Dry Needling as a Treatment for Hallux Valgus – A Case Report
Article Information
Zilberberg O1*, Dr. Sheehan N MISCP MMedSE PhD2 , Dr. Sanocka D MD PhD3
1Member of ANMT (Association of Neuromuscular and Massage Therapies), Ireland
2Chairperson, Register of Orthopaedic and Soft Tissue Therapists of Ireland (ROSTI), Ireland
3Director of Private Mecidal Centre Our Clinic Sanocka, Ireland
*Corresponding Author: O Zilberberg, Member of ANMT (Association of Neuromuscular and Massage Therapies), Ireland
Received: 26 March 2023; Accepted: 03 April 2023; Published: 05 April 2023
Citation:
Zilberberg O, Sheehan N, Sanocka D. Dry Needling as a Treatment for Hallux Valgus – A -Case Report. Journal of Orthopedics and Sports Medicine. 5 (2023): 177-180.
Share at FacebookAbstract
Introduction: Hallux Valgus, commonly known as Bunions, is a condition in which the 1st proximal phalange deviates laterally while the 1st metatarsal deviates medially. The aim of this case report is to check the validity of Dry Needling (DN) as a treatment modality for patients presenting with this condition.
Materials and Methods: The Bristol Foot Score (BFS) was used to asses subjective changes with the client. Ultrasound (US) and X-Ray were used to determine structural changes pre and post treatment. Tests were performed before the initiation of the treatment, at the end of it, and 6 weeks after.
Case Presentation: Female client, 50 years of age, presenting with bunions since the age of 14. Previous options suggested to the client were fusion or shaving of the joint. Client had 23 DN sessions during this report. Results: On the BFS there was a 45.2% improvement in the score from baseline to 6 weeks after the last intervention. US and X-Ray comparison showed a decrease in the bunion angle going from severe (left) and moderate (right) to normal on both.
Conclusion: This report shows that DN can be considered as a feasible intervention for bunions.
Keywords
Dry Needling; Ultrasound guided Dry Needling; Hallux Valgus; Bunions
Article Details
Abbreviations: DN – Dry Needling; MTP – Metatarsophalangeal; BFS – Bristol Foot Score; US – Ultrasound; HVA – Hallux Valgus Angle
- Introduction
Hallux Valgus, commonly known as Bunions, is a condition estimated to affect 23% of population between the ages of 18 – 65, and 35.7% above the age of 65 [1]. In early stages, bunions begin with a deviation of the 1st proximal phalange laterally along with the 1st metatarsal medially. Overtime these deviations progress into a subluxation of the 1st Metatarsophalangeal (MTP) joint [2]. This condition is more prevalent in females when compared to males [1,2]. Due to the subluxation of the joint, inflammation may occur, causing further pain and swelling to the area [3,4].
Dry needling (DN) is being used to achieve various outcomes such as pain and muscle tension reduction, range of motion improvement and muscle strength and coordination improvement [5]. According to Cagnie et al. [5] DN increases blood flow to the treated area, allowing more oxygen to reach the surrounding tissues.
During the physiological process of wound healing, oxygen plays a main role. From the first stages of inflammation to the final stage tissue remodelling after scarring, oxygen is being used. Wound healing cells consume oxygen through the process of increased metabolism. However, due to the injury effecting the place, blood flow is decreased, and the combination of higher oxygen consumption with the decreased flow creates a hypoxic microenvironment that overtime can interfere with the process of healing [6]. Taking into consideration that wound healing requires oxygen, however that is also deprived of it, it could be concluded that DN an area which requires healing, or is within the stages of inflammation, will increase the blood flow, bring more oxygenated blood to the area and promote healing.
The aim of this case report is to check the validity and effectiveness of DN as a treatment for bunions, reducing the symptoms and discomfort. While some of the parameters examined are physical, measurable changes, the biggest hypothesised outcome would be subjective to the client and objective to the therapist.
- Materials and Methods
All needles used are Peace Classic Needles® sizes 0.16 × 13mm and 0.22 × 25mm (0.5” and 1” respectively). All needles were used once and disposed of thereafter.
The Bristol Foot Score (BFS) [7] was used on baseline, the last treatment and 6 weeks after the last treatment to check the lasting efficiency of the intervention from the client’s perspective.
Samsung SonoAce X8 Ultrasound Machine was used for the accuracy of the DN insertion into the 1st MTP joint cavity. The machine is capable of full spectrum imaging with a 17” high resolution monitor to allow precision work. The Ultrasound (US) was operated by a qualified physician.
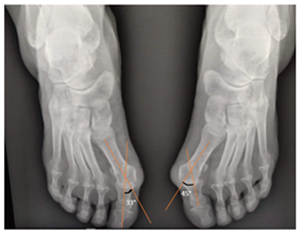
Initial bone positioning was done using an X-Ray as a referral given by the surgical consultants. The transition to US, for the progression check, was made in order to reduce client’s exposure to radiation, as it has been shown to be hazardous [8,9] and after confirming that US use can provide better insight into minor bone changes when compared with X-Ray [10].
Scans were made at the end of the treatment series, and 6 weeks after the last treatment to check for long term effects.
3. Case Presentation
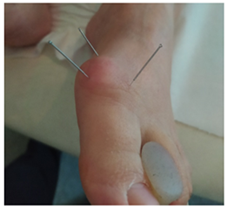
Our client is female, 50 years of age, presenting with bunions on both feet (Figure 1). The bunions have been present with her since approximately the age of 14, as the bunions are hereditary and were also present with the grandfather and aunt from the maternal side. The bunions have affected the quality of life for our client, and she has seen surgical consultants to decide the best approach for her. Among the suggestions given, a fusion surgery and a shaving procedure, both were refused at this point by the client.
Treatment for the bunions began in May of 2022. A total of 23 sessions has been administered. Appointments were aimed to take place once a week, however due to unforeseen circumstances, some weeks were skipped, and some weeks were done twice to maintain proximity between sessions. Due to the area being sensitive to touch, for the first 5 treatments, DN was applied in close proximity to the bunions, but not to the MTP joint itself. The aim of these treatments was to desensitize the area, and promote healing of the inflammation surrounding the joint.
Needles were inserted from the medial side pointing laterally and from superior pointing inferiorly in order to affect the most tissues possible from the surface of the bunion to the bone (Figure 2). Insertion was done within client’s level of tolerance. Needles were left in place for a period of 10 to 20 minutes, time varies according to client’s perceived reaction. Needles were taken out after client confirmed the needles sensation has subsided and they no longer feel the needles. From the 6th session, DN was done into the MTP joint cavity. Needles used at first were all 13mm aimed at the joint from superior and medial angles, however, with progression, needles were switched to 25mm at the 12th session in order to reach deeper into the joint cavity and get a deeper response.
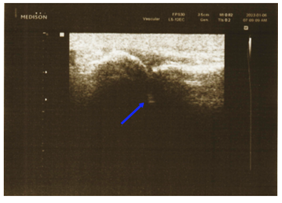
As mentioned, the Bunions were present with the client for roughly 36 years prior to treatment, so the inflammation to the area was built over years of no treatment. It was our hypothesis that aiming the DN at the MTP joint cavity would reduce inflammation inside the joint, promoting healing and structural changes. DN was done using US guidance (Figure 3) for precision insertion into the MTP joint cavity (Figure 4). Using US guided DN shown to promote better healing when compared with non US guided DN [11].
4. Results
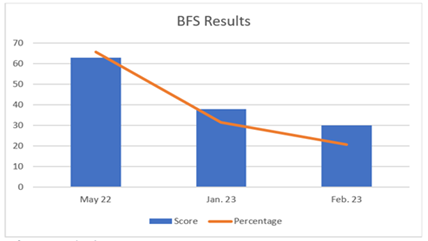
The BFS was filled out by our client on May 2022, at the baseline of the study. The score calculated was 63 out of 88 possible points. In the BFS, a lower score indicates good foot health and effect on the patient’s daily lifestyle, accordingly a higher score is an indicator of poor foot health and major negative effect on life. After intervention, on January 2023, another BFS was filled by the client, a score of 38 out of 88 was recorded. On the BFS taken 6 weeks post intervention a score of 30 was given. Setting 88 as a 100% and 15 as 0%, as that is the lowest score anyone can get from the BFS, the scores are 65.75%, 31.51% and 20.55% respectively (Figure 5). There was a 34.24% difference between January’s score and May’s score, pointing to a perceived improvement from the client’s side. The February’s score reflect that the change kept improving with no intervention, 45.2% improvement from baseline, and 10.96% from final intervention.
While examining and comparing the US of 6 weeks post treatment with the initial X-Ray, we measured the angle between the 1st metatarsal and 1st proximal phalange, also known as the Hallux Valgus Angle (HVA) on both US and X-Ray (Figure 6,7). We could see an angle of 13° in comparison with 45° on the left, and 7° compared with 33° on the right. This is a 32° (left) and 26° (right) difference between the pre-treatment and post treatment. The normal angle of HVA is between 5° – 15°, a mild Hallux Valgus is measured between 16° – 25°, moderate goes between 26° - 35°, and anything above 35° is considered severe [12]. The measurements show a change from severe on the left, and moderate on the right to normal angle on both.
5. Conclusion
This report has shown DN is a feasible therapeutic intervention to treat bunions. DN had both structural and subjective effects on the client, and held over a short period post treatment, with an improvement noted on a subjective level through the BFS.
Further research with a larger sample should be conducted in the future with a longer break period to check for longer term effects. Future research may need to include the effect of DN on the rest of the foot’s structure, including the angle between the bases of the 1st and 2nd Metatarsals, and the effect of the structure on the rest of the MTP joints.
6. Clinical Relevance
Many therapists come in close contact with a client suffering from bunions. This paper supports DN as a modality that can be used on a bunions, increasing client satisfaction and reducing the need for surgery.
Credit Authorship Contribution Statement:
- Zilberberg: Treatment design, Writing, Data curation. Dr. N. Sheehan: Supervision, Methodology, Writing – review and editing. D. Sanocka: Ultrasound operation and analysis.
References
- Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. Journal of Foot and Ankle Research 3 (2010).
- Hecht PJ, Lin TJ. Hallux Valgus. Medical Clinics of North America 98 (2014): 227-232.
- Kennedy JG, Collumbier JA. Bunions in Dancers. Clinics in Sports Medicine 27 (2008): 321-328.
- Ajis A, Koti M, Maffulli N. Tailor’s bunion: a review. The Journal of Foot and Ankle Surgery: Official Publication of the American College of Foot and Ankle Surgeons 44 (2005): 236-245.
- Cagnie B, Dewitte V, Barbe T, et al. Physiologic Effects of Dry Needling. Current Pain and Headache Reports 17 (2013).
- Schreml S, Szeimies RM, Prantl L, et al. Oxygen in acute and chronic wound healing. British Journal of Dermatology 163 (2010): 257-268.
- Barnett S, Campbell R, Harvey I. The Bristol Foot Score. Journal of the American Podiatric Medical Association 95 (2005): 264-272.
- Lin EC. Radiation Risk from Medical Imaging. Mayo Clinic Proceedings 85 (2010): 1142-1146.
- Pace N, Ricci L, Negrini S. A comparison approach to explain risks related to X-ray imaging for scoliosis, 2012 SOSORT award winner. Scoliosis 8 (2013): 11.
- Wakefield RJ, Gibbon WW, Conaghan PG, et al. The value of sonography in the detection of bone erosions in patients with rheumatoid arthritis: A comparison with conventional radiography. Arthritis and Rheumatism 43 (2000): 2762-2770.
- Pang JCY, Fu ASN, Lam SKH, et al. Ultrasound-guided dry needling versus traditional dry needling for patients with knee osteoarthritis: A double-blind randomized controlled trial. PLOS ONE 17 (2022): e0274990.
- Gentili A, Masih S, Yao L, et al. Foot axes and angles. The British Journal of Radiology 69 (1996): 968-974.