Double-Shelled Brace to Correct Spinal Deformity in Non-Ambulatory Patients with Cerebral Palsy A STROBE-Compliant Study
Article Information
Adrian Bosshard1, Maden Nadarajalingam1, Sandra Keller1, Reinald Brunner2,3, Carlo Camathias2,3, Erich Rutz2,3,4*
1ORTHO-TEAM Bern AG, Bern, Switzerland
2University Children’s Hospital, UKBB, Basel, Switzerland
3University of Basel, Basel, Switzerland
4Murdoch Children’s Research Institute, The Royal Children’s Hospital Melbourne, Parkville, Victoria, Australia
*Corresponding Author: Erich Rutz, Department of Pediatric Orthopedics, University Children’s Hospital Basel, UKBB, PO Box, CH-4031 Basel, Switzerland
Received: 15 August 2019; Accepted: 30 August 2019; Published: 05 September 2019
Citation:
Adrian Bosshard, Maden Nadarajalingam, Sandra Keller, Reinald Brunner, Carlo Camathias, Erich Rutz. Double-Shelled Brace to Correct Spinal Deformity in Non-Ambulatory Patients with Cerebral Palsy-A STROBE-Compliant Study. Journal of Pediatrics, Perinatology and Child Health 3 (2019): 152-162.
Share at FacebookAbstract
Introduction: The generally accepted incidence of scoliosis in cerebral palsy (CP) is 20% to 25% and is directly related to the Gross Motor Function Classification System (GMFCS) level. One treatment option for neurogenic scoliosis is a double-shelled brace (DSB). The aim of this study was to investigate the degree of correction achieved when using three different replica techniques.
Materials and Methods: We included a consecutive series of 25 CP patients (8 boys, 15 girls) in this retrospective study. Mean age was 13.0 years (range: 4.0 to 20.0 years). All participants were non-ambulatory (GMFCS levels IV and V). The degree of immediate correction was expressed in percent of the lumbar and thoracic COBB angles.
Results: At the level of the lumbar spine, we found a mean (± SD) curve of 45.7° (19.2°). Mean correction with the DSB was 20.9° (13.1°; p<0.05). This represents an improvement of 49.9% At the level of the thoracic spine, we determined a mean curve of 40.5° (17.8°). In all the cases, we measured the immediate correction. Mean correction with the DSB was 13.8° (10.3°; p<0.05). This represents an improvement of 33.1%. All three replica techniques achieved a statistically significant correction (p<0.05) of the COBB angles at both levels.
Conclusions: Double-shelled bracing provides an excellent immediate correction of neurogenic scoliosis in cerebral palsy. Further studies are required to investigate long-term outcomes.
Keywords
Spinal Deformity, Double-Shelled Brace, Cerebral Palsy
Spinal Deformity articles, Double-Shelled Brace articles, Cerebral Palsy articles
Article Details
1. Introduction
The incidence of scoliosis in cerebral palsy (CP) varies greatly. Recent studies reported rates ranging from 6% to almost 100% [1-3]. The generally accepted incidence in the overall CP population is 20% to 25% [3]. The incidence is lowest in patients with athetoid type of CP (6%-50%) and highest in those with spastic CP (up to 70%) [4]. In patients with subluxated or dislocated hips (an indicator of disease severity), Madigan and Wallace observed an incidence of scoliosis of approximately 75% [4]. Pelvic obliquity is considered the key measure thus requiring more attention [1-3]. The incidence of scoliosis is also directly related to the Gross Motor Function Classification System (GMFCS) [5] level. Untreated scoliosis in patients with CP is associated with progression, and factors implicated in deterioration include the type of involvement (quadriplegia), poor functional status (non-ambulatory, GMFCS levels IV and V), and curve location (thoracolumbar) [1-3, 6]. The cause of scoliosis in CP is not entirely clear but is thought to be a combination of muscle weakness, truncal imbalance, and asymmetric tone in paraspinous and intercostal muscles [3].
Saito et al. described the risk factors for progression of scoliosis in spastic CP as follows: spinal curve of 40° COBB angle before the age of 15 years, total body involvement, bedriddenness, and presence of thoracolumbar curve [1]. Patients with these risk factors might benefit from early surgical intervention to prevent severe scoliosis. It is, however, known that bone growth is reduced under pressure and increased under tension, which may lead to rapid progression in severely affected patients (GMFCS levels IV and V). According to our experience, scoliosis mainly results from inadequate gravity control, which typically leads to lateral flexion of the thorax over the relative mobile spine, thus resulting in a thoracolumbar curve. Non-operative treatment options consist of observation and bracing but also include seating modifications and pharmacological management. There are two methods to provide external support to the spine in the presence of neuromuscular scoliosis: i.e. customized seating arrangements and braces (e.g. double-shelled brace; DSB) [2]. Most patients suffering from neuromuscular disorders present with poor balance control and dynamic instability of the trunk. At an early stage, the patient presents with dynamic instability of the trunk only, and this can be easily observed by asking for “hands up” while sitting.
The goals of any intervention are to maintain comfortable sitting and to allow functional use of the upper extremities. There is some evidence that the use of braces may slow curve progression in quadriplegic CP [7], but it is unclear whether spinal bracing reduces the need for surgery [2]. During growth, however, spinal bracing reduces the radius of the curve and slows the progression to severe curves [7]. Nevertheless, it is unclear whether bracing is able to stop progression [1-3, 7-11]. Thus, spinal bracing in children with CP is a well-described and established method of conservative management [7, 9, 10, 12-17]. Although botulinum toxin A is increasingly used to treat limb spasticity in patients suffering from CP, there is little evidence of its use in treating scoliosis [3].
The aim of this study was to assess the effectiveness of DSB in the treatment of neurogenic scoliosis with respect to the following:
- Immediate correction of the lumbar and thoracic COBB angle,
- Influence of three different replica techniques, namely A: print supine, B: print lying in lateral position, C: computer aided design (CAD) technique supine.
In addition, we recorded the average time of DSB use per day and local complications, such as pressure sores.
2. Materials and Methods
This study was conducted according to local ethics requirements (KEK 2015; Berne, Switzerland) and the Declaration of Helsinki. Inclusion criteria were confirmed CP diagnosis, non-ambulatory status (GMFCS level IV or V), lumbar or thoracic COBB angles of more than 20° (or severe trunk instability), and age of 4 to 20 years. Exclusion criteria were painful dislocation of the hip, GMFCS levels I to III, or previous spine surgery.
2.1 Study cohort
A consecutive series of 25 patients with CP was included in this retrospective investigation. Overall, we recruited 8 male and 15 female patients. The mean age was 13.0 years (range: 4.0 to 20.0 years). Overall, 12 patients were classified as GMFCS level IV function and 13 patients as GMFCS level V function. Table 1 provides the demographics, such as sex, age, and type of scoliosis (12 patients with lumbar curve, 5 patients with thoracic curve, and 8 patients with S shaped curve). All patients were hypotonic at the level of the trunk but suffered from spasticity at the level of the lower and upper extremities.
|
Patient no |
Sex |
Age |
Type of scoliosis |
Replica technique |
|
1 |
f |
14 |
lumbar |
C |
|
2 |
f |
12 |
lumbar |
C |
|
3 |
m |
17 |
lumbar |
A |
|
4 |
m |
14 |
lumbar |
B |
|
5 |
f |
10 |
lumbar |
B |
|
6 |
f |
8 |
lumbar |
B |
|
7 |
f |
14 |
lumbar |
A |
|
8 |
f |
14 |
thoracic |
A |
|
9 |
m |
15 |
lumbar & thoracic |
A |
|
10 |
m |
13 |
thoracic |
A |
|
11 |
f |
9 |
lumbar & thoracic |
C |
|
12 |
f |
17 |
thoracic |
B |
|
13 |
f |
10 |
lumbar |
B |
|
14 |
f |
4 |
lumbar & thoracic |
C |
|
15 |
f |
9 |
lumbar & thoracic |
B |
|
16 |
f |
17 |
lumbar & thoracic |
A |
|
17 |
f |
18 |
lumbar & thoracic |
A |
|
18 |
f |
11 |
lumbar & thoracic |
B |
|
19 |
m |
16 |
lumbar |
C |
|
20 |
m |
11 |
lumbar |
B |
|
21 |
f |
14 |
lumbar & thoracic |
A |
|
22 |
f |
20 |
thoracic |
A |
|
23 |
f |
13 |
lumbar |
B |
|
24 |
m |
13 |
thoracic |
B |
|
25 |
m |
12 |
lumbar |
B |
f=female; m=male; replica technique A=print supine, B=print lying in lateral position on a roll, C=CAD technique supine
Table 1: patient’s demographics.
2.2 Radiologic findings
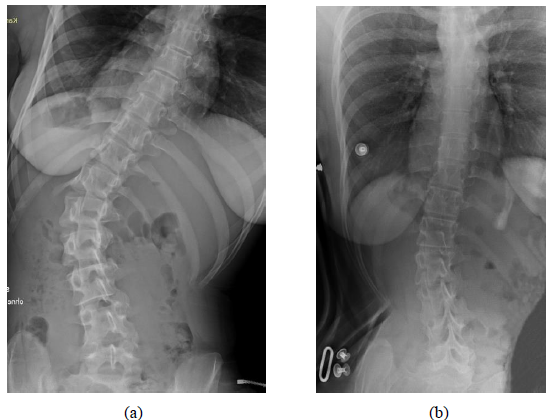
Standardized antero-posterior (ap) radiographs were analyzed retrospectively. These pictures were recorded in a sitting position in all patients. In three patients, we obtained plain X-ray images in the standing position. Radiographs must not be obtained in the lying position because the maximum of the curve is not visible in this position due to absent gravity force. The apex as well as lumbar and thoracic COBB angles were calculated from the ap radiographs. All angles were measured using Centricity DICOM Viewer V3.1. At the same hospital appointment, two radiographs were obtained: We obtained the first radiograph (T1) using the brace (DSB), and after 5 min (T0), we obtained a second X-ray without application of the brace. This was possible only for patients with good and correct adaption of the DSB. For other patients, the time period between T1 and T0 was no longer than 3 months due to the need of adaptations of the DSB by the orthotechnician. The degree of correction of the COBB angle at the levels of the lumbar and thoracic spine was expressed as percent of the measurement without the brace at T0.
2.3 Double-shelled brace and replica technique
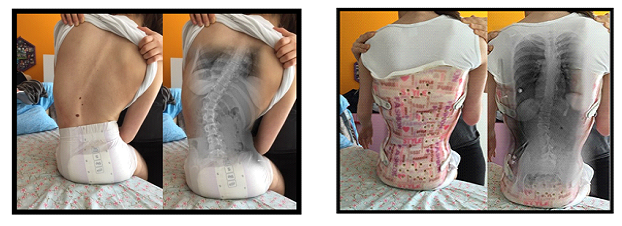
A DSB was used in all cases as described by Rutz et al. in 2013 [19]. This is a custom-made brace (Figure 1) that is easy to handle. The parents or caregivers were advised to apply the DSB to the affected patient for 6 to 8 h per day, in positions allowing gravity to influence the curvatures of the spine, such as the sitting or standing positions, but not during sleeping and lying.
We used the following three replica techniques:
- A: Print supine: During this procedure, the correction was provided manually. Two experienced orthotechnicians performed this print when the patient was in a lying position (supine). Hips were flexed at 70°.
- B: Print lying in lateral position: During this procedure, the patients was lying on the convex side of the curve. Two experienced orthotechnicians performed this print. Hips were flexed at 70°. Figure 2 illustrates this position (head on the right side).
- C: CAD technique supine: For this procedure, we employed CAD software (Canfit Dessin V14.0 and Scan Gogh, VORUM Research Canada). Two experienced orthotechnicians performed this print when the patient was in a supine lying position under traction. The “models” were imported in a library by using the VORUM Research Canada software. Technique A was used in 9 (36%) patients, while techniques B and C were applied in 11 (44%) in 5 (20%) patients, respectively.
2.4 Clinical data
Parents and care-givers reported
- the duration of DSB use per day (in hours) during sitting or standing positions, and
- any problems associated with the use of DSB, such as skin problems or pressure soars.
2.5 Statistics
For the statistical analysis of the data, we used JMPâ Version 10.0.0 (SAS Institute, Cary, NC). All data were analyzed for normal distribution by using Shapiro-Wilk-Test. A paired t-test was used to compare the data obtained in the presence and absence of DSB. A one-way ANOVA was performed to detect differences between the replica techniques A, B, and C. In cases of statistical significance, a post-hoc Tukey test was used. The level of significance was set at α=0.05. A priori power calculation was used to estimate the required sample size. Previously reported data [19] on the conservative treatment of spinal deformity were used to calculate the corresponding effect size for our population (effect size=1.04). A priori power analysis with α=0.05 and β=0.80 indicated a minimum sample size of 10.
3. Results
3.1 Study cohort
All included patients were able to participate in our study. In patient No. 9, the lumbar curve deteriorated from an initial COBB angle of 50° to 60° within a time period of 3 months. Patient No. 15 exhibited a lumbar curve of 15° but additionally suffered from severe trunk instability. For this reason, this patient was included in the study.
3.2 Radiographic findings
Overall, 40 of 50 (80%) of the radiographs were obtained on the same day (T1 and T0). Ten radiographs (20%; (n= 5 patients), for T0 and T1 were not obtained on the same day but were recorded within a time period of less than 3 months. During this time period, adaptations of the DSB were necessary. All DSBs were checked clinically 4, 8, and 12 weeks after the initial delivery by the orthotechnicians. At the level of the lumbar spine, we measured a mean (± SD) curve of 45.7° (19.2°). Mean correction when using DSB was 20.9° (13.1°; p< 0.05) within a time period of 3 months. This represents an improvement of 49.9%. At the level of the thoracic spine, we calculated a mean curve of 40.5° (17.8°). Mean correction achieved by using DSB was 13.8° (10.3°; p< 0.05). This represents an improvement of 33.1%. Tables 2a and 2b list the corrections for all 25 patients at the position of the lumbar spine (Table 2a) and thoracic spine (Table 2b).
|
Patient |
RX 1 |
RX 1 |
RX 2 |
RX 2 |
Correction Cobb angle lumbar [°] |
Correction |
|
1 |
36 |
LW 1 |
20 |
LW 2 |
16 |
44.4 |
|
2 |
79 |
LW 3 |
45 |
LW 3 |
34 |
43.0 |
|
3 |
52 |
LW 2 |
20 |
LW 2 |
32 |
61.5 |
|
4 |
33 |
LW 2 |
20 |
LW 2 |
13 |
39.4 |
|
5 |
40 |
LW 2 |
20 |
LW 2 |
20 |
50.0 |
|
6 |
40 |
LW 3 |
9 |
LW 2 |
31 |
77.5 |
|
7 |
20 |
LW 2 |
7 |
LW 2 |
13 |
65.0 |
|
9 |
50 |
LW 2 |
60 |
LW 2 |
-10 |
-20.0 |
|
11 |
42 |
LW 2 |
0 |
- |
42 |
100.0 |
|
13 |
15 |
LW 1 |
0 |
LW 1 |
15 |
100.0 |
|
14 |
24 |
LW 2 |
10 |
LW 1 |
14 |
58.3 |
|
15 |
46 |
LW 2 |
27 |
LW 2 |
19 |
41.3 |
|
16 |
60 |
LW 2 |
45 |
LW 2 |
15 |
25.0 |
|
17 |
56 |
LW 1 |
33 |
LW 1 |
23 |
41.1 |
|
18 |
33 |
LW 2 |
22 |
LW 1 |
11 |
33.3 |
|
19 |
50 |
LW 1 |
45 |
LW 1 |
5 |
10.0 |
|
20 |
72 |
LW 2 |
27 |
LW 2 |
45 |
62.5 |
|
21 |
88 |
LW 2 |
61 |
LW 2 |
27 |
30.7 |
|
23 |
52 |
LW 1 |
17 |
LW 1 |
35 |
67.3 |
|
25 |
25 |
LW 3 |
8 |
LW 3 |
17 |
68.0 |
RX=x-ray; LWS=lumbar spine; LW=lumbar vertebra/The correction value of patient no 9 of -10° means a deterioration of the scoliosis
Table 2: (a) Lumbar results.
|
Patient no |
RX 2 |
RX 1 |
RX 2 |
RX 2 |
Correction |
Correction |
|
8 |
61 |
BW 11 |
37 |
BW 8 |
24 |
39.3 |
|
9 |
34 |
BW 7 |
34 |
BW 8 |
0 |
0.0 |
|
10 |
23 |
BW 10 |
23 |
BW 9 |
0 |
0.0 |
|
11 |
35 |
BW 8 |
14 |
BW 5 |
21 |
60.0 |
|
12 |
70 |
BW 8 |
40 |
BW 9 |
30 |
42.9 |
|
14 |
18 |
BW 8 |
10 |
BW 7 |
8 |
44.4 |
|
15 |
21 |
BW 9 |
13 |
BW 8 |
8 |
38.1 |
|
16 |
55 |
BW 9 |
40 |
BW 9 |
15 |
27.3 |
|
17 |
29 |
BW 7 |
21 |
BW 7 |
8 |
27.6 |
|
18 |
21 |
BW 8 |
12 |
BW 8 |
9 |
42.9 |
|
21 |
54 |
BW 8 |
40 |
BW 8 |
14 |
25.9 |
|
22 |
56 |
BW 10 |
46 |
BW 9 |
10 |
17.9 |
|
24 |
50 |
BW 8 |
18 |
BW 8 |
32 |
64.0 |
RX=x-ray; BWS=thoracic spine; BW=thoracic vertebra
Table 2: (b) Thoracic results.
3.3 Effects of the replica techniques on the lumbar spine
Replica technique A (n=9 patients) resulted in a median correction rate of 33.9% (range: -20% to 61.5%). This corresponded to a median angle correction of 16.7° (range: -10° to 32°) at the level of the lumbar spine. Replica technique B (n=11 patients) resulted in a median correction rate of 59.9% (range: 33.3 to 62.5%). This corresponded to a median angle correction of 22.9° (range: 11° to 45°) at the level of the lumbar spine. Replica technique C (n=5 patients) resulted in a median correction rate of 51.2% (range: 10 to 100%). This corresponded to a (median angle correction of 22.2° (range: 5 to 42°) at the level of the lumbar spine. All replica techniques achieved a statistically significant correction of scoliosis (p<0.05), but replica technique B provided the best correction at the level of the lumbar spine (59.9%).
3.4 Effects of the replica techniques on the thoracic spine
Replica technique A (n=9 patients) resulted in a median correction rate of 19.7% (range: 0 to 24%). This corresponded to a median angle correction of 10.1° (range: 0 to 24°) at the level of the thoracic spine. Replica technique B (n=11 patients) resulted in a median correction rate of 47.0% (range: 38.1 to 64.0%). This corresponded to a median angle correction of 19.8° (range: 8 to 32°) at the level of the thoracic spine. Replica technique C (n=5 patients) provided a median correction rate of 52.2% (range: 44.4 to 60.0%). This corresponded to a median angle correction of 14.5° (range: 8 to 21°) at the level of the thoracic spine. All replica techniques achieved a statistically significant correction (p<0.05), but technique C provided the best correction at the level of the thoracic spine (51.2%; Tables 3a and 3b).
|
Correction lumbar |
Replica technique A |
Replica technique B |
Replica technique C |
|
mean [°] |
16.7 |
22.9 |
22.2 |
|
standard deriation [°] |
14.9 |
11.5 |
15.3 |
|
mean [%] |
33.9 |
59.9 |
51.2 |
|
standard deriation [%] |
30.9 |
21.3 |
32.6 |
Replica technique A=print supine, B=print lying in lateral position on a roll, C=CAD technique supine
Table 3: (a) Correction lumbar dependent on replica technique.
|
Correction thoracic |
Replica technique A |
Replica technique B |
Replica technique C |
|
mean [°] |
10.1 |
19.8 |
14.5 |
|
standard deriation [°] |
8.6 |
13.0 |
9.2 |
|
mean [%] |
19.7 |
47.0 |
52.2 |
|
standard deriation [%] |
14.9 |
11.6 |
11 |
Replica technique A=print supine, B=print lying in lateral position on a roll, C=CAD technique supine
Table 3: (b) Correction thoracic dependent on replica technique.
3.5 Clinical findings
Parents or caregivers reported a median daily use of DSB of 6.7 h (range 6 to 10 h). Temporary skin redness was noted in 10 patients (40%). None of the patients experienced deep pressure sores.
3.6 Clinical case
Figures 3 and 4 show the clinical and radiologic findings for an 18-year old woman (case 17). Figure 3 represents the clinical photographs with and without the DSB. Figure 4 shows the radiographs of this patient without (a) and with (b) the DSB.
4. Discussion
To our knowledge, this is the first study investigating the degree of angle correction achieved with three different replica techniques in neurogenic scoliosis in patients with CP. In our retrospective study involving 25 patients treated with DSB due to neurogenic scoliosis, we determined a 50% correction of the lumbar spinal deformity and a 30% correction of the thoracic deformity. All replica techniques obtained a statistically significant correction of the COBB angles. Technique B provided the best correction at the level of the lumbar spine (59.9%), and technique C achieved the best correction at the level of the thoracic spine (51.2%). Saito et al. described the risk factors for progression of scoliosis in spastic CP and recommend early surgical intervention to prevent progression to severe scoliosis [1]. This kind of surgery is demanding and associated with a high rate of complications. Therefore, early bracing for correction of neurogenic scoliosis in children with CP is a rewarding treatment option [7, 9, 10, 12-17].
Terjesen et al. reported the results of treatment with spinal orthoses in 86 patients with spastic quadriplegic CP [7]. Their scoliotic deformities were treated with custom-molded, polypropylene thoraco-lumbar-sacral orthoses. The mean initial COBB angle was 68°, and mean correction in orthosis was 25°. In our study, the mean degree of initial deformity was lower, but the extent of correction was similar. In the study of Terjesen et al., long-term follow-up of 6.3 years was obtained. The authors reported a mean progression rate of 4.2° per year. However, spinal orthosis bracing does not delay the rate of curve progression.
5. Study Limitations
There were several limitations of our study. We included a small number of young CP patients, and long-term results are missing since we investigated the immediate (short-term) effects only. Moreover, the influence of pelvic obliquity and hip pathology was not taken into account. For the reporting of the time of daily DSB use, we refrained from using skin sensors and relied on parent or caregiver reports. The type of replica technique used did not seem to influence the short-term outcome of spinal bracing. Clinical experience and manual work of the orthotechnicians appear to be more important. We postulate that optimal correction of the COBB angles at the level of lumbar and thoracic spine should be achieved from the beginning of bracing therapy, especially in young children with neurogenic scoliosis using a DSB.
6. Conclusions
Use of DSB provided excellent immediate correction of neurogenic scoliosis in our cohort of young CP patients. Both the lumbar spinal and thoracic deformities were markedly corrected, and all three replica techniques achieved statistically significant corrections of the COBB angles. Further studies are required to investigate long-term outcomes of these techniques.
References
- Saito N, Ebara S, Ohotsuka K, et al. Natural history of scoliosis in spastic cerebral palsy. Lancet 351 (1998): 1687-1692.
- Koop SE. Scoliosis in cerebral palsy. Dev Med Child Neurol 4 (2009): 92-98.
- Imrie MN, Yaszay B. Management of spinal deformity in cerebral palsy. Orthop Clin North Am 4 (2010): 531-547.
- Madigan RR, Wallace SL. Scoliosis in the institutionalized cerebral palsy population. Spine (Phila Pa 1976) 6 (1981): 583-590.
- Palisano R, Rosenbaum P, Walter S, et al. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 4 (1997): 214-223.
- Galasko CS. Progression of scoliosis. J Pediatr Orthop 17 (1997): 407.
- Terjesen T, Lange JE, Steen H. Treatment of scoliosis with spinal bracing in quadriplegic cerebral palsy. Dev Med Child Neurol 42 (2000): 448-454.
- Kotwicki T, Jozwiak M. Conservative management of neuromuscular scoliosis: personal experience and review of literature. Disabil Rehabil 30 (2008): 792-798.
- Winter RB, Carlson JM. Modern orthotics for spinal deformities. Clin Orthop Relat Res 126 (1977): 74-86.
- James WV. Spinal bracing in children with atonic cerebral palsy. Ulster Med J 44 (1975): 53-55.
- Zadek RE. Orthopedic management of the child and multiple handicaps. Pediatr Clin North Am 20 (1973): 177-185.
- Baumann JU. Conservative therapy of scoliosis in cerebral palsy. Z Orthop Ihre Grenzgeb 114 (1976): 496-498.
- James WV. Spinal bracing for children with atonic cerebral palsy. Prosthet Orthot Int 1 (1977): 105-106.
- Brunner R, Gebhard F. Neurogenic spinal deformities - Conservative and surgical treatment of spinal deformities. Orthopade 31 (2002): 51-57.
- Nuzzo RM. Dynamic bracing: elastics for patients with cerebral palsy, muscular dystrophy and myelodysplasia. Clin Orthop Relat Res 148 (1980): 263-273.
- Bunnell WP, MacEwen GD. Non-operative treatment of scoliosis in cerebral palsy: preliminary report on the use of a plastic jacket. Dev Med Child Neurol 19 (1977): 45-49.
- Thomson JD, Banta JV. Scoliosis in cerebral palsy: an overview and recent results. J Pediatr Orthop B 10 (2001): 6-9.
- Rutz E, Brunner R. Lumbal short corset for treatment of neuromuscular scoliosis. Medizinisch-Orthopädische Technik 3 (2008): 71-74.
- Rutz E, Brunner R. Management of spinal deformity in cerebral palsy: conservative treatment. J Child Orthop 7 (2013): 415-418.