Early Femoral Failure in Two Patients Undergoing Downsizing of the Femoral Component During High-Flexion Total Knee Arthroplasty
Article Information
Ji-Hoon Baek, M.D.1, Su Chan Lee, M.D. 1, Seung Hyun Hwang, M.D. 2, Taehyeon Kim, M.D. 1, Hye Sun Ahn, M.S. 1, Chang Hyun Nam, M.D. 1*
1Joint and Arthritis Research, Department of Orthopaedic Surgery, Himchan Hospital, Seoul, Republic of Korea
2Department of Orthopaedic Surgery, Himnaera Hospital, Busan, Republic of Korea
*Corresponding Author: Chang Hyun Nam, Joint and Arthritis Research, Department of Orthopaedic Surgery, Himchan Hospital, 120, Sinmok-ro, Yangcheon-gu, Seoul, 07999, Republic of Korea
Received: 03 April 2023; Accepted: 17 April 2023; Published: 26 April 2023
Citation: Ji-Hoon Baek, Su Chan Lee, Seung Hyun Hwang, Taehyeon Kim, Hye Sun Ahn, Chang Hyun Nam. Early Femoral Failure in Two Patients Undergoing Downsizing of the Femoral Component During High-Flexion Total Knee Arthroplasty. Archives of Clinical and Medical Case Reports. 7 (2023): 162-165.
Share at FacebookAbstract
Introduction and Importance: High-flexion prostheses can be associated with a greater risk of early aseptic loosening of the femoral component than standard prosthesis.
Case presentation: We describe two patients in whom high-flexion total knee arthroplasty (TKA) was performed using the anterior referencing (AR) method that resulted in early aseptic loosening of the downsized femoral component.
Conclusion: Excessive bone resection of the posterior femoral condyle by additional downsizing of the femoral component during high-flexion TKA using the AR method could lead to early failure of the femoral component.
Keywords
Early aseptic loosening; Total knee arthroplasty; Anterior referencing; Downsizing
Article Details
1. Introduction
High-flexion total knee arthroplasty (TKA) designs were developed to facilitate maximum post-operative flexion. However, concerns have been raised regarding early aseptic loosening of the femoral component in the design of high-flexion TKA during the postoperative phase [1, 2]. There have been reports of higher revision rates due to aseptic loosening of the femoral component in some high-flexion designs [3-5]. We report two cases of patients in whom high-flexion TKA was performed using the anterior referencing (AR) method that resulted in early aseptic loosening of the downsized femoral component. The work has been reported in accordance with the SCARE 2020 criteria [6].
2. Presentation of Case
2.1. Case 1
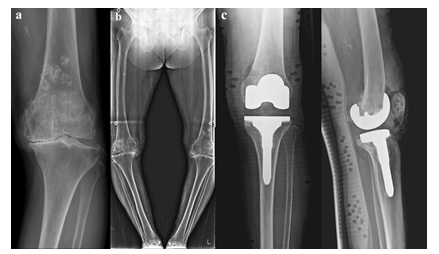
A 77-year-old female patient who complained of serious pain in the left knee for the preceding 10 years presented to our clinic in December 2018. She was 146.0 cm in height and 54.0 kg in weight with a body mass index of 25.3 kg/m2. She had a medical history of hypertension and diabetes mellitus. The patient displayed difficulty in walking because of her left knee pain, and she had experienced no improvement of her symptoms after receiving medication and injection treatment at another clinic. The physical examination revealed a large effusion and pain with range of motion in the left knee. Kellgren-Lawrence (K-L) grade IV osteoarthritic change of the left knee was documented (Figure 1a). The Hospital for Special Surgery (HSS) score for the left knee was 45. A weight-bearing x-ray revealed a varus deformity, and the hip-knee-ankle (HKA) angle was 21.0° (Figure 1b).
The patient underwent a left TKA (Figure 1c) performed by an experienced knee surgeon using the posterior-stabilized (PS) high-flexion LOSPA total knee prosthesis (Corentc, Seoul, Korea). The knee was exposed with a standard anterior midline incision via the medial parapatellar approach, and the patella was everted laterally. The anterior cruciate ligament was resected from the femoral notch and tibial insertions, and the posterior cruciate ligament was removed from the notch. The intramedullary canal was accessed by twist drilling a hole located about 1 cm anterior to the center of the intercondylar notch. After setting the instrument to the desired angle and placing it in the appropriate notch, distal femoral resection was conducted. The AP sizer on the resected distal femur was positioned, and proper femoral size and rotation were determined by the anterior referencing (AR) method. The femoral size was changed from size 6 to size 4 in order to increase the flexion gap. The remaining four femoral bone resections and box cutting were performed. Tibial cuts with a 2° posterior slope in the sagittal plane were made with a tibial extramedullary resection guide. Stability and alignment were assessed using the trial components. Femoral trial assessment (size 4) and tibial trial assessment (size 4) were performed. The femoral and tibial implants were inserted using bone cement, and the use of a polyethylene liner (16mm) was deemed appropriate and was also inserted. The patient was advised to perform immediate weight-bearing as tolerated, and active exercise was initiated under the supervision of a physiotherapist during rehabilitation.
Figure 1: a. Anteroposterior radiograph of a 77-year-old female patient who developed Kellgren-Lawrence Grade IV osteoarthritic change in the left knee. b. A standing AP radiograph of the bilateral lower extremities of the same patient preoperatively, which shows a left hip-knee-ankle angle of 21.0°. c. Radiograph following left total knee arthroplasty (TKA) with a 16mm polyethylene liner (femoral component: size 4, tibial component: size 4).
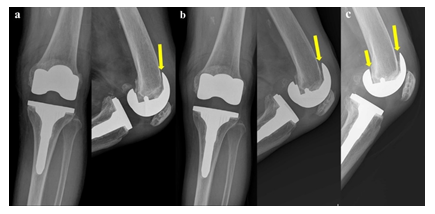
Three months following the TKA, the patient complained of mild pain in the left knee, especially on walking. Clinical examination revealed no restriction of movement and no tenderness on the left knee. Laboratory studies including a complete blood-cell and differential count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) level were within normal limits, and there was no clinical evidence of infection. Plain lateral radiographs demonstrated a radiolucent line beneath the anterior flange of the femoral component (Figure 2a). Radiolucency beneath the anterior flange indicated early loosening of the femoral component. The surgeon decided to prescribe medication and observe progress because the pain was not severe. Six months post-operatively, the patient complained of global pain in the left knee joint as well as tenderness and swelling. She reported aggravation of pain when her full body weight was loaded onto her knee joint. Plain lateral radiographs demonstrated a progressive radiolucent line and osteolysis beneath the anterior flange of the femoral component (Figure 2b). The femoral component was not well positioned in the lateral plane in the sitting flexion position (Figure 2b). One year post-operatively, plain lateral radiographs demonstrated a progressive radiolucent line and osteolysis around the anterior and posterior flanges of the femoral component (Figure 2c).
Currently, the patient does not want to undergo revision TKA, so we are monitoring the patient once every six months in an outpatient clinic.
Figure 2: Radiographs showing early failure of the femoral component. a. Three months after TKA. Lateral radiograph showing a radiolucent line at the anterior surface of the femoral component (yellow arrow). b. Six months after TKA. Lateral radiograph showing a progressive radiolucent line and osteolysis beneath the anterior flange of the femoral component (yellow arrow). c. One year after TKA. Lateral radiograph showing a progressive radiolucent line and osteolysis around the anterior (yellow arrow) and posterior (short yellow arrow) flanges.
2.2. Case 2
A 70-year-old female patient who complained of serious pain in the right knee for the preceding five years presented to our clinic in January 2019. She was 150.0 cm in height and 61.0 kg in weight with a body mass index of 27.1 kg/m2. She had a medical history of hypertension and diabetes mellitus.
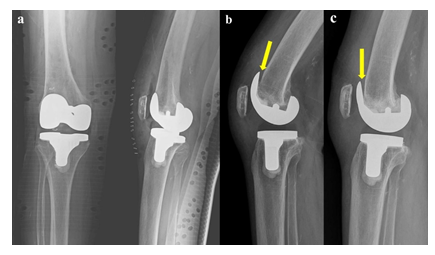
One month post-operatively, the patient complained of global pain in the right knee joint. Plain lateral radiograph demonstrated a radiolucent line beneath the anterior flange of the femoral component (Figure 3b). Three months post-operatively, a plain lateral radiograph demonstrated a progressive radiolucent line and osteolysis beneath the anterior flange of the femoral component (Figure 3c). The femoral component was not well positioned in the lateral plane in the sitting flexion position. (Figure 3c).
Currently, the patient does not want to undergo revision TKA; therefore, we are monitoring the patient once every six months in an outpatient clinic.
Figure 3: a. A 70-year-old female patient underwent right TKA with a 12mm polyethylene liner (femoral component: size 4, tibial component: size 4). b. One month after TKA. Lateral radiograph showing a radiolucent line beneath the anterior flange of the femoral component (yellow arrow). c. Three months after TKA. Lateral radiograph showing a progressive radiolucent line and osteolysis beneath the anterior flange of the femoral component (yellow arrow).
3. Discussion
The purpose of this report is to caution surgeons on the risks associated with excessive downsizing of the femoral component during high-flexion TKA using the AR method. Excessive downsizing can result in early failure of the femoral component due to additional removal of bone from the posterior femoral condyle. Aseptic loosening of the femoral component after TKA is considered a relatively rare complication. We had never experienced early failure of the femoral component within three months postoperatively prior to the present cases.
Several studies have expressed concerns about the increased risk of femoral loosening in high-flexion knee prostheses compared to standard prosthesis as the load on the knee joint increases considerably during deep flexion [7, 8]. There have been reports of early failure of the femoral component in some high-flexion prostheses [3-5]. Han et al. [3] reported a high incidence of femoral aseptic loosening in 38% (27/72 knees) of their cases treated with high-flexion TKA during a mean follow-up of 23 months. This group proposed that early failure of the femoral component could be attributed to certain characteristics of the implant design, the increased load on the knee during deep flexion, and an implant-cement interface problem. King and Scott [9] suggested that early loosening of the femoral component was initiated by inadequate support of the posterior femoral condyle that might be related to inaccurate bone cuts, deficient bone stock, or poor cementing technique. In our cases, failure of the femoral component proceeded within weeks postoperatively, and we assumed that this phenomenon was more related to surgical techniques than to implant design. The surgeon performed primary TKA using the anterior referencing (AR) method and chose two levels of femoral component downsizing to widen the flexion gap in these patients. The advantages of the AR method are re-approximation of the patellofemoral joint and reduced risk of notching of the anterior femoral cortex. However, the disadvantage is that excessive resection of the posterior condylar bone can occur. In addition, the excessive downsizing of the femoral component to widen the flexion gap can lead to additional resection of the posterior condylar bone. We suggested that early failure of the femoral component might be related to excessive bone resection of the posterior femoral condyle that might have resulted from femoral component downsizing in high-flexion TKA using the AR method.
4. Conclusion
We have expressed concerns about excessive bone resection of the posterior femoral condyle by additional downsizing of the femoral component in high-flexion TKA using the AR method, which could lead to early failure of the femoral component.
Conflicts of Interest
Each author certifies that he or she has no commercial association (eg. consultancies, stock ownership, equity interest, patent, licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Ethics Approval
This study was approved by the Institutional Review Board of our institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- Zelle J, Janssen D, Van Eijden J, et al. Does high-flexion total knee arthroplasty promote early loosening of the femoral component? J Orthop Res 29 (2011): 976-983.
- Bollars P, Luyckx JP, Innocenti B, et al. Femoral component loosening in high-flexion total knee replacement: an in vitro comparison of high-flexion versus conventional designs. J Bone Joint Surg Br 93 (2011): 1355-1361.
- Han HS, Kang SB, Yoon KS. High incidence of loosening of the femoral component in legacy posterior stabilised-flex total knee replacement. J Bone Joint Surg Br 89 (2007): 1457-1461.
- Cho SD, Youm YS, Park KB. Three- to six-year follow-up results after high-flexion total knee arthroplasty: can we allow passive deep knee bending? Knee Surg Sports Traumatol Arthrosc 19 (2011): 899-903.
- Jung WH, Jeong JH, Ha YC, et al. High early failure rate of the Columbus posterior stabilized high-flexion knee prosthesis. Clin Orthop Relat Res 470 (2012): 1472-1481.
- Agha RA, Franchi T, Sohrabi C, Mathew G, for the SCARE Group. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 84 (2020): 226-230.
- Dahlkvist NJ, Mayo P, Seedhom BB. Forces during squatting and rising from a deep squat. Eng Med 11 (1982): 69-76.
- Zelle J, Barink M, De Waal MM, et al. Thigh-calf contact: does it affect the loading of the knee in the high-flexion range? J Biomech 42 (2009): 587-593.
- King TV, Scott RD. Femoral component loosening in total knee arthroplasty. Clin Orthop Relat Res 194 (1985): 285-290.