Dural Repair by Direct Continuous Locking Sutures and Concomitant Insertion of Subfascial Tube in Planned Intradural Spinal Cord Tumor Surgery
Article Information
Ramadan Shamseldein*
Lecturer of Neurosurgery, Department of Neurosurgical, Elsahil teaching hospital, Cairo, Egypt
*Corresponding Author: Ramadan Shamseldein, Lecturer of Neurosurgery, Department of Neurosurgical, Elsahil teaching hospital, Cairo, Egypt
Received: 06 December 2020; Accepted: 14 December 2020; Published: 16 December 2020
Citation:
Ramadan Shamseldein. Dural Repair by Direct Continuous Locking Sutures and Concomitant Insertion of Subfascial Tube in Planned Intradural Spinal Cord Tumor Surgery. Journal of Spine Research and Surgery 2 (2020): 130-137.
Share at FacebookAbstract
Background: Durotomy induced cerebrospinal fluid (CSF) leakage is a terrible complication in spine surgery that could be occurred even with expertise. The estimated rate of CSF leakage in intentional durotomies varies from 5 to 13% in intradural spinal tumor resection to even higher rate for surgeries for tethered cord syndrome or Chiari I malformation. Different treatment modalities are utilized as conservative measures, direct sutures, autograft, dural substitutes and sealant agents to overcome this complication.
Patient and method: This is a retrospective descriptive study of thirty patients were operated upon at neurosurgery department of Elsahil teaching hospital from November 2014 to November 2019. They were operated for intradural spinal cord tumor excision followed by primary direct sutural repair of the durotomy site augmented with autograft and concomitant insertion of subfascial tube as a drainage tube for seven to ten days.
Aim: To evaluate the results of primary direct dural repair with continuous locking sutures and on lay gel foam layer augmented with autograft (fat or muscle) without sealant agents. With concomitant insertion of subfascial tube closed system as drainage in planned intradural surgery.
Results: After subfascial tube removal three cases (10%) show persistent leakage that managed conservatively with tapering cessation within three weeks till complete cessation of the CSF leakage occur. One of the three cases developed pseudomeningocele (3.3%) after complete wound closure and cessation of the leakage.
Conclusion: Direct sutural repair of the durotomy site with continuous locking sutural closure and on lay gel foam layer and fat or muscle graft without any sealant agents, and concomitant insertion of subfascial tube closed system as a drainage tube for seven to ten days, is effective and safe e
Keywords
Cerebrospinal Fluid, Subfascial Tube
Cerebrospinal Fluid articles Cerebrospinal Fluid Research articles Cerebrospinal Fluid review articles Cerebrospinal Fluid PubMed articles Cerebrospinal Fluid PubMed Central articles Cerebrospinal Fluid 2023 articles Cerebrospinal Fluid 2024 articles Cerebrospinal Fluid Scopus articles Cerebrospinal Fluid impact factor journals Cerebrospinal Fluid Scopus journals Cerebrospinal Fluid PubMed journals Cerebrospinal Fluid medical journals Cerebrospinal Fluid free journals Cerebrospinal Fluid best journals Cerebrospinal Fluid top journals Cerebrospinal Fluid free medical journals Cerebrospinal Fluid famous journals Cerebrospinal Fluid Google Scholar indexed journals Subfascial Tube articles Subfascial Tube Research articles Subfascial Tube review articles Subfascial Tube PubMed articles Subfascial Tube PubMed Central articles Subfascial Tube 2023 articles Subfascial Tube 2024 articles Subfascial Tube Scopus articles Subfascial Tube impact factor journals Subfascial Tube Scopus journals Subfascial Tube PubMed journals Subfascial Tube medical journals Subfascial Tube free journals Subfascial Tube best journals Subfascial Tube top journals Subfascial Tube free medical journals Subfascial Tube famous journals Subfascial Tube Google Scholar indexed journals Spinal Cord Tumor articles Spinal Cord Tumor Research articles Spinal Cord Tumor review articles Spinal Cord Tumor PubMed articles Spinal Cord Tumor PubMed Central articles Spinal Cord Tumor 2023 articles Spinal Cord Tumor 2024 articles Spinal Cord Tumor Scopus articles Spinal Cord Tumor impact factor journals Spinal Cord Tumor Scopus journals Spinal Cord Tumor PubMed journals Spinal Cord Tumor medical journals Spinal Cord Tumor free journals Spinal Cord Tumor best journals Spinal Cord Tumor top journals Spinal Cord Tumor free medical journals Spinal Cord Tumor famous journals Spinal Cord Tumor Google Scholar indexed journals cerebellar hemorrhage articles cerebellar hemorrhage Research articles cerebellar hemorrhage review articles cerebellar hemorrhage PubMed articles cerebellar hemorrhage PubMed Central articles cerebellar hemorrhage 2023 articles cerebellar hemorrhage 2024 articles cerebellar hemorrhage Scopus articles cerebellar hemorrhage impact factor journals cerebellar hemorrhage Scopus journals cerebellar hemorrhage PubMed journals cerebellar hemorrhage medical journals cerebellar hemorrhage free journals cerebellar hemorrhage best journals cerebellar hemorrhage top journals cerebellar hemorrhage free medical journals cerebellar hemorrhage famous journals cerebellar hemorrhage Google Scholar indexed journals intracranial subdural hematoma articles intracranial subdural hematoma Research articles intracranial subdural hematoma review articles intracranial subdural hematoma PubMed articles intracranial subdural hematoma PubMed Central articles intracranial subdural hematoma 2023 articles intracranial subdural hematoma 2024 articles intracranial subdural hematoma Scopus articles intracranial subdural hematoma impact factor journals intracranial subdural hematoma Scopus journals intracranial subdural hematoma PubMed journals intracranial subdural hematoma medical journals intracranial subdural hematoma free journals intracranial subdural hematoma best journals intracranial subdural hematoma top journals intracranial subdural hematoma free medical journals intracranial subdural hematoma famous journals intracranial subdural hematoma Google Scholar indexed journals spinal dura mater articles spinal dura mater Research articles spinal dura mater review articles spinal dura mater PubMed articles spinal dura mater PubMed Central articles spinal dura mater 2023 articles spinal dura mater 2024 articles spinal dura mater Scopus articles spinal dura mater impact factor journals spinal dura mater Scopus journals spinal dura mater PubMed journals spinal dura mater medical journals spinal dura mater free journals spinal dura mater best journals spinal dura mater top journals spinal dura mater free medical journals spinal dura mater famous journals spinal dura mater Google Scholar indexed journals cervicodorsal spine articles cervicodorsal spine Research articles cervicodorsal spine review articles cervicodorsal spine PubMed articles cervicodorsal spine PubMed Central articles cervicodorsal spine 2023 articles cervicodorsal spine 2024 articles cervicodorsal spine Scopus articles cervicodorsal spine impact factor journals cervicodorsal spine Scopus journals cervicodorsal spine PubMed journals cervicodorsal spine medical journals cervicodorsal spine free journals cervicodorsal spine best journals cervicodorsal spine top journals cervicodorsal spine free medical journals cervicodorsal spine famous journals cervicodorsal spine Google Scholar indexed journals MRI articles MRI Research articles MRI review articles MRI PubMed articles MRI PubMed Central articles MRI 2023 articles MRI 2024 articles MRI Scopus articles MRI impact factor journals MRI Scopus journals MRI PubMed journals MRI medical journals MRI free journals MRI best journals MRI top journals MRI free medical journals MRI famous journals MRI Google Scholar indexed journals low back pain articles low back pain Research articles low back pain review articles low back pain PubMed articles low back pain PubMed Central articles low back pain 2023 articles low back pain 2024 articles low back pain Scopus articles low back pain impact factor journals low back pain Scopus journals low back pain PubMed journals low back pain medical journals low back pain free journals low back pain best journals low back pain top journals low back pain free medical journals low back pain famous journals low back pain Google Scholar indexed journals L4 vertebral body articles L4 vertebral body Research articles L4 vertebral body review articles L4 vertebral body PubMed articles L4 vertebral body PubMed Central articles L4 vertebral body 2023 articles L4 vertebral body 2024 articles L4 vertebral body Scopus articles L4 vertebral body impact factor journals L4 vertebral body Scopus journals L4 vertebral body PubMed journals L4 vertebral body medical journals L4 vertebral body free journals L4 vertebral body best journals L4 vertebral body top journals L4 vertebral body free medical journals L4 vertebral body famous journals L4 vertebral body Google Scholar indexed journals
Article Details
1. Introduction
Durotomy induced cerebrospinal fluid (CSF) leakage is a terrible complication in spine surgery that could be occurred even with expertise, the current reported incidence of durotomy and eventually CSF leaks varies between (1, 6% and 17, 4%) [1-3]. The estimated rate of CSF leakage in intentional durotomies varies from 5 to 13% in intradural spinal tumor resection to even higher rate for surgeries for tethered cord syndrome or Chiari I malformation [4, 10]. The cases complicated with CSF leakage clinically presented with postural headache, may be associated with nausea, vomiting, dizziness, and photophobia. Also Persistent CSF leak often leads to formation of paraspinal muscel fluid pockets, and a pseudomeningocele or a dural cutaneous fistula, these conditions lead to infective states as meningitis, or abscesses [5]. Serious but rare complications may also occur in case of persistent leakage of the CSF as cerebellar hemorrhage and intracranial subdural hematoma [6]. Persistent CSF leakage can be first managed by conservative strategies such as the use of brace, bedrest, lumbar intrathecal drain, or epidural blood patches and these are typically sufficient during the postoperative course a surgical revision is rarely needed [5, 11]. For planned intradural surgery, post durotomy primary direct suture watertight closure is critical step in the treatment and prevention of CSF leakage and its complications. Grafting materials such as muscle, fascia and or fat are usually utilized concomitant with direct suture watertight closure. Adjunctive to direct repair and grafting the use of a collagen based dural implant and/or a sealant also utilized [7].
Although many sealant agents and collagen based dural implant existed, none of them appeared to be superior for dural repair when compared to the others. Also, surgery with combined use of multiple dura closure substitutes is associated with the enhanced incidence of postoperative CSF leaks, probably due to the more complicated surgical conditions in these cases [11]. Post intradural tumor surgery direct repair with suture is typically done. The controversial issue is the effectiveness of different sutural materials and the way they utilized for the repair. Some reports support interrupted sutures, and other studies showing similar outcomes with interrupted and running techniques [8]. Some authors advocated postoperative subfascial drainage, which is used in concomitant with watertight layered wound closure to decrease the subfascial space pressure and so, would facilitate wound healing. When it is left from seven to ten days, the wound resistance would be strong enough to withstand the subarachnoid pressure and retard CSF leak at the durotomy site and accordingly facilitate the healing of damaged spinal dura mater [9].
2. Patient and Method
This is a retrospective descriptive study of thirty patients were operated upon at neurosurgery department of Elsahil teaching hospital from November 2014 to November 2019.Fifteen males, and fifteen females. They were operated for intradural spinal cord tumor excision followed by primary direct sutural repair of the durotomy site with continuous locking watertight sutural closure and on lay gel foam layer and fat or muscle graft without any sealant agents. Concomitant insertion of subfascial tube (none suction tube) closed system as a drainage tube for seven to ten days.
2.1 Aim of the work
To evaluate the results of primary direct dural repair with continuous locking sutures and on lay gel foam layer augmented with autograft (fat or muscle) without sealant agents. Concomitant insertion of subfascial tube closed system as drainage. This offered to the cases of post intradural spinal cord tumor surgery durotomy repair.
2.2 Surgical procedure
All procedures throughout this study were performed by the author and his team. The surgical incision was sutured layer by layer and it is imperative that the wound closure is so watertight that it could withstand the strength of the Valsalva maneuver at the conclusion of the suture repair. Primary direct sutural repair of the durotomy site utilizing continuous locking sutures by vicryle 4/0 followed by on lay gel foam layer, fat and or muscle graft without any other sealant agents. The most important deep fascial layer of wound closure was accomplished in an interrupted fashion. The drainage tube non suction simple nelaton tube (12fr-14fr-or 16fr) was placed in the subfascial space close to the durotomy site, connected sterile collecting bag to ensure a closed drainage system. The skin entry site of drainage tube was covered with a transparent waterproof dressing in order to ensure sterility. The collection bag was kept on the patient's bed to avoid gravity drainage of CSF and patient was requested to rest on bed during the postoperative wound drain period. Additionally, the drainage bag was changed every 24 h with strict aseptic measures and wound dressing was done every 24h. postoperatively patients were given third generation cephalosporin (2 g/day, tid) for 7 days.
3. Results
This is a retrospective descriptive study of thirty patient’s fifteen males, and fifteen females. Age ranged from 12 years to 72 years (mean age 41.37 years), (Table 1). They were operated for intradural spinal cord tumor excision followed by primary direct sutural repair of the durotomy site with continuous locking watertight sutural closure and on lay gel foam layer and fat or muscle graft without any sealant agents. Insertion of subfascial tube closed system as a drainage tube for seven to ten days. After subfascial tube removal three cases (10%) show persistent leakage that managed conservatively with tapering cessation within three weeks till complete cessation of the CSF leakage occur. One of the three cases developed pseudomeningocele (3.3%) after complete wound closure and cessation of the leakage. The study group was thirty patients’ fifteen females and fifteen males. Mean age was 41.37 years.
|
Variables |
The study group (n=30) |
|
Age/ years |
|
|
Mean ± SD |
41.37 ± 17.38 |
|
Min-Max |
3.0-72 |
|
Sex |
|
|
Male |
15 (50%) |
|
Female |
15 (50%) |
Table 1: Demographic data among the studied group.
|
Type of dural closure (n=30) |
Postoperative CSF leakage |
||
|
Direct continuous locking water tight suture |
30 (100%) |
CSF leakage |
3 (10%) |
|
No leakage |
27 (90%) |
||
Table 2: post-operative CSF leakage.
4. Case Presentation
4.1 Case 1 (the case of pseudomeningocele)
Male patient 59 years old presented with left upper extremity numbness and tingling and left lower extremity weakness G4 and exaggerated deep reflexes at left lower extremity and planter extensor response on
the left foot. He was continent to both urine and stool. MRI cervicodorsal spine show intradural extramedullary relatively hyperintense space occupying lesion compressing the cord from left to right and occupying most of the left side. The pathology was transitional meningioma.
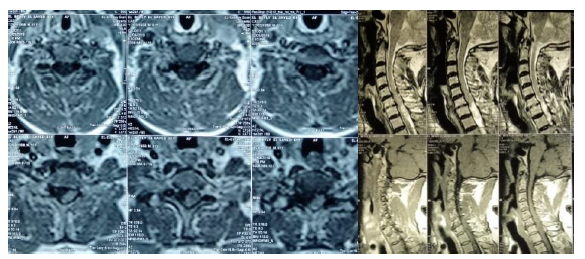
Figure 1a: Preoperative MRI Cervicothoracic spine with contrast show intradural extramedullary Sol at C7D1level.
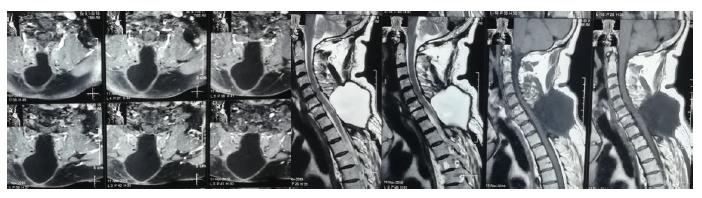
Figure 1b: follow up contrast enhanced MRI. After three weeks after complete wound closure and complete cessation of CSF leakage.
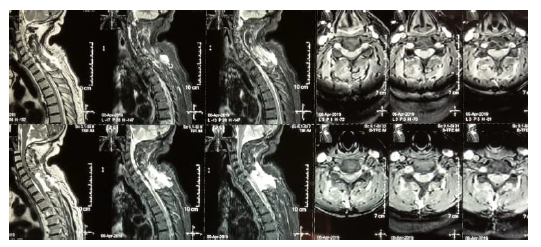
Figure 1c: late follow up five months post-operative of the same case. Show regressive course of the pseudomeningocele after conservative measures.
4.2 Case 2
Female patient 27 years old suffering low back pain bilateral lower extremity pain from thigh to feet associated with blow knee weakness G3 on RT side and G4 on Lt side and she is continent. Contrast lumbosacral MRI show intradural extramedullary enhanced lesion at L3-L4 level and L4 vertebral body. Operated totally excised and patient regain the full motor power and follow up MRI after three months good healing for all wound layers from dura to the skin and no residual lesion. The lesion histopathologically was schwannoma.
Figure 2a: Preoperative MRI.
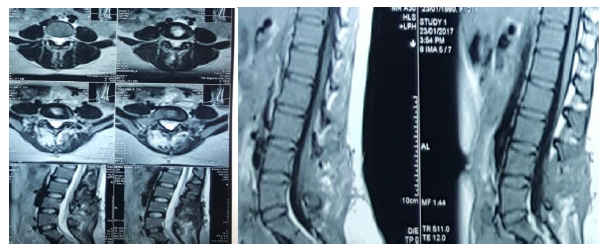
Figure 2b: Postoperative MRI.
4.3 Case
Female patient 47years suffering progressive paraparesis G4, urinary urgency, no sensory level. MRI cervicodorsal spine show intradural extramedullary lesions at D2 level relatively Isointense with contrast. Operated, totally excised and patient regain the full motor power and voiding control. Late follow up MRI after three years, good healing for all wound layers from dura to the skin and no residual lesion. The lesion histopathologically was psammomatous meningioma.
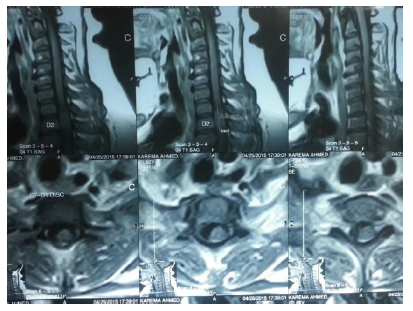
Figure 3a: Preoperative MRI.
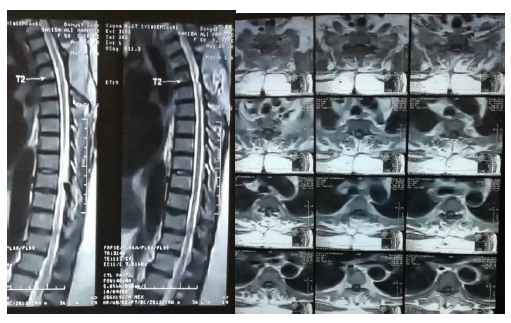
Figure 3b: Postoperative MRI.
5. Discussion
Post spinal surgery CSF leakage is the worst scenario for spine surgeon even with expertise. The reported incidence of literatures varied from 1,6% to 17,4% [1-3]. The highest reported incidence occur post intradural spinal cord tumor surgery is up to 13% which may increase more than that in case of Chiari I malformation surgery and surgery on tethered cord [4, 10]. In this work the studied group was operated upon for intradural spinal cord tumors. The complicated cases of post-operative persistent CSF leakage were 10% which is in accordance to reported data from Jenkinson et al 2006 and Danish SF et al 2006 about that context where it was ranged from 5 to 13%. The main stay for dural repair in intradural surgery is direct watertight closure plus utilization of autograft materials, in adjunctive to different types of sealants, but none of these agents appeared to be superior for dural repair when compared to the others [7, 11]. As the issue of the way to get water tight dural closure is still controversial, in this work the way for dural closure was, direct repair with continuous locking sutures augmented by on lay gel foam layer and autograft without sealants, with concomitant insertion of subfascial non suction tube closed system as a drainage tube for seven to ten days.
By this mean we depend on prevention of the leakage by the direct repair augmented with autograft, increasing the resistance of the wound to the leakage by layered water tight closure, and decreasing the subarachnoid space pressure through subfascial tube insertion and bed rest. This is in concordance to Zhao Fang et al 2017 where they reported a failure rate of 5%-9% for standalone direct sutural repair, and they suggest multimodality methods for repair aiming at prevention of CSF leakage and decreasing the subarachnoid space pressure [12]. This simple economic way for repair reducing the complication of postoperative CSF leakage with the reported range, in accordance to Jenkinson et al 2006 and Danish SF et al 2006 and responding well to the conservative follow up measures in the postoperative course. In case of persistent post-operative CSF leakage, the conservative measures are typically sufficient in the postoperative course to manage that condition, and the shift to surgical repair is rarely needed11. In this work the reported three cases of persistent post-operative CSF leakage were managed conservatively and complete regression were obtained within the first three weeks postoperatively, and the shift to surgical revision wasn’t needed. Sun et al 2012, reported success rate of 91.8%, effectiveness for the conservative comprehensive measures and only 8.2% require shift to redo surgical repair and failed conservative measures [13]. So, conservative measures for persistent CSF leakage after augmented direct repair, is effective strategy with least chance for reoperation.
6. Conclusion
In planned intradural surgery as the case in intradural spinal cord tumors. Direct sutural repair of the durotomy site with continuous locking sutural closure and on lay gel foam layer and fat or muscle graft without any sealant agents, and concomitant insertion of subfascial tube closed system as a drainage tube for seven to ten days, is effective and safe economic method for dural repair. With this method the possible occurrence of postoperative persistent CSF leakage lies within the recorded range in the literature about 10%. In case of persistent CSF leakage after augmented direct repair by this method the conservative measures is very effective and need for redo surgery is rarely needed.
References
- Baker GA, Cizik AM, Bransford RJ, et al. Risk factors for unintended durotomy during spine surgery: a multivariate analysis. Spine J 12 (2012): 121e126.
- Adam D, Papacocea T, Iliescu R, et al. Moisescu (2015): Incidental durotomy in lumbar spine surgery incidence,risk factors and management. Romanian Neurosurgery 22 (2015).
- Serdal Albayrak, Sait Ozturk, Omer Ayden, et al. Dural Tear: A Feared Complication of Lumbar Discectomy. Turk Neurosurg 26(2016): 918-921.
- Danish SF, Samdani A, Hanna A, et al. Experience with acellular human dura and bovine collagen matrix for duraplasty after posterior fossa decompression for Chiari malformations. J Neurosurg 104 (2006): 16-20.
- Hawk MW, Kim KD. Review of spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus 9 (2000): e5.
- Lu CH, Ho ST, Kong SS, et al. Intracranial subdural hematoma after unintended durotomy during spine surgery. Can J Anaesth 49 (2002): 100-102.
- Kee D Kim, Dinesh Ramanathan, Jason Highsmith, et al. DuraSeal Exact Is a Safe Adjunctive Treatment for Durotomy in Spine: Postapproval Study. Global Spine Journal 9 (2019): 272-278.
- Barber SM, Fridley JS, Konakondla S, et al. Cerebrospinal fluid leaks after spine tumor resection: avoidance, recognition and management. Ann Transl Med 7 (2019): 217.
- Zhao Fang, Yu-Tao Jia, Rong Tian, et al. Subfascial drainage for management of cerebrospinal fluid leakage after posterior spine surgery A prospective study based on Poiseuille's law. Chinese Journal of Traumatology 19 (2016): e35-e38.
- Jenkinson MD, Simpson C, Nicholas RS, et al. Outcome predictors and complications in the management of intradural spinal tumours. Eur Spine J 15 (2006): 203-210.
- Koechlin N O, Burkhardt J K, Scherer M, et al. Cerebrospinal fluid leaks after planned intradural spine surgery: a single-center analysis of 91 cases. Journal of Neurological Surgery. Part A: Central European Neurosurgery 74 (2012): 216-221.
- Zhao Fang, Rong Tian, Yu-Tao Jia, et al. Treatment of cerebrospinal fluid leak after spine surgery. Chinese Journal of Traumatology 20 (2017): e81-e83.
- Xinzhi Sun, Chuiguo Sun, Xiaoguang Liu, et al. The Frequency and Treatment of Dural Tears and Cerebrospinal Fluid Leakage in 266 Patients With Thoracic Myelopathy Caused by Ossification of the Ligamentum Flavum. SPINE 37 (2012): E702-E707.
