, Md Tanzir-Uz-Zaman, Md Golam Kibria, Md Mostafijur Rahman, Md Jubair Hassan, Saddam Hossain, Md Kutub Uddin, Mohammad Ainur Nishad Rhajib and Abdullah Ibn Abul Fazal. Effectiveness of Core Stabilization Exercise along with Conventional Physiotherapy on Pain and Disability in Patients with Chronic Low Back Pain; A Randomized Control Trial Protocol. Journal of Orthopedics and Sports Medicine 4 (2022): 205-210.
Share at FacebookAbstract
Background/Purpose: Currently, there is significant emphasis on importance of core muscle in rehabilitation of musculoskeletal pain like low back pain. Therefore, this study aim to investigate where additional core muscle training improve clinical outcomes.
Methods: In a randomized controlled trial 60 patient will be randomly allocated to two groups of conventional physiotherapy and core stability exercise with conventional therapy. Single blind randomize control trial design will be used in this study. Total treatment session will be 4 sessions per week for 12 weeks.
Outcome Measurement: The investigator will assess the pain before and after intervention with Numeric Pain Ratting Scale (NPRS) and disability with Oswestry Low Back Pain Disability Index. Intermediate assessment will be performed after 6 weeks of intervention.
Discussion: This study will provide evidence for additional effect of core stability exercise on pain and functional disability for patient with low back pain.
Keywords
Chronic Low back pain; Core stabilization exercise; Conventional physiotherapy
Physiotherapist articles Physiotherapist Research articles Physiotherapist review articles Physiotherapist PubMed articles Physiotherapist PubMed Central articles Physiotherapist 2023 articles Physiotherapist 2024 articles Physiotherapist Scopus articles Physiotherapist impact factor journals Physiotherapist Scopus journals Physiotherapist PubMed journals Physiotherapist medical journals Physiotherapist free journals Physiotherapist best journals Physiotherapist top journals Physiotherapist free medical journals Physiotherapist famous journals Physiotherapist Google Scholar indexed journals Rehabilitation articles Rehabilitation Research articles Rehabilitation review articles Rehabilitation PubMed articles Rehabilitation PubMed Central articles Rehabilitation 2023 articles Rehabilitation 2024 articles Rehabilitation Scopus articles Rehabilitation impact factor journals Rehabilitation Scopus journals Rehabilitation PubMed journals Rehabilitation medical journals Rehabilitation free journals Rehabilitation best journals Rehabilitation top journals Rehabilitation free medical journals Rehabilitation famous journals Rehabilitation Google Scholar indexed journals Low back pain articles Low back pain Research articles Low back pain review articles Low back pain PubMed articles Low back pain PubMed Central articles Low back pain 2023 articles Low back pain 2024 articles Low back pain Scopus articles Low back pain impact factor journals Low back pain Scopus journals Low back pain PubMed journals Low back pain medical journals Low back pain free journals Low back pain best journals Low back pain top journals Low back pain free medical journals Low back pain famous journals Low back pain Google Scholar indexed journals Therapeutic exercises articles Therapeutic exercises Research articles Therapeutic exercises review articles Therapeutic exercises PubMed articles Therapeutic exercises PubMed Central articles Therapeutic exercises 2023 articles Therapeutic exercises 2024 articles Therapeutic exercises Scopus articles Therapeutic exercises impact factor journals Therapeutic exercises Scopus journals Therapeutic exercises PubMed journals Therapeutic exercises medical journals Therapeutic exercises free journals Therapeutic exercises best journals Therapeutic exercises top journals Therapeutic exercises free medical journals Therapeutic exercises famous journals Therapeutic exercises Google Scholar indexed journals Lumbar spine articles Lumbar spine Research articles Lumbar spine review articles Lumbar spine PubMed articles Lumbar spine PubMed Central articles Lumbar spine 2023 articles Lumbar spine 2024 articles Lumbar spine Scopus articles Lumbar spine impact factor journals Lumbar spine Scopus journals Lumbar spine PubMed journals Lumbar spine medical journals Lumbar spine free journals Lumbar spine best journals Lumbar spine top journals Lumbar spine free medical journals Lumbar spine famous journals Lumbar spine Google Scholar indexed journals Thoracolumbar fascia articles Thoracolumbar fascia Research articles Thoracolumbar fascia review articles Thoracolumbar fascia PubMed articles Thoracolumbar fascia PubMed Central articles Thoracolumbar fascia 2023 articles Thoracolumbar fascia 2024 articles Thoracolumbar fascia Scopus articles Thoracolumbar fascia impact factor journals Thoracolumbar fascia Scopus journals Thoracolumbar fascia PubMed journals Thoracolumbar fascia medical journals Thoracolumbar fascia free journals Thoracolumbar fascia best journals Thoracolumbar fascia top journals Thoracolumbar fascia free medical journals Thoracolumbar fascia famous journals Thoracolumbar fascia Google Scholar indexed journals Muscle behavior articles Muscle behavior Research articles Muscle behavior review articles Muscle behavior PubMed articles Muscle behavior PubMed Central articles Muscle behavior 2023 articles Muscle behavior 2024 articles Muscle behavior Scopus articles Muscle behavior impact factor journals Muscle behavior Scopus journals Muscle behavior PubMed journals Muscle behavior medical journals Muscle behavior free journals Muscle behavior best journals Muscle behavior top journals Muscle behavior free medical journals Muscle behavior famous journals Muscle behavior Google Scholar indexed journals Spinal stability articles Spinal stability Research articles Spinal stability review articles Spinal stability PubMed articles Spinal stability PubMed Central articles Spinal stability 2023 articles Spinal stability 2024 articles Spinal stability Scopus articles Spinal stability impact factor journals Spinal stability Scopus journals Spinal stability PubMed journals Spinal stability medical journals Spinal stability free journals Spinal stability best journals Spinal stability top journals Spinal stability free medical journals Spinal stability famous journals Spinal stability Google Scholar indexed journals Fracture articles Fracture Research articles Fracture review articles Fracture PubMed articles Fracture PubMed Central articles Fracture 2023 articles Fracture 2024 articles Fracture Scopus articles Fracture impact factor journals Fracture Scopus journals Fracture PubMed journals Fracture medical journals Fracture free journals Fracture best journals Fracture top journals Fracture free medical journals Fracture famous journals Fracture Google Scholar indexed journals Spinal stenosis articles Spinal stenosis Research articles Spinal stenosis review articles Spinal stenosis PubMed articles Spinal stenosis PubMed Central articles Spinal stenosis 2023 articles Spinal stenosis 2024 articles Spinal stenosis Scopus articles Spinal stenosis impact factor journals Spinal stenosis Scopus journals Spinal stenosis PubMed journals Spinal stenosis medical journals Spinal stenosis free journals Spinal stenosis best journals Spinal stenosis top journals Spinal stenosis free medical journals Spinal stenosis famous journals Spinal stenosis Google Scholar indexed journals Inflammatory disease articles Inflammatory disease Research articles Inflammatory disease review articles Inflammatory disease PubMed articles Inflammatory disease PubMed Central articles Inflammatory disease 2023 articles Inflammatory disease 2024 articles Inflammatory disease Scopus articles Inflammatory disease impact factor journals Inflammatory disease Scopus journals Inflammatory disease PubMed journals Inflammatory disease medical journals Inflammatory disease free journals Inflammatory disease best journals Inflammatory disease top journals Inflammatory disease free medical journals Inflammatory disease famous journals Inflammatory disease Google Scholar indexed journals Psychiatric illness articles Psychiatric illness Research articles Psychiatric illness review articles Psychiatric illness PubMed articles Psychiatric illness PubMed Central articles Psychiatric illness 2023 articles Psychiatric illness 2024 articles Psychiatric illness Scopus articles Psychiatric illness impact factor journals Psychiatric illness Scopus journals Psychiatric illness PubMed journals Psychiatric illness medical journals Psychiatric illness free journals Psychiatric illness best journals Psychiatric illness top journals Psychiatric illness free medical journals Psychiatric illness famous journals Psychiatric illness Google Scholar indexed journals Pulmonary disease articles Pulmonary disease Research articles Pulmonary disease review articles Pulmonary disease PubMed articles Pulmonary disease PubMed Central articles Pulmonary disease 2023 articles Pulmonary disease 2024 articles Pulmonary disease Scopus articles Pulmonary disease impact factor journals Pulmonary disease Scopus journals Pulmonary disease PubMed journals Pulmonary disease medical journals Pulmonary disease free journals Pulmonary disease best journals Pulmonary disease top journals Pulmonary disease free medical journals Pulmonary disease famous journals Pulmonary disease Google Scholar indexed journals Athletic performance articles Athletic performance Research articles Athletic performance review articles Athletic performance PubMed articles Athletic performance PubMed Central articles Athletic performance 2023 articles Athletic performance 2024 articles Athletic performance Scopus articles Athletic performance impact factor journals Athletic performance Scopus journals Athletic performance PubMed journals Athletic performance medical journals Athletic performance free journals Athletic performance best journals Athletic performance top journals Athletic performance free medical journals Athletic performance famous journals Athletic performance Google Scholar indexed journals Musculoskeletal articles Musculoskeletal Research articles Musculoskeletal review articles Musculoskeletal PubMed articles Musculoskeletal PubMed Central articles Musculoskeletal 2023 articles Musculoskeletal 2024 articles Musculoskeletal Scopus articles Musculoskeletal impact factor journals Musculoskeletal Scopus journals Musculoskeletal PubMed journals Musculoskeletal medical journals Musculoskeletal free journals Musculoskeletal best journals Musculoskeletal top journals Musculoskeletal free medical journals Musculoskeletal famous journals Musculoskeletal Google Scholar indexed journals
Article Details
1. Introduction
Low Back Pain (LBP) is a widespread health and socioeconomic issue that significantly contributes to disability worldwide. LBP scored as the most severe handicap in terms of years lived with disability, according to Global Burden of Disease 2010 research [1]. Furthermore, according to Hoy et al. [2] estimated the mean point prevalence, 1-year prevalence, and lifetime prevalence of LBP were, respectively, 18.3%, 38.0%, and 38.9%.
Lower extremities discomfort may or may not accompany low back pain, which causes pain that is localized between the costal margins and the inferior gluteal folds [3]. Nonspecific LBP (NSLBP), which has no known etiology or pathology, makes for more than 85% of LBP cases [4,5]. Patients with NSLBP have reduced postural control, which is necessary for performing functional activities [6]. The ocular, vestibular, and somatic sensory systems all contribute sensory information to the complex neuromuscular process of postural regulation [6-8].
Postural control requires both cerebral processing and motor output [9]. Proprioception is significantly affected in individuals with chronic LBP than in healthy controls, according to a comprehensive study [10]. LBP may have a potential mechanism involving proprioceptive deficits altering the motion of the lumbar spine [11,12]. Reduced proprioceptive acuity may affect a population's ability to achieve and maintain a neutral spinal position, muscle coordination, and consequently diminish balance control. Patients with LBP may experience discomfort, impairment, and recurrences of injury because of decreased postural control. Accordingly, impaired sensorimotor control may result from diminished proprioception in patients with LBP, which has been suggested to be either or both a cause and a result of their pain [13,14].
For patients with LBP, several types of therapeutic exercises are employed in clinical settings. The co-activation of the Transversus Abdominis (TrA) and LM muscles is emphasized in Core Stability Exercises (CSE), which are based on the motor learning method. By increasing intra-abdominal pressure, these deep stabilizing muscles stiffen the lumbar spine and give the spine segmental stability [15]. They link to the thoracolumbar fascia. Additionally, CSE can improve muscle behavior, undo pain-related restructuring in the motor cortex, and retrain local trunk muscles' critical role in the neuromuscular regulation of spinal stability [16]. In LBP patients, stabilization exercises have been shown to increase stability index, successfully correct postural abnormalities, and reduce pain and disability [17-20].
Treatment for patients with LBP frequently involves Strengthening Exercises (STE). For patients with subacute or chronic NSLBP, strengthening activities are appropriate because they activate the superficial trunk muscles that enable shock absorption of loads [21,22]. These exercises are meant to improve overall spinal stability by strengthening and controlling the global trunk muscles. In patients with NSLBP, these exercises may lessen discomfort and physical impairment while increasing trunk muscular activation [22]. Docherty et al. [23] claim that strength training can improve joint position awareness and strength in the ankle. A combination of central and spindle mechanisms or an improvement in the central mechanisms of motor control may result from strengthening training regimens [24,25]. No prior research has reported the effects of strengthening exercises on proprioception related to either the subacute or chronic stages of LBP.
Therefore, our primary purpose is to compare the effects of conventional and conventional with core stabilization exercise on pain and disability in patients with chronic low back pain. Our secondary purpose was to compare the effects of conventional and conventional with core stabilization exercise on pain and disability.
2. Methodology
An assessor-blinded randomized controlled trial will be performed after receiving the ethical permission of Ethics Committee; the study proposal will follow the CONSORT checklist and will be submitted for trial registration. It will be conducted at the Tertiary level rehabilitation centre. The intentions and processes of the study will be explained to the eligible participants, and they were asked to sign an informed consent form before their participation. The participants will be allocated into two groups, conventional physiotherapy group and the core stability group. An initial assessment will be done before and after intervention and after 4 weeks of treatment.
Inclusion and Exclusion Criteria: The inclusion criteria are: (a) male and female between 18 years and above, (b) primary complaint of LBP experienced at least over the previous 3 months, and (c) ability to cooperate with investigator. The participants exclusion criteria is: (a) previous history of thoracic spine or lumbosacral spine surgery, (b) Any neurological deficit or presence of red flag, (c) evidence of serious spine pathology (e.g., tumor, infection, fracture, spinal stenosis, inflammatory disease), (d) Unstable or severe disabling chronic cardiovascular and pulmonary disease, (e) History of serious psychological or psychiatric illness, and (f) current pregnancy.
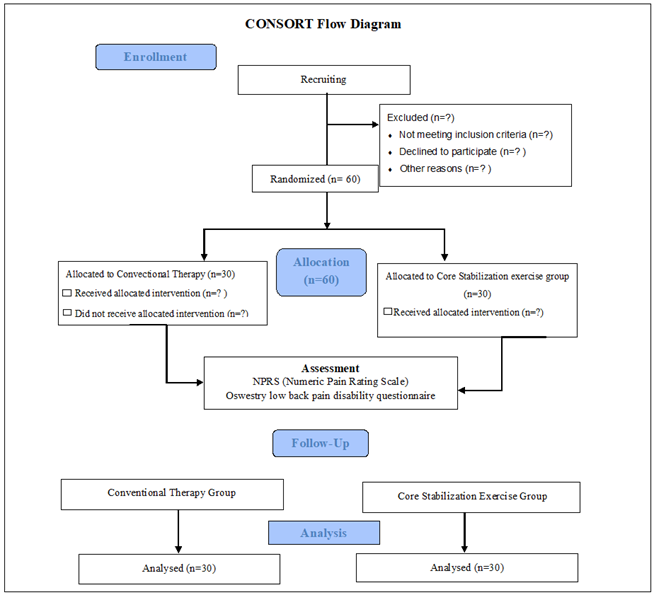
Figure 1: Consort flow diagram.
2.1 Outcome measurement
Functional disability (Oswestry low back pain disability questionnaire): The self-completed questionnaire asks 10 questions about ten different topics: pain intensity, lifting, ability to take care of oneself, walking, sitting, sexual function, standing, social life, sleep quality, and ability to travel. Six sentences detailing several possible events in the patient's life related to the topic follow each topic area. The patient then evaluates the statement that most accurately describes their circumstance. The first statement in each question receives a score of zero, signifying the least amount of handicap, and the last statement receives a score of five, signifying the most severe disability. To get the index, the answers to all questions are added together, then multiplied by two (range 0 to 100) [39].
Pain: The NPRS (numeric pain rating scale) is a segmented numerical version of the Visual Analog Scale (VAS), in which the respondent chooses an integer value between 0 and 10 that best describes the degree of their pain. Horizontal bars or lines are the most typical format. The 11-point numerical scale runs from 0 (which represents the least amount of pain, such as "no pain") to 10 (which represent the most extreme amount of pain, such as "pain as bad as you can conceive" or "worst pain imaginable") [40].
2.2 Intervention:
Conventional: Graduate physiotherapist will be involved in the treatment of patients. It will include McKenzie directional preference, Maitland and Mulligan technique and electro physical modalities.
Core stability exercise: The "cat" and "camel" stretches as well as a brief aerobic exercise might be included in the warm-up. Recognizing the neutral spine position, which is said to be the posture of power and balance for the best athletic performance in many sports, is the first step in a core stability training program [26]. Learning to activate the muscles of the abdominal wall is the first step in core stability training. It may take more time and practice for those who struggle with voluntary motor pathway activation, suffer from persistent low back pain, or exhibit fear-avoidance behavior to learn to recruit muscles alone or in conjunction with motor patterns [27,28]. A crucial first step is to cue people to hollow their abdomens, which may activate the transversus abdominis, as well as to brace their abdomens, which activate several muscles, including the transversus abdominis, external obliques, and internal obliques. According to one study, hollowing and bracing the abdomen before doing abdominal curls helped to activate the transversus abdominis and internal obliques during the abdominal curling exercise [29,30]. Training should be advanced once these activation techniques are mastered and the transversus abdominis is "awakened." The "major 3" exercises as outlined by McGill can then be incorporated by the beginner. These include the "bird dog" stance, the side bridge (also known as a side plank), and the curl-up. At this point, the prone plank and bridging can also be incorporated [28]. Pelvic bridging works very well to stimulate the lumbar paraspinals [31]. Supine, hook-lying, or quadruped positions are used for the first workouts. It should be emphasized that the spine should not be flattened or tilted but should instead maintain a neutral position. Additionally stressed is regular, rhythmic diaphragmatic breathing. After demonstrating strong control with the static core exercises, the person can move on to exercises including a physio ball. It should be noted that non-weight-bearing core exercises, such those done on a physio ball, could not result in better athletic performance [32]. Therefore, patients should move on to more practical activities in the sitting, standing, and walking positions as soon as possible. Focus should be given on improving balance and coordination while executing a variety of movement patterns in the three cardinal planes of movement sagittal, frontal, and transverse—as one advance through the early stages of a core strengthening program. Exercises ought to be done while standing and should imitate functional motions. Acceleration, deceleration, and dynamic stability are frequently needed during functional training. Reflexive control and postural regulation should be practiced in a sophisticated core stabilizing program [25].
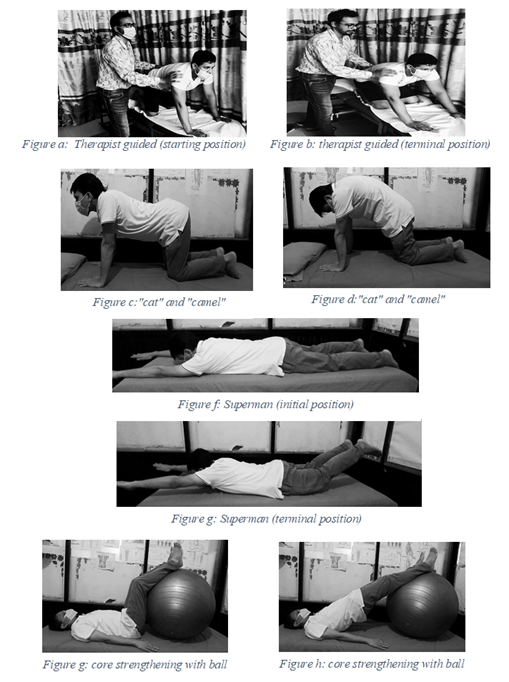
Figure 2: Core stabilization exercise.
2.3 Core strength training guidelines (FITT)
Frequency: 4 times a week. Intensity: Since all exercises will mostly done using subjects own body weight, one should focus on higher repetitions of 10 or more. Isometric contractions should be maintained for duration of time. (Ex. 15-20 seconds).
Time: 20-25 minutes.
Type: Body weighted exercises. During each exercise patient should contract your abdominal muscles as if patents were expecting to get hit in the stomach. Also, important to remember proper breathing techniques inhaling and exhaling on opposite movements.
The SPIRIT scheme diagram of the study schedule and management (Table 1); NPRS, Numeric Pain Rating Scale; ROM, Rang of Motion; -T1: pre-study, Screening/Consent T0: Baseline Randomization T2: Study, 2 weeks after intervention T3:4-weeks post assessment.
|
Time point |
Enrolment |
Allocation |
Post-allocation |
||
|
0 |
T0 |
T1 |
T2 |
T3 |
|
|
Enrolment |
|||||
|
Eligibility screen |
X |
|
|
|
|
|
Informed consent |
|
X |
|
|
|
|
Demographic Questionnaire |
|
X |
|
|
|
|
Allocation |
|
X |
X |
|
|
|
Intervention |
|
|
|
|
|
|
Core stability exercise |
|
|
X |
|
|
|
Patient education |
|
|
X |
|
|
|
Assessment |
|
|
|
|
|
|
NPRS |
|
X |
|
X |
X |
|
ROM |
|
X |
|
X |
X |
|
Oswestry low back pain disability questionnaire |
|
X |
|
X |
X |
Table 1: Sprit statement for RCT protocol.
2.4 Data analysis
Statistical analysis of data will be performed in Statistical Package for Social Science (SPSS), version 25.0. Statistical analysis will be performed according to nature of data. Normal distribution of the data will be test by kolmogorov smirnov test. In case of normal distribution parametric test will be performed.
2.5 Ethical consideration
Helsinki guidelines 2008 will be followed during the study periods. Initially a consent form will be given to each participant. This form explains the title, objective, confidentiality & anonymity of the research project. The participant will be also informed that, they are free to withdraw at any time. The researcher will keep the information in a secured place [33]. It will be explained to all the participants that their personal identity will be kept confidential, their name & address would not be written, except for social number or a pseudonym. Only principal investigator had the access of that information. Finally, the study will be reviewed and approved by the authorities.
3. Discussion
There is plenty of proof that people with persistent LBP and sacroiliac pain don't properly activate their core muscles and have weak cores [34-38]. Additionally, there is proof that people with chronic LBP have greater fatigability, a smaller cross section, and fatty infiltration of the paraspinal muscles [39]. These patients also appear to have less ability to adapt for unforeseen trunk disturbance and more problems with balance. Additionally, back pain sufferers appear to over-activate superficial global muscles, but deep spinal muscle control and activation are compromised. Therefore, core stability exercises offer a solid theoretical foundation for the treatment of spinal diseases as well as the prevention of various musculoskeletal conditions. Studies on LBP account for most of the level 1 evidence for stabilization exercises, which is mixed. Five randomized trials have, to our knowledge, supported stabilizing exercises for LBP [35]. However, several of these studies have methodological issues, among them are a dearth of real controls, a high attrition rate, and statistical irregularities [36]. The superiority of stabilizing exercises is also disputed by two other randomized trials [37]. Both studies' control groups featured generalized strengthening elements in addition to other characteristics [33]. Stabilization is useful for spinal problems, but it may not be better to other therapeutic exercise regimens, according to systematic reviews that have been conducted [38,40].
4. Results
This study will provide the effects of core stability exercise therapy with conventional physiotherapy compared to the conventional alone on pain and disability for chronic low back pain patient.
Author contributions
Md. Waliul Islam: Critical intellectual input, read and approval of the final submission, study concept and design, methodology, writing manuscript draft, study supervision.
Md. Tanzir-Uz-Zaman: Critical intellectual input, read and approval of the final submission, study concept and design, methodology, revision for critically intellectual content.
Md. Golam Kibria: Critical intellectual input, read and approval of the final sub- mission, study concept and design, methodology.
Abdullah Ibn Abul Fazal: Critical intellectual input, read and approval of the final sub- mission, study concept and design, methodology.
Md. Jubair Hassan: Critical intellectual input, read and approval of the final sub- mission, study concept and design, methodology.
Md. Mostafijur Rahman: Critical intellectual input, read and approval of the final sub- mission, study concept and design, methodology.
Saddam Hossain: Critical intellectual input, read and approval of the final submission, writing manuscript draft.
Md. Kutub Uddin: Critical intellectual input, read and approval of the final sub- mission, revision for critically intellectual content.
Mohammad Ainur Nishad Rhajib and Md Zakir Hossain: Critical intellectual input, read and approval of the final sub- mission, revision for critically intellectual content.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
First Author:
ORCiD https://orcid.org/0000-0003-1062-5349.
Corresponding Author:
ORCiD https://orcid.org/0000-0002-1952-9436.
Declaration of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Kuo CF, Grainge MJ, Mallen C, et al. Comorbidities in patients with gout prior to and following diagnosis: case-control study. Annals of the rheumatic diseases 75 (2016): 210-217.
- Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis and Rheumatism 64 (2012): 2028-2037.
- Chou R. Low back pain (chronic). Am Fam Physician 84 (2011): 437-438.
- Deyo RA, Weinstein JN. Low back pain. N Engl J Med 344 (2001): 363-370.
- Ehrlich GE. Low back pain. Bull World Health Organ 81 (2003): 671-676.
- Shumway-Cook A, Horak FB. Assessing the influence of sensory interac- tion of balance: suggestion from the field. Phys Ther 66 (1986): 1548-1550.
- Horak FB, Macpherson JM. Postural orientation and equilibrium. In: Shepard J, Rowell L, (Eds). Handbook of physiology, section 12. Exercise: regulation and integration of multiple systems. Oxford University, New York (1996): pp: 255-292.
- Chiba R, Takakusaki K, Ota J, et al. Human upright posture control models based on multisensory inputs, in fast and slow dynamics. Neurosci Res 104 (2016): 96-104.
- Han J, Waddington G, Adams R, et al. A proprioceptive ability underlying all proprioception tests? Response to tremblay. Percept Mot Skills 119 (2014): 30-34.
- Vickers NJ. Animal communication: when I’m calling you, will you answer too? Current biology 24 (2017): R713-15.
- Newcomer K, Laskowski ER, Yu B, et al. Repositioning error in low back pain: comparing trunk repositioning error in subjects with chronic low back pain and control subjects. Spine 25 (2000): 245.
- O’Sullivan PB, Burnett A, Floyd AN, et al. Lumbar repositioning deficit in a specific low back pain population. Spine 28 (2003): 1074-1079.
- van Dieën JH, Moseley GL, Hodges PW. Motor control changes and low back pain: cause or effect. Spinal control: the rehabilitation of back pain. State of the art and science 207 (2013): 207-218.
- Brumagne S, Diers M, Danneels L, et al. Neuroplasticity of sensorimotor control in low back pain. Journal of orthopaedic and sports physical therapy 49 (2019): 402-414.
- Vleeming A, Schuenke MD, Masi AT, et al. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. Journal of anatomy 221 (2012): 537-567.
- Tsao H, Druitt TR, Schollum TM, et al. Motor training of the lumbar paraspinal muscles induces immediate changes in motor coordination in patients with recurrent low back pain. J Pain 11 (2010): 11201128.
- Kim TH, Kim EH, Cho HY. The effects of the CORE programme on pain at rest, movement-induced and secondary pain, active range of motion, and proprioception in female office workers with chronic low back pain: a randomized controlled trial. Clin Rehabil 29 (2015): 653-662.
- Tsao H, Hodges PW. Persistence of improvements in postural strategies following motor control training in people with recurrent low back pain. J Electromyogr Kinesiol 18 (2008): 559-567.
- Hoffman SL, Johnson MB, Zou D, et al. Effect of classification-specific treatment on lumbopelvic motion during hip rotation in people with low back pain. Man Ther 16 (2011): 344-350.
- Salavati M, Akhbari B, Takamjani IE, et al. Effect of spinal stabilization exercise on dynamic postural control and visual dependency in subjects with chronic non-specific low back pain. J Bodyw Mov Ther 20 (2016): 441-448.
- Comerford MJ, Mottram SL. Movement and stability dysfunction–contemporary developments. Man Ther 6 (2001): 15-26.
- Koumantakis GA, Watson PJ, Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther 85 (2005): 209-25.
- Docherty CL, Moore JH, Arnold BL. Effects of strength training on strength development and joint position sense in functionally unstable ankles. J Athl Train 33 (1998): 310.
- Crowe A, Matthews PBC. The effects of stimulation of static and dynamic fusimotor fibres on the response to stretching of the primary endings of muscle spindles. J Physiol 174 (1964): 109-131.
- Appelberg b, bessou p, laporte y. Effects of dynamic and static fusimotor gamma fibres on responses of primary and secondary endings belonging to same spindle. In Journal of physiology London 177 (1965): 29.
- Barnet F, Gilleard W. The use of lumbar spinal stabilization techniques during the performance of abdominal strengthening exercise variations. J Sports Med Phys Fitness 45 (2005): 38Y43.
- Grenier SG, McGill SM. Quantification of lumbar stability by using two different abdominal activation strategies. Arch Phys Med Rehabil 88 (2007): 54Y62.
- Fredericson M, Moore T. Muscular balance, core stability, and injury prevention for middle-and long-distance runners. Physical Medicine and Rehabilitation Clinics 16 (2005): 669-689.
- Klenerman L, Slade PD, Stanley IM, et al. The prediction of chronicity in patients with an acute attack of low back pain in a general practice setting. Spine 20 (1995): 478Y484.
- Barnet F, Gilleard W. The use of lumbar spinal stabilization techniques during the performance of abdominal strengthening exercise variations. J Sports Med Phys Fitness 45 (2005): 38Y43.
- Grenier SG, McGill SM. Quantification of lumbar stability by using two different abdominal activation strategies. Arch Phys Med Rehabil 88 (20070: 54Y62.
- Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. Journal of Orthopaedic and Sports Physical Therapy 37 (2007): 290-302.
- Newcomer KL, Jacobson TD, Gabriel DA, et al. Muscle activation patterns in subjects with and without low back pain. Arch Phys Med Rehabil 83 (2002): 816Y821.
- Hungerford B, Gilleard W, Hodges P. Evidence of altered lumbopelvic muscle recruitment in the presence of sacroiliac joint pain. Spine 28 (2003): 1593-1600.
- Foster NE, Konstantinou K, Lewis M, et al. A randomized controlled trial investigating the efficacy of musculoskeletal physiotherapy on chronic low back disorder (comment). Spine 31 (2006): 2405Y2406.
- Koumantakis GA, Watson PJ, Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent lowback pain. Phys Ther 85 (2005): 209Y225.
- Slade SC, Keating JL. Trunk-strengthening exercises for chronic lowback pain: a systematic review. J Manipulative Physiol Ther 29 (2006): 163Y173.
- Hodges PW. Core stability exercise in chronic low back pain. Orthop Clin North Am 34 (2003): 245Y254.
- Fairbank JC, Pynsent PB. The Oswestry disability index. Spine 25 (2000): 2940-2953.
- Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain: Visual Analog Scale For Pain (vas pain), Numeric Rating Scale for Pain (nrs pain), Mcgill Pain Questionnaire (mpq), Short-Form Mcgill Pain Questionnaire (sf-mpq), Chronic Pain Grade Scale (cpgs), Short Form-36 Bodily Pain Scale (sf-36 bps), and measure of Intermittent and Constant Osteoarthritis Pain (icoap). Arthritis care and research 63 (2011): S240-S252.
