Diagnosis and Surgical Management with Immediate Breast Reconstruction of atypical Borderline Phyllodes tumor: Case Report
Article Information
Alejandro Flores Uribe*, Jorge Alberto González Arévalo, Diego Bolaños Maya, Eduardo Chávez Ornelas, Roberto Martínez Mejorada
General Surgery Department, Christus Muguerza Alta Especialidad Hospital, Monterrey, Nuevo León, México.
*Corresponding Author: Alejandro Flores Uribe, Universidad de Monterrey (UDEM), Escuela de Medicina, Especialidades Médicas. Av. Ignacio Morones Prieto 4500, Jesús M. Garza, San Pedro Garza García, N.L. Zip Code 66238.
Received: 09 November 2022; Accepted: 16 November 2022; Published: 25 November 2022
Citation: Alejandro Flores Uribe, Jorge Alberto González Arévalo, Diego Bolaños Maya, Eduardo Chávez Ornelas, Roberto Martínez Mejorada. Diagnosis and Surgical Management with Immediate Breast Reconstruction of atypical Borderline Phyllodes tumor: Case Report. Journal of Surgery and Research 5 (2022): 593-598.
Share at FacebookAbstract
We present the case of a phyllodes breast tumor of borderline type, one of the rarest in the breast cancer literature. She is a 30-year-old female who is admitted to the emergency room due to a stabbing pain in the left breast and changes in coloration at nipple level, accompanied by a progressive volume increase. In general surgery consultation, the diagnosis is confirmed by simple thoracoabdominal tomography and biopsy with a tru-cut core needle. The mass was resected by surgery, which is sent to pathology reconfirming the diagnosis, ruling out a fibroadenoma or nested metastases. The patient's outcome and prognosis was positive. The important lessons of this case is to share the diagnosis and management carried out, to contribute to the literature and that other authors benefit from it as information or even as a management replica. It also provides an interesting value in terms of epidemiology in the context of northern Mexico.
Keywords
Phyllodes, Borderline, Management, Diagnosis, Atypical
Phyllodes articles; Borderline articles; Management articles; Diagnosis articles; Atypical articles
Phyllodes articles Phyllodes Research articles Phyllodes review articles Phyllodes PubMed articles Phyllodes PubMed Central articles Phyllodes 2023 articles Phyllodes 2024 articles Phyllodes Scopus articles Phyllodes impact factor journals Phyllodes Scopus journals Phyllodes PubMed journals Phyllodes medical journals Phyllodes free journals Phyllodes best journals Phyllodes top journals Phyllodes free medical journals Phyllodes famous journals Phyllodes Google Scholar indexed journals Borderline articles Borderline Research articles Borderline review articles Borderline PubMed articles Borderline PubMed Central articles Borderline 2023 articles Borderline 2024 articles Borderline Scopus articles Borderline impact factor journals Borderline Scopus journals Borderline PubMed journals Borderline medical journals Borderline free journals Borderline best journals Borderline top journals Borderline free medical journals Borderline famous journals Borderline Google Scholar indexed journals Management articles Management Research articles Management review articles Management PubMed articles Management PubMed Central articles Management 2023 articles Management 2024 articles Management Scopus articles Management impact factor journals Management Scopus journals Management PubMed journals Management medical journals Management free journals Management best journals Management top journals Management free medical journals Management famous journals Management Google Scholar indexed journals Diagnosis articles Diagnosis Research articles Diagnosis review articles Diagnosis PubMed articles Diagnosis PubMed Central articles Diagnosis 2023 articles Diagnosis 2024 articles Diagnosis Scopus articles Diagnosis impact factor journals Diagnosis Scopus journals Diagnosis PubMed journals Diagnosis medical journals Diagnosis free journals Diagnosis best journals Diagnosis top journals Diagnosis free medical journals Diagnosis famous journals Diagnosis Google Scholar indexed journals fibroadenoma articles fibroadenoma Research articles fibroadenoma review articles fibroadenoma PubMed articles fibroadenoma PubMed Central articles fibroadenoma 2023 articles fibroadenoma 2024 articles fibroadenoma Scopus articles fibroadenoma impact factor journals fibroadenoma Scopus journals fibroadenoma PubMed journals fibroadenoma medical journals fibroadenoma free journals fibroadenoma best journals fibroadenoma top journals fibroadenoma free medical journals fibroadenoma famous journals fibroadenoma Google Scholar indexed journals general surgery articles general surgery Research articles general surgery review articles general surgery PubMed articles general surgery PubMed Central articles general surgery 2023 articles general surgery 2024 articles general surgery Scopus articles general surgery impact factor journals general surgery Scopus journals general surgery PubMed journals general surgery medical journals general surgery free journals general surgery best journals general surgery top journals general surgery free medical journals general surgery famous journals general surgery Google Scholar indexed journals thoracoabdominal articles thoracoabdominal Research articles thoracoabdominal review articles thoracoabdominal PubMed articles thoracoabdominal PubMed Central articles thoracoabdominal 2023 articles thoracoabdominal 2024 articles thoracoabdominal Scopus articles thoracoabdominal impact factor journals thoracoabdominal Scopus journals thoracoabdominal PubMed journals thoracoabdominal medical journals thoracoabdominal free journals thoracoabdominal best journals thoracoabdominal top journals thoracoabdominal free medical journals thoracoabdominal famous journals thoracoabdominal Google Scholar indexed journals metastases articles metastases Research articles metastases review articles metastases PubMed articles metastases PubMed Central articles metastases 2023 articles metastases 2024 articles metastases Scopus articles metastases impact factor journals metastases Scopus journals metastases PubMed journals metastases medical journals metastases free journals metastases best journals metastases top journals metastases free medical journals metastases famous journals metastases Google Scholar indexed journals nipple level articles nipple level Research articles nipple level review articles nipple level PubMed articles nipple level PubMed Central articles nipple level 2023 articles nipple level 2024 articles nipple level Scopus articles nipple level impact factor journals nipple level Scopus journals nipple level PubMed journals nipple level medical journals nipple level free journals nipple level best journals nipple level top journals nipple level free medical journals nipple level famous journals nipple level Google Scholar indexed journalsArticle Details
Introduction
Phyllodes tumor of the breast is a rare fibroepithelial neoplasm, encompassing 0.3% to 1% of breast tumors. These tumors are classified by the World Health Organization (WHO) as benign, borderline, and malignant [1]. They predominantly occur in women in middle adulthood (40 to 50 years), occurring about 15 to 20 years after fibroadenomas [2]. These tumors occur mostly in women, however there are some cases reported in males [3]. This case is rare not only because of the histopathological and epidemiological nature in breast cancer, since the Borderline type tumor only occurs in 12 to 26% of cases of all phyllodes tumors, in addition to being the least investigated type of the three [1], if not also its rarity is complemented in the painful and stabbing clinic, being common the painless unilateral masses that stretch the skin and distend the superficial veins [4], in our case a dermal stretch was observed, but only color changes were observed in the nipple. We also consider this case of importance because of the little or no information about these tumors in northern Mexico (and in Latin America in general).
Case Presentation
We present the case of a 30-year-old female patient, Mexican, professional, married with economic independence and a BMI of 24.7. Reports having no relevant medical history or important allergies, began 3 months prior to admission to the emergency department to present stabbing pain, located in the left breast, without the presence of pain migration (for which he refers to having taken acetaminophen 500 mg every 8 hours occasionally from the onset of pain), accompanied by a progressive increase in volume and changes in coloration at the nipple level. It has a father with type 2 diabetes mellitus and a mother without chronic degenerative diseases, the patient reports consumption of alcohol and occasional tobacco. She was referred to general surgery which after her assessment, requested a biopsy with a core needle (Tru-cut), with histopathological report of a Phyllodes tumor type Borderline, and a simple thoracoabdominal CT scan that reported a tumor in the left breast with dimensions of 15 x 13 x 18 cm, with volume of 2020 cc, of lobed contours with extension to skin and left pectoralis major muscle, with the presence of axillary nodes with suspicious morphology at the central level (Figure 1), with this a diagnosis of Borderline Phyllodes tumor in the left breast was made. After this, he came electively for his definitive surgical management. Upon arrival, during the physical examination, the left breast was assessed with an increase in volume of 15 x 13 cm, presence of ulcer at the level of the nipple with the presence of changes in coloration, right breast and rest of the examination without alterations present (Figure 2). Laboratories show a hemoglobin figure of 12.7 (14-18 g/dl), mean corpuscular volume (MCV) of 86.4 (80-94 fL), mean corpuscular hemoglobin (MCH) of 30.2 (28 - 32 pg), leukocytes of 8,120 (4,500-11,500) with neutrophils of 56.5% (50-70%), eosinophils of 4.8% (1-3%), other studies within normal parameters. It was scheduled for left total mastectomy with reconstruction with broad dorsal musculocutaneous flap. The procedure was performed by an external doctor with five years of experience as a general surgeon as well as the accompaniment of a plastic surgeon with 10 years experience, the procedure was performed in a high specialty hospital in northern Mexico. There were no changes in planning or management in the preoperative and transoperative period. A preoperative scheme was initiated with cephalothin (1 g IV every 12 hours), acetaminophen (1 g IV every 8 hours), ketorolac (30 mg IV every 8 hours), there was no pre-existing disease type preparation that will indicate a special type of preparation for this procedure. It was performed with balanced general anesthesia and epidural block- An approach that began with the patient in a supine position, performing a wash with chlorhexidine at the incision site, the approach is performed with wide margins of 1 cm of tumor in the left breast, subcutaneous cell tissue was dissected until reaching the pectoralis major muscle and costal grill which were dried en bloc along with the tumor (Figure 3), the piece was resected which weighed a total of 2,500 grams and was sent to pathology to definitive, after this two left palpable axillary nodes are resected that were also sent to pathology with resected piece, finally hemostasis was performed without acute complications. In a second surgical time, the patient was accommodated in the right lateral position, the vascular pedicle of the thoracodorsal artery/vein was located by Doppler ultrasound and then the marking of the same was completed, an incision was made on the left dorsal region with a size of 15 x 20 cm, it was dissected until locating the broad dorsal muscle which respected both the vascular flap pedicle and the perforating arteries of the remaining muscle, once its complete dissection was finished, it was rotated to place it on a post-mastectomy wound and covered in its entirety (Figure 4), 2 continuous suction drains of closed type were placed in the 2 wounds which were fixed with prolene 3-0, and both wounds were closed by planes with vicryl 2-0 in subcutaneous cellular tissue and prolene 3-0 skin, the procedure was completed without any complications. In the transoperative period, the histopathology report confirmed the diagnosis of Borderline-type Phyllodes tumor in the left breast with negative nodes for regional metastasis (Figure 5). In the postoperative period, cephalothin (1 g IV every 12 hours), ketorolac (30 mg IV every 8 hours), acetaminophen (1 g IV every 8 hours) and omeprazole (40 mg IV every 24 hours) were used. One of the difficulties at the time of making the diagnosis was the presence of a non-specific and insidious clinic, coupled with the lack of routine studies. The differential diagnosis in early stages was in this case the fibroadenoma, due to age and location, being excluded by its rapid growth in a short time, as well as imaging studies and tru-cut biopsy. The patient presented with adequate postoperative evolution, with good tolerance to diet and pain, with drains on his first postoperative day of 65 cc serohematic in the anterior drainage (# 1) and 55 cc also serohematic in the posterior (# 2), which were progressively decreased, so it was decided to discharge with drains on the third day of postoperative, with indications for monitoring and assessment of wide dorsal musculocutaneous flap. A private follow-up consultation was summoned on days 7 and 14 for wound assessment and drainage removal, surgical wounds and flap vascularity were explored, the latter in appropriate conditions, without changes in coloration, adequate temperature and capillary filling. No laboratory or imaging studies were requested at the consultation. Postoperative instructions were relative rest, compressive chest dressing, drainage quantification, normal diet, no heavy carrying, wound healings with antiseptic every 8 hours, and acetaminophen (500 mg VO every 8 hours for 7 days) for pain management and cephalexin (500 mg every 8 hours for 10 days) as antimicrobial prophylaxis. The clinical result was favorable and expected regarding the pathology and evolution, following the literature established in the NCCN guidelines for breast phyllodes tumor, the patient only reported having mild pain related to surgical wounds. No scale was used to assess quality of life. There was no increase in morbidity/mortality after 30 days of hospital discharge.
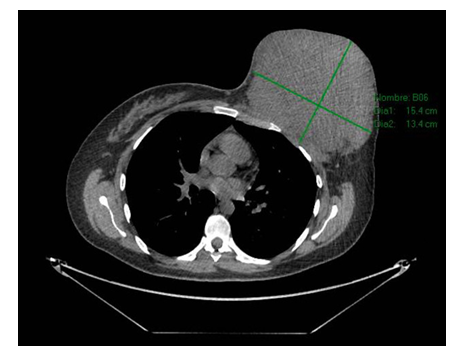
Figure 1: Simple thoracoabdominal CT scan in axial cut: Tumor is visualized in the left breast with dimensions of 15 x 13 x 18 cm, with lobed contours with extension to skin and left pectoralis major muscle.

Figure 2: Left breast with increase in volume of 15 x 13 cm and presence of ulcer at the level of the nipple accompanied by changes in skin coloration.

Figure 3: Block resection that included left breast tumor with margins of 1 cm, pectoralis major muscle and costal grill.

Figure 4: Broad dorsal musculocutaneous flap with adequate vascularity after its closure

Figure 5: Report of histopathology of the Phyllodes borderline type tumor in the left breast with epithelial component with proliferation of morphological characteristics "foliaceous".
Discussion
Unlike breast cancer, phyllodes tumors begin outside the lobes and ducts, specifically in connective tissue called the stroma, including ligaments, fatty tissue, lymph, and blood vessels. The above explains its clinical characteristic [5]. Most tumors form de novo, although there have been reports of progression from fibroadenomas to phyllodes tumors. [6]. One of the important points in our case report is the management that was carried out, being not common the level of high specialty in our environment (northern Mexico), from the participation of specialists (general surgeons, internal medicine, plastic surgery, nursing) to the complete use of resources. Another strong point is that excellent information is provided to the literature on a case with little or no visibility, especially in Mexico and Latin America. If we talk about weaknesses, our case may not provide a new management in terms of the diagnosis and treatment of this pathology, being its main contribution in epidemiology. As for the diagnosis, the most reliable is the histopathological with macroscopic observation (well circumscribed, firm and protruding tumors. The surface when cut can be pink or gray and presents as fleshy and mucous. Hemorrhages and necrosis may be observed [7]. Microscopically they have an intra-canalicular pattern of growth, with leaf-type projections extending to the dilated and elongated lumen. The epithelial component consists of epithelial and myoepithelial cells, stretched into arc-like clefts that overcome the stromal leaves [7]. The phyllodes tumor is divided into benign, malignant and borderline. Focusing on our case, the borderline type is one of the rarest types. The diagnosis can be complicated, due to the little information and well-defined characteristics of it. These tumors do not possess all the characteristics of malignancy, having frequent mitosis of 5-9 HPF (High-power fields) [8]. Moderate stromal cellularity, nuclear atypia, and focal infiltration are characteristic of both benign and borderline phyllodes tumors. It seems that mitotic activity is an important parameter for the diagnosis of borderline tumor [8]. The benign tumor consists of mild cellularity, mild atypia, mitosis < 5 HPF, no stromal growth and well-defined margins. The malignant, on the other hand, there is marked stromal cellularity and atypia, as well as infiltrative margin and mitosis > 10 HPF [9]. Speaking of treatment, a local excision with margins greater than 1 cm is usually curative, reducing the local risk of recurrence [10]. No differences have been shown between mastectomy and breast-conserving surgery, with the same survival rates and metastasis. Radiation therapy has been shown to reduce the risk of local recurrence, however adjuvant chemotherapy has shown no clinical benefit [11].
Patient perspective
The perspective of the patient regarding the clinical problem was that she did not expect it to be a case of phyllodes tumor, since in her family no one had presented something similar, that at first she felt a non-specific pain in her left breast, which she did not feel at first and so she did not give it importance believing that it could be related to her menstrual cycle, after this during its evolution was increasing the intensity of pain and the size of the tumor, for this reason they decided to go to the consultation with a general surgeon for its assessment, and with this same after the thoracoabdominal CT and biopsy (Trucut) the diagnosis was made, the patient after the surgical procedure reported a significant improvement in her general condition and pain, based on this, it is necessary to emphasize the importance of going to a routine and at the same time timely medical evaluation when presenting any type of pain located in the breast regardless of age, so in turn avoid long-term complications, said the patient and his family who are grateful for the management, evolution and well-being of the same.
Methods
This case report has been reported in line with the SCARE Criteria [12].
Conclusion
The knowledge of the possible appearance in our environment of the phyllodes tumor makes it essential when taking it into account in our differential diagnoses, knowing its characteristics, management and treatment can greatly help to consolidate in the literature better ways to safeguard the prognosis of patients with this pathology. We strongly invite our lectors to read the discussion as well as read accompanying literature to learn or remember the ideal management of these patients.
Sources of funding
This study did not receive any specific support from funding agencies, in the public, commercial or non-profit sector.
Conflict of interest
The authors declare that they have no conflict of interest in the writing of this manuscript.
Ethical considerations
Protection of people and animals: The authors state that no experiments have been carried out on humans or animals for this research.
Confidentiality of data: The authors state that they have followed their workplace protocols on the publication of patient data.
Right to privacy and informed consent
The authors declare that no patient data appears in this article. The patient was told about the publication of the case and the anonymity of his personal data, which referred to be in complete agreement, the consent was both verbal and written.
Authors contribution
Alejandro Flores Uribe: Patient care, clinical case, writing.
Jorge Alberto González Arévalo: Writing and translation.
Diego Bolaños Maya: Patient care, clinical case.
Eduardo Chávez Ornelas: Writing and translation.
Roberto Martínez Mejorada: Writing and translation.
References
- Reich H, McGlynn F, Decaprio J, et al. Laparoscopic excision of benign liver lesions. Obstet Gynecol 78 (1991): 956-958.
- Cherqui D, Laurent A, Tayar C, et al. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg 243 (2006): 499-506.
- Simillis C, Constantinides VA, Tekkis PP, et al. Laparoscopic versus open hepatic resections for benign and malignant neoplasms- a meta-analysis. Surgery 141 (2007): 203-211.
- Imura S, Shimada M, Utsunomiya T, et al. Current status of laparoscopic liver surgery in Japan: results of a multicenter Japanese experience. Surg Today 44 (2014): 1214-1219.
- Ban D, Kudo A, Ito H, et al. The difficulty of laparoscopic liver resection. Updates Surg 67 (2015): 123-128.
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 250 (2008): 825-830.
- Tranchart H, Di Giuro G, Lainas P, et al. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc 24 (2010):1170-1176.
- Belli G, Fantini C, D’Agostino A, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc 21 (2007): 2004-2011.
- Kaneko H, Takagi S, Otsuka Y, et al. Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg 189 (2005): 190-194.
- Lesurtel M, Cherqui M, Laurent A, et al. Laparoscopic versus open left lateral hepatic lobectomy: a case–control study. J Am Coll Surg 196 (2003): 236-242.
- Zhao L, Han J, Loeb S, et al. Thoracic complications of urologic laparoscopy: correlation between radiographic findings and clinical manifestations. J Endourol 22 (2008): 607-614.
- Murdock CM, Wolff AJ, Geem TV. Risk factors for hypercarbia, subcutaneous emphysema, pneumothorax, and pneumomediastinum during laparoscopy. Obstet Gynecol 95 (2005): 704-709.
- Craig JOC, Bromley LL, Williams R. Thoracotomy and the contralateral lung. A study of the changes occurring in the dependent and contralateral lung during and after thoracotomy in lateral decubitus. Thorax 17 (1962): 9-15.
- Goodman ZD. Grading and staging systems for inflammation and fibrosis in chronic liver diseases. J Hepatol 47 (2007): 598-607.
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240 (2004): 205-213.
- Di Giuro G, Lainas P, Franco D, et al. Laparoscopic left hepatectomy with prior vascular control. Surg Endosc 24 (2010): 697-699.
- Rehder K, Hatch DJ, Sessler AD, et al. The function of each lung of anesthetized and paralyzed man during mechanical ventilation. Anesthesiology 37 (1972): 16-26.
- Kaneko K, Milic-Emili J, Dolovich MB, et al. Regional distribution of ventilation and perfusion as a function of body position. J Appl Physiol 21 (1966): 767-777.
- Kazaryan AM, Marangos IP, Rosok BI, et al. Laparoscopic resection of colorectal liver metastases: surgical and long-term oncologic outcome. Ann Surg 252 (2010): 1005-1012.
- Castaing D, Vibert E, Ricca L, et al Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg 250 (2009): 849-855.
- Berard F, Gandon J. Postoperative wound infections: the influence of ultraviolet irradiation of the operating room and of various other factors. Ann Surg 160 (1964): 1-192.
- PHLS. Incidence of surgical wound infection in England and Wales: A report of the Public Health Laboratory Service. Lancet 2 (1960): 659-653.
- Nobili C, Marzano E, Oussoultzoglou E, et al, Multivariate analysis of risk factors for pulmonary complications after hepatic resection. Ann Surg 255 (2012): 540-550.
- Okabayashi T, Nishimori I, Yamashita K, et al. Risk factors and predictors for surgical site infection after hepatic resection. J Hosp Infect 73 (2009): 47-53.
